Pediatric Safety - Austin Community College
advertisement

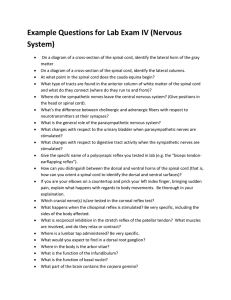
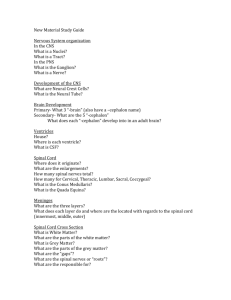
Traumatic Spinal Cord Injury Marnie Quick, RN, MSN, CNRN A. Pathophysiology/etiology Normal spinal cord as it relates to SCI Spinal cord begins at the foramen magnum in the cranium Cord ends at the L1L2 vertebra level Spinal nerves continue to the last sacral vertebra Normal protection of spinal cord from injury: Bones- vertebral column Protection of spinal cord from injury Disc between vertebra Internal and external ligaments Protection of Spinal Cord from Injury Meninges CSF in subarachnoid space allow for movement within spinal canal Normal spinal cord as relates SCI: Autonomic Nervous System & Cord ANS can be affected by SCI Sympathetic chains on both sides of the spinal column Parasympathic nervous system is the cranial-sacral branch Normal spinal cord: White tracks send messages to and from the brain Pyramidal- Voluntary movements Posterior column (Dorsal)- touch, proprioception, and vibration sense Lateral spinothalamic tract- pain and temperature sensation (only tract that crosses within the cord) Normal spinal cord: Reflex ark in center of the spinal cord Where sensory and motor nerves arise from cord Sensory fibers enter posterior Motor fibers leave from anterior Once outside cord join form spinal nerve Normal spinal cord: Dermatones: skin innervated by sensory nerves Normal spinal cord: Spinal cord level When referring to spinal cord level, it the reflex arc level not the vertebral or bone level. Note that the thoracic, lumbar & sacral reflex arcs are higher than were the spinal nerves actually leave through the opening of there respective vertebral bone Upper and Lower Motor Neurons Upper motor deficits results in spastic paralysis Lower motor deficits are flaccid paralysis and muscle atrophy Etiology of traumatic spinal cord injury MVA- most common cause Other: falls, violence, sport injuries Typically occurs from indirect injury from displaced vertebral bones compressing cord Frequently occurs with head injuries Less frequent cord torn/cut, as from direct trauma from knives or bullets Hemorrhage/edema occurs secondary in cord post injury, causing more damage to cord Extension of cord injury from cord edema can occur over 1st few days- watch the phrenic nerve! Initially SCI experience spinal shock- depression of all cord & ANS function below injury. Lasts from few min to wks Risk factors- male, 16-30 yr, risk taker 90% discharged home; 10% chronic care facility Events leading to spinal cord ischemia and hypoxia of 2nd injury Classification of SCI: 1. Mechanism of Spinal Cord Injury Mechanism of Injury SCI: Flexion (hyperflexion) Most common because of natural protection position. Generally cause neck to be unstable because stretching of ligaments Flexion with rotation can also occur Mechanism of SCI: Hyperextention Caused by chin hitting a surface area, such as dashboard or bathtub Usually causes central cord syndrome symptoms Mechanism of SCI: Compression Caused by force from above, as hit on head Or from below as landing on butt Usually affects the lumbar region Classification of SCI: 2. Level of skeletal injury Classification of spinal cord injury3. Level of Injury to the spinal cord Neurologic level of Injury Neurologic level or the lowest cord segment (reflex) or dermatone level functioning Such as C6; L4 SCI Prefix: Para-, quadSuffix:-paresis,-plegia Classification of SCI: Level of SCI Neurologic level Classification 4. Degree of completeness inj: Complete (transection) spinal cord inj After spinal shock: Motor deficits- spastic paralysis below level of injury Sensory- loss of all sensation perception Autonomic deficitsvasomotor failure (orthostatic hypotension, poikilothermic) and spastic bladder Classification of SCI: Incomplete spinal cord injury- what white tracks are working after spinal shock is over? Classification of SCI: Degree of completeness Incomplete spinal cord injury Incomplete spinal cord injury: Central cord Syndrome Injury to the center of the cord by edema and hemorrhage Weakness in both upper extremitieslegs are spared Varied loss of sensation Incomplete spinal cord injury: Anterior Cord Syndrome Injury to anterior cord Loss of voluntary motor (Pyramidal track) below Loss of pain and temperature perception Retains posterior column function Incomplete spinal cord injury: Brown-Sequard Syndrome Hemisection of cord Ipsilateral paralysis Ipsilateral superficial sensation, vibration and proprioception loss Contralateral loss of pain and temperature perception Classification of SCI: 5. American Spinal Injury Association Impairment Scale Clinical Manifestations & Complications Spinal Cord Injury Depends on extent and level of injury Higher cord injury more serious sequelae Resp: decrease chest expansion (intercostals); decrease cough reflex & Vital capacity; diaphragm function controlled by phrenic nerve (C3-5); may need mechanical