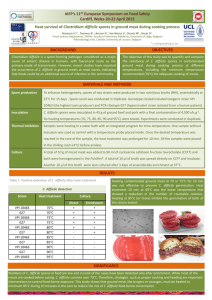
Evaluation of UV Light Technology and CDI
advertisement

Evaluation of Discharge Room Cleaning using UV Technology: Focus on Clostridium difficile Alison Gibson D.O. Fellow, Pediatric Infectious Diseases University of Michigan Disclosures • This study was funded by a $12,000 award from the Patient Safety Committee of University of Michigan Health System • Both of the UV devices used in our study were provided to the institution by Xenex and iPT during the outcomes study, the Xenex device was then rented to complete the environmental culturing study • I have no other conflicts of interest or relationships with industry This is a confidential Quality Improvement and Assurance/peer review document of the University of Michigan Hospitals and Health Centers. Unauthorized disclosure or duplication is absolutely prohibited. This document is protected from disclosure pursuant to the provisions of MCL 333.20175; MCL 333.21515; MCL 331.531; MCL 331.533 or such other statutes that may be applicable. Objectives • How does UV work? • What literature do we have to support the use of UV? • Why did UofM choose to pursue UV and how did we utilize it? • Outcomes study • Environmental culturing study • Future Directions Automated Room Disinfection • Ultraviolet (UV) – UV-C (mercury bulbs) – PPX-UV (pulsed xenon bulbs) • Hydrogen peroxide vapor (HPV) • Neither of these technologies replace manual cleaning, and therefore both add additional time before room turnover Tru-D Lumalier (UV-C) Xenex (PPX-UV) Bioquell (HPV) http://www.hpnonline.com/inside/201109/1109-CS-RoomDisinfection.html http://bionews-tx.com/wpcontent/uploads/2013/04/xenex-device.jpg http://www.bioquell.com/en-us/markets/product-selector/bioquell-q10/ UV – Science • Breaks DNA bonds by inducing pyrimidine or thymine dimers (1,2,3,4,5) http://mashable.com/category/dna/ UV – Safety • No health or safety concerns returning to room • Direct prolonged light exposure can cause temporary corneal and conjunctival irritation (1,2,3,4,5) http://www.clinicaladvisor.com/what-to-do-whenthe-eyes-have-it/article/121816/ UV – Utilization • Easy to use, no room modifications • Shorter treatment time (depending on device and room size, compared to HPV) • Expenses associated with machine and bulb replacement • Safe with electronic room devices and other room materials (1,2,3,4,5) UV - Efficacy • 2-4 log10 reduction of spores • May allow resistant organisms to develop due to sublethal dose • Efficacy dependent on intensity of emitted light (old bulb vs. new bulb), exposure time, placement/obstructions, air movement • Less effective out of direct line of sight • Less effective further from the source (cannot use in large areas) (1,2,3,4,5) UV-C vs. PPX-UV UV-C (Ex.Tru-D Lumalier, iPT) PPX-UV (Ex. Xenex) • 200-280nm, Tru-D emits at 254nm • Breaks DNA bonds but not at the ideal wavelength (265nm), so occurs more slowly • Continuous dose at germicidal wavelength • Longer treatment times (34100min per cycle) (1,2,4,5) • 200-320nm broad spectrum • More efficient (faster) because more broad spectrum • Additional benefits of photosplitting, photohydration, and photocrosslinking, all of which contributes to faster treatment times • Pulse dose at broad wavelength including germicidal range • Shorter treatment times (5-10 min per cycle) (1,2,5) Published UV Data Study Device Cleaning Method Culture Method Results Anderson et al. (2013)6 Tru-D Lumalier UV Rodac touch plates 1.16 log reduction in colony counts Boyce et al. (2011)7 Tru-D Lumalier UV Pre-inoculated plates 1.7-2.9 log reduction in colony counts Sitzlar et al. (2013)8 Tru-D Lumalier Routine cleaning Surface followed by UV swabbing Reduction in positive cultures from 57% to 35% Levin et al. (2013)9 PPX-UV Bleach followed by UV Reduction in HO-CDI rate from 9.46 to 4.45/10,000 PDs None Why did we