Spinal Trauma
advertisement

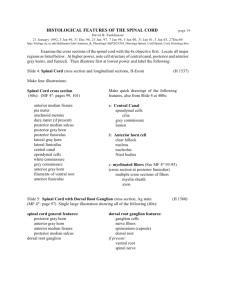
Spinal Trauma Outline • • • • • • Incidence Types Clinical signs Radiological signs Spinal shock Management Incidence • • • • • • • • 10 - 15 per million 18 - 35 years Male - 3:1 RTA 51% - cars Domestic 16% Industrial 11% Sports 16% - diving incidents Self harm 5% Types • • • • • Cervical 40% Thoracic 10% Lumbar 3% Dorso lumbar 35% Any 14% Anatomy • Spinal cord ends below lower border of L1 • Cauda equina is below L1 • Mid dorsal spinal cord & neural canal space are of same diameter hence prone for complete lesion • Mechanical injury - early ischaemia, cord edema cord necrosis • Neurological recovery unpredictable in cauda equina ie. peripheral nerves Cervical spine anatomy • Anterior column - Anterior longitudinal ligament+ Anterior annular ligament and anterior half of VB. • Middle column – Posterior long. Lig. + Posterior annular ligament +Posterior half of VB. • Posterior Column – Lig flavum + superior & Interspinous lig + intertransverse capsular lig + neural arch + pedicle & spinous process. Significance • Unstable if middle column + either Anterior or Posterior column is damaged • Rupture of interspinous ligament is : - associated with avulsion of spinous process - Unstable spine - Further flexion increases neurological injury Level of Spinal injury • Neurological level is at the most lowest segment with normal motor & sensory function • Difficult to determine : - as most muscle efferents receive fibres from more than one level - Closed cord lesions may extend over several cms. - Dermatomes have imprecise boundaries. Cord level • C2 – C7 = add +1 for cord level • T1 – T6 = add +2 • T7 – T9 = add +3 • T10 = L1, L2 level • T11 = L3, L4 level • L1 = sacro coccygeal segments Degrees of injury • Complete - flaccid paralysis + total loss of sensory & motor functions • Incomplete - mixed loss - Anterior sc syndrome - Posterior sc syndrome - Central cord syndrome - Brown sequard’s syndrome - Cauda equina syndrome Anterior spinal cord syndrome • Flexion rotational force to spine • Due to compression fracture of vertebral body or anterior dislocation • Anterior spinal artery compression • Loss of power, reduced pain and temperature below the lesion. Posterior cord syndrome • Hyperextension injuries • Posterior vertebral body fracture • Loss of proprioception and vibration sense • Severe ataxia Central cord syndrome • Older age with cervical spondylosis • Hyperextension with minor trauma • Cord is compressed by osteophytes from vertebral body against thick ligamentum flavum. • Damages the central cervical tract • UMN lesion to legs (spastic) • LMN to arms (flaccid paralysis) Brown sequards syndrome • Hemisection of the cord • Stab injury and lateral mass fractures • Uninjured side has good power but absent pinprick and temperature. • Spinothalamic tracts cross to opposite side of the cord three segments below. Types of bony injury • Flexion • Extension • Flexion with rotation • Compression Pathophysiology • Primary Neurological damage Direct trauma, haematoma & SCIWORA < 8yrs old In 4hrs - Infarction of white matter occurs In 8hrs - Infarction of grey matter and irreversible paralysis • Secondary damage Hypoxia Hypoperfusion Neurogenic shock Spinal shock Hypoxia • Lesions above C5 – damage to diaphragm leads to 20% reduction in vital capacity Rx Phrenic n. pacing • Lesions at D4-6 – reduces vital capacity if < 500ml patient is ventilated • Intercostal nerve paralysis • Atelectasis – poor cough • V/Q mismatch • Reduced compliance of lung – muscle fatigue. Neurogenic shock • • • • • • Lesions above D6 Minutes – hours (fall of catecholamines may take 24 hrs) Disruption of sympathetic outflow from D1 - L2 Unapposed vagal tone Peripheral vasodilatation Hypotension, Bradycardia & Hypothermia • BUT consider haemmorhagic shock if – injury below D6, other major injuries, hypotension with spinal fracture alone without neurological injury. Spinal shock • Transient physiological reflex depression of cord function – ‘concussion of spinal cord’ • Loss anal tone, reflexes, autonomic control within 24-72hr • Flaccid paralysis bladder & bowel and sustained Priapism • Lasts even days till reflex neural arcs below the level recovers. Assessment & Managemnt • • • • • • • • Failure to suspect leads to failure to detect injuries ABCDE – Logroll and