ventilation Clinical Manifestations & Complications Spinal Cord Injury continued Cardio: dysrhythmias; bradycardia; loss SNS control bl vessels spinal shock; loss of sympathetic nervous system control over blood vessels (vasomotor control)- dec venous return, orthostatic hypotension; dec CO; poikilothermic (takes on temp of room) GU: upper/lower motor bladder; impotence; sexual dysfunction GI: stress ulcers; paralytic ileus; bowelimpaction & incontinence Clinical Manifestations & Complications Spinal Cord Injury continued Skin: pressure ulcers can lead to infection/sepsis Thermoregulation: poikilothermic (take on temp of environment) Unable to sweat or shiver below level of SCI. Occurs due to SNS interruption; Degree depends level inj Metabolic needs: Nasogastric suctioning may lead to metabolic alkalosis (Paralytic ileus). Nutritional needs to deep body wt and prevent complications- need positive nitrogen, highprotein diet Peripheral vascular: DVT; pulmonary embolism Clinical Manifestations & Complications Spinal Cord Injury continued Neuro: pain at the level of injury; sensory loss; upper/lower motor deficits; autonomic dysreflexia; spinal shock Musculoskeletal: joint contractures; bone demineralization; osteoporosis; muscle spasms; muscle atrophy; pathologic fractures; para/tetra/Quad; plegia/paresis Spinal shock: result of inflammatory process in cord after injury, causing depression of cord & ANS function below level of injury. Approx 50% develop Motor loss- flaccid paralysis below level injury Sensory loss- loss touch, pressure, temperature pain and proprioception perception below injury Sympathetic NS loss results in parasympathic dominance with vasomotor failure Neurogenic shock, bradycardia, orthostatic hypotension and poor temperature control (poikilothermic- takes on temp of environment) Parasympathetic NS loss of the S 2,3,4 reflex arks results in flaccid bladder Distributive shock symptoms Spinal shock lasts from few minutes to wks How do you know spinal shock is over? Clonus is one of the first signs Hyperreflexia of foot Test by flexing leg at knee & quickly dorsiflex the foot Rhythmic oscillations of foot against hand Common manifestations&complications: Functional Goals for Spinal Cord Injury C1-3 usually fatal- loss phrenic inervation; ventilator dependent; no B/B control; spastic paralysis; electric w/c with chin/mouth control C6- weak grasp; has shoulder/biceps to transfer & push w/c; can use assistive devices; dec resp reserve; loss vasomotor; no bowel /bladder control. T1-6- full use of upper extremity; transfer; drive car with hand controls and do ADL’s; dec trunk stability; no bowel/bladder control C6 SCI using a transfer board Collaborative Care for SCI: Diagnostic tests Comprehensive neuro exam X-ray of spinal column CT/MRI Blood gases Collaborative Care: Emergency care at scene, ER & ICU Initial goals- sustain life and prevent further cord damage Transport with cervical collar Assess ABC’s; O2; tracheotomy/vent IV for life line- to give meds NG to suction Foley- flaccid bladder Collaborative Care: Stabilization & immobilization with traction Collaborative Care: Gardner-Wells tongs Collaborative Care: External traction Halo device For patients who have few motor deficits Experience less immobility complications Collaborative Care: Casts; splints; collars; braces Collaborative Care: Special Beds for SCI To decrease immobility complications Rotorest bed provides for lateral rotation 23 hrs a day Collaborative Care: Surgery for SCI Manipulation to correct dislocation or to unlock vertebrae Decompression laminectomy Spinal fusion Wiring or rods to hold vertebrae together Collaborative Care: Drug Therapy IV metylprednisone (Solu-Medrol) within 8 hrs to decrease cord edema/inflammation Medications to control or to prevent complications SCI and immobility: Vasopressors treat bradycardia or hypotension Histamine H2 blockers to prevent stress ulcers Anticoagulants- immobility Stool softeners Antispastomotics BP meds (Procardia) if sym persists with autonomic dysreflexia Nursing Assessment Specific to SCI Lewis 1553 Table 61-6 Subjective data: Important health info- health history; cause of SCI Function health patterns-activity; perceptual;coping Objective data: By systems LOC/pupils- R/O head injury VS- bradycardia Motor & Sensory Clonus & spontaneous movement Nursing assessment: Motor assessment Movement, strength and symmetry Hand grips Flex and extend arm at elbow- with and without resistance Nursing assessment: Motor assessment lower extremity Flex and extend leg at knee with and without resistance Planter and dorsi flexion of foot Nursing assessment: Motor assessment- Clonus Clonus- hyperreflexia Flex knee and quickly dorsiflex the foot with your hand If has return of reflex function the foot will have repetitive movements against you hand Spinal shock is over Nursing assessment: Sensory assessment With the sharp and dull ends of a Q-tip or paperclip have the individual, with