choose to pursue use of a UV system? • C. difficile rates are above the national and state averages • Tried to implement daily bleach cleans of hightouch surfaces • Appeal of a device less vulnerable to human error UV light trials • Trialed two different lights [PPX-UV (Xenex) and UV-C (iPT)] on three units each and followed HO-CDI rates – Trial 1 was 5 months – Trial 2 was 10 months UV Utilization • Adjunct to bleach for discharge room cleans • 2 - 4 cycles per room, 5-10 min each plus set up and take down • Device was operated by EVS personnel trained by our institution • Spot cleaning of public areas/work areas (family rooms, bathrooms, etc.) http://bionews-tx.com/news/2014/10/08/xenex-uv-emitting-room-disinfectionrobots-ready-to-tackle-ebola-and-other-contamination/ iPT (UV-C) http://www.infectionpreventiontechnologies.com/irsModel320 0m.php Xenex (PPX-UV) http://bionews-tx.com/wp-content/uploads/2013/04/xenex-device.jpg Healthcare Facility Onset C. difficile Rates During UV-C Trial C. difficile Rate (Cases/10,000 Patient-Days) 30 25 20 UV Trial 15 5 mths prior to trial (p = .3360) Same time period previous year (p = .3793) 10 5 *None of the units showed a statistically significant change in C. difficile rate, with the exception of 8DNS which showed a significantly worse rate when compared to the previous 5 months 0 5D 8C 8DNS Hospital Unit Total Healthcare Facility Onset C. difficle Rates During PPX-UV Trial C. difficile rate (cases/10,000 patient-days) 35 30 25 20 UV Trial 10 mths prior to trial (p = .9576) 15 Same time period previous year (p = .5738) 10 5 *no individual units reached a statistically significant difference in C. difficile rate 0 5B 6D 4D Hospital Unit Total UV Utilization Barriers to UV Utilization • Prolonged room turnover time • Only can be used at discharge in single occupant rooms • Burden of initial investment to provide sufficient machines to cover all C.diff or contact isolation or every discharge • Burden of training and maintaining additional EVS personnel to run the devices Why we chose to pursue this study • No improvement in C. difficile outcomes after utilizing UV technology – Were we utilizing the device correctly? • Were enough rooms being treated? – Was it actually decreasing environmental C. difficile burden? – Is environmental contamination at discharge our primary issue? The Study Our goal was to compare the effectiveness of manual cleaning with quaternary ammonium cleaner (Virex), manual cleaning with bleach, and PPX-UV cleaning both separately and in combination Obtained cultures from confirmed C. difficile positive rooms at discharge and throughout the cleaning process • • • • • • • • • • Bed rail Tray table Remote Toilet seat Toilet rim Sink faucet Light switch Keyboard Soiled Room Culture #1 Bleach Clean Culture #2 PPX-UV Clean Culture #3 Ready for Admission Soiled Room Culture #1 QA Clean Culture #2 PPX-UV Clean Culture #3 Bleach Clean Technicalities of swabbing and culturing • Sites were swabbed using pre-moistened sterile swabs (EnviroMax Plus) • Swabs were inoculated in enrichment broth (TCCFB) and incubated anaerobically for 24-48 hours • Broth was plated on selective media (CCFA-HT) and incubated anaerobically for 24-48 hours • Multiple colonies which were morphologically similar to/consistent with C.difficile were selected from each plate for PCR • PCR was used to detect toxin genes tcdA, tcdB, cdtA/cdtB • Representative isolates from each room were PCR ribotyped C. difficile Reduction with Bleach Followed by PPX-UV C. difficile Reduction with QA Followed By PPX-UV Conclusions • Bleach effectively eradicated C. difficile from multiple surfaces (p = .011) • PPX-UV light could not show an additive benefit when utilized after bleach cleaning (p = .343) • Manual cleaning with a QA product followed by PPXUV did reduce positive C. difficile cultures (p = .008) • Manual cleaning with a QA product followed by PPXUV is possibly not as effective for C. difficile eradication as bleach alone (p = .063) In the Meantime… • Nerandzic et al. (2015): – Xenex (PPX-UV) device and Tru-D Lumalier (UV-C) device – C. diff, MRSA, and VRE from pre-inoculated plates • Pathogen load did not impact killing, but distance from source did • C. diff at 4ft was only 0.5 log10 reduction with PPX-UV • UV-C was superior to PPX-UV for reduction of all 3 organisms with the same concentrations of organisms and distance from source (1 log10 for C. diff) – Room contamination • Tested PPX-UV alone and bleach + PPX-UV • Saw statistically significant reductions in culture positivity with PPX-UV, but not with bleach + PPX-UV, and did not assess for statistically significant difference between the two methods (10) In the Meantime… • Ghantoji et al. (2015): – Xenex PPX-UV device – Environmental cultures were collected before and after environmental cleaning with activated hydrogen peroxide followed by bleach (26/74 18/74) – And with activated hydrogen peroxide followed by PPX-UV (29/70 16/70) – No statistically significant difference in C. difficile positive cultures, z = 0.058 (11) Comparing Our Study Positive cultures pre- Positive cultures post- Study bleach (%) bleach (%) Gibson et al. 17/80 (21%) 1/80 (1%) Ghantoji et al.11 26/74 (35%) 18/74 (24%)a Nerandzic et al. 10 22/113 (19%) 9/113 (8%)b aCultures bCultures were obtained pre- and post- combination of activated hydrogen peroxide followed by bleach were obtained pre- and post- combination of standard clean including bleach followed by PPX-UV Remaining Questions • Is environmental contamination at discharge a primary contributor to C. difficile transmission at our institution? • Does UV-C/PPX-UV have a place in an infection prevention program? • What amount of bacterial environmental burden is permissible? Future Directions When an excessive number of cases occur on a unit (5 in a rolling 4 week period), multi-pronged approach including: bleach cleaning ATP assessment contact precautions re-enforcement and monitoring Possible utilization of hydrogen peroxide vapor (Bioquell) Focusing on other aspects of C. difficile prevention besides the terminal clean Thanks • Patient Safety Committee of the University of Michigan Health System • The Young Lab – Kavitha Santhosh – Vincent Young MD, PhD – Krishna Rao MD • Infection Prevention – Amanda Valyko MPH, CIC – Laraine Washer MD – Terri Stillwell MD, MPH References • • • • • • • • • • • 1. Barbut F. “How to eradicate Clostridium difficile from the environment.” J Hosp Infect. 2015 Jan 7. pii: S01956701(15)00005-5. 2. Otter JA,Yezli S, Perl TM, et al. “The role of ‘no-touch’ automated room disinfection systems in infection prevention and control.” J Hosp Infect. 2013 Jan;83(1):1-13. 3. Weber DJ, Anderson D, Rutala WA. “The role of the surface environment in healthcare-associated infections.” Curr Opin Infect Dis. 2013 Aug;26(4):338-44. 4. Rutala WA, Weber DJ. “Disinfectants used for environmental disinfection and new room decontamination technology.” Am J Infect Control. 2013 May;41(5 Suppl):S36-41. 5. Chemaly RF, Simmons S, Dale C, et al. “The role of the healthcare environment in the spread of multidrug-resistant organisms: update on current best practices for containment.” Ther Adv Infect Dis. 2014 Jun;2(3-4):79-90. 6. Anderson DJ, Gergen MF, Smathers E, et al. “Decontamination of targeted pathogens from patient rooms using an automated ultraviolet-C-emitting device.” Infect Control Hosp Epidemiol. 2013 May;34(5):466-71. 7. Boyce JM, Havill NL, Moore BA. “Terminal decontamination of patient rooms using an automated mobile UV light unit.” Infect Control Hosp Epidemiol. 2011 Aug;32(8):737-42. 8. Sitzlar B, Deshpande A, Fertelli D, et al. “An environmental disinfection odyssey: evaluation of sequential interventions to