remove the spinal board Look for markers of spinal injury Secondary survey Adequate Xray’s Emergency treatment Surgery Definitive care & rehab. Clinical features • Pain in the neck or back radiating due to nerve root irritation • Sensory disturbance distal to neurological level • Weakness or flaccid paralysis below the level Signs in an Unconcious patients • • • • Diaphragmatic breathing Neurological shock (Low BP & HR) Spinal shock - Flaccid areflexia Flexed upper limbs (loss of extensor innervation below C5) • Responds to pain above the clavicle only • Priapism – may be incomplete. Signs of spinal injury • Forehead wounds – think of hyperextension injury • Localized bruise • Deformities of spine - Gibbus, feel a step & Priapism • Beevors sign – tensing the abdomen umbilicus moves upwards in D10 lesions Prehospital transfer • • • • • • • • • • Awareness of the crew & by A&E staff Modified left lateral position at scene Kendrick or Russell’s extrication device Scoop stretcher slotted together around the patient Agitated patient left alone with hard collar Repeated assessment enroute Head down if they vomit Remove objects from clothes to avoid pressure sores Avoid opiates in high lesions Avoid oral suction in tetraplegics – vagal reflex Care in A&E • • • • • • • • • • Careful manual handling especially if unconcious Jaw thrust is safer Correct gross spinal deformities Call the anaesthetist if diaphragmatic paralysis or RR>35 Use flexible fibreoptic scopes in unstable fractures Ryles tube if abdominal distension causes respiratory probl Cathetrize to avoid overstretching of detrusor IV fluids – paralytic ileus in first 48hrs. Passive movements to rule out fractures Small iv doses of opiates Assessment • Document the level of injury • Rule out other injuries – DPL in abdominal injuries as there is paralytic ileus and absent peritioneal irritation. • Associated injuries in dorsal spine fracture are : - Renal injuries - Chest and Sternal injuries - Wide Mediatinum due to fracture haematoma. - Retroperitoneal injuries Radiology • Be thorough – Adequacy, Alignment,Bones, Cartilages and soft tissues and distances • SCIWORA in kids • Low threshold for xray in rheumatoid & Ankylosing spond • Flexion injury common in lower cervical spine • Extension injury in upper cervical Spine • Junction of mobile & fixed part are prone to injury eg. C7 T1 & D12 L1. Radiographs in spinal injuries • Lateral C spine views in diagnostic in 80% • Complete set of C spine xray are 90% diagnostic • CT of the c spine is 98% diagnostic • 22.5* logrolled view for better views of the facets • 45* view shows the intervertebral foramen & facets Normal Cervical Spine • Peg & lateral mass distance <2mm and symmetrical • Peg & arch of atlas distance <2mm in adults < 4mm in kids • Above C4 the width is <half of the VB width below C4 its equal to one VB width • Pseudosubluxation of C2 on C3 is normal in young kids& it disappears on extension • C1 and C2 interspinous space <10mm wide • Distance between occiput and atlas <5mm • Anterior compression of VB >40% suggest burst fracture Abnormal C spine • Unilateral facet dislocation < half of the vertebral body shifted on the lateral view • Bilateral facet dislocation > half shifted forwards • Wide interspinous gap is unstable (crush fracture or subluxation) suggestive of rupture of the posterior cervical ligament rupture and haematoma formation. • Severe flexion injury – fractures the anteroinferior margin of the vertebral body • Severe extension injury – fractures the anterosuperior margin of the VB. Emergency treatment • • • • • ABCDE Keep warm Treat if BP<80mmHg & HR <50bpm Spring loaded gardener wells calipers for traction H2 Antagonists & Heparin • Methylprednisolone 30mg/kg iv bolus over 15min immediately • 45minutes after the bolus a 5.4mg/kg/h infusion over 23 hrs in first 3 hours after the injury. • 5.4mg/kg/hr for 47hrs if 4 - 8hrs following the injury. Whiplash injury • Sudden hyperextension and flexion • Increasing neck pain for the first 24hours • Associated headache, pain radiating to both shoulders and paraesthesia in hands • Reduced lateral flexion • Anterior longitudinal ligaments are torn causes dysphagia • Forward flexion against resistance is painful • 90% are asymptomatic after 2years • 10% still have pain • Some still claim money hence the need for proper documentations.