their eyes closed identify Use the dermatome as reference to identify level C6 thumb; T4 nipple; T10 naval Pertinent Nsg problems/intervention SCI Lewis p.1554-5 NCP: 61-1 Impaired gas exchange Decrease CO Impaired skin integrity Constipation Impaired urinary elimination Risk for autonomic dysreflexia Ineffective coping Interrupted family process Pertinent nursing problems/interventions Acute intervention: Immobilization Log roll as a single unit; provide assistance as needed to keep alignment; teach patient Care traction, special beds, collars, splints, braces, assistive devices for ADL’s Flaccid paralysis- use high top tennis shoes or splints to prevent contractures. Remove at least every 2 hrs for ROM (active ROM best) Spastic paralysis- assess for clonus Prevent spasms by avoiding; sudden movements or jarring of the bed; internal stimulus (full bladder/skin breakdown; use of footboard; staying in one position too long; fatigue Treat spasms by decreasing causes; hot or cold packs; passive stretching; antispasmotic medications Assess skin break down & thrombophlebitis; remove TED hose at least every shift Pertinent nursing problems/interventions Respiratory Phrenic nerve; thoracic and intercstal nerves; abdominal muscles Monitor vital capacity, respiratory effort, ABG’s, O2 saturation, need for ventilator assistance Assess for signs of impending extension of SCI up cord to phrenic nerve level (C3-5) Quad cough (assistive cough) as needed Pertinent nursing problems/interventions Acute intervention: Cardio/nutrition Cardiovascular instablity Prevent/treat orthostatic hypotension Abdominal binder, calf compressors, TED hose when individual gets up Assess BP, especially when rising Assist Physical Therapy with tilt table as individual gradually gets use to being in an upright position Fluid and nutritional maintenance NG to suction in acute; monitor F&E High protein/high calorie diet Pertinent nursing problems/interventions Acute intervention: Bladder Bladder reflex ark- sacral 2,3,4 Flaccid bladder (lower motor neuron lesion) has no reflex from S2,3,4. Have automatic empting of bladder. Urine fills the bladder and dribbles out. Need foley or freq intermittent self catherization Spastic bladder (upper motor neuron lesion) has reflex ark, but no connection to or from brain. Reflex fires at will. Bladder training- trigger points to stimulate empting; self catherization Upper/lower motor bladder-Website http://www.rnceus.com/course_frame.asp?exam_id=56&directory=uro 4. Autonomic Dysreflexia SCI above T6 Results in loss of normal compensatory mechanisms when sympathetic nervous system is stimulated Life threatening- if goes unchecked BP can result in cerebral hemorrhage Autonomic Dysreflexia- assess Vasodilatation symptoms above SCI Vasoconstriction symptoms below SCI The cause of SNS stimulation Autonomic Dysreflexia- treatment Elevate head of bed- causes orthostatic hypotension Identify cause/alleviate- if full bladder- cath; if skin- remove pressure, if full bowel- empty, etc Remove support hose/abdominal binder Monitor blood pressure- can get > 300 S Give PRN medication to lower BP If above not effective– call physician Use bladder scan to see amount of urine in bladder Goal- residual <100ml/20% bladder capacity Some individuals may need suprapubic catheter Assess effectiveness of medication Urecholine to stimulate the parasympathic S 2,3,4 reflex to fire and cause bladder contraction Urinary antiseptic Pertinent nursing problems/interventions other Bowels Temperature control Stress ulcer Sensory deprivation Reflexes- may see hyperreflexia as return of motor function Rehabilitation and home care: Resp; neurogenic bladder/bowel; skin care; sexuality; grief/depression Bowel Bowel rely more on bulk than on nerves Stimulate bowels at the same time each day. Best after a meal when normal peristalsis occurs Individual may progress from ducolax suppository to glycerin then to gloved finger for digital stimulation Assess bowel sounds prior to giving food for the first time– paralytic illus! Sexual dysfunction Assess readiness/knowledge/your ability Male sexual function- reflexogenic (S2,3,4) erections; psychogenic erections (psychological stimulation) Ejaculation/fertility may be affected Female- hormones more than nerves regarding fertility. C-section because of chance for autonomic dysreflexia during labor. Lack of sensation/movement affects sexual performance Suggestions: empty bladder before sex; withhold fluids and antispasmodics; certain positions may increase spasms; explore new erogenous zones; penile implants Low self-esteem Assess thoughts on ‘quality of life’; body image; role changes Physical and psychological support Most common SCI is 15-30 yeas old and generally a risk taker– this greatly affects their perception of life and rehabilitation progress Home care Assess psychological, physical resources, need for rehabilitation (in-house or outpatient); need for community resources Home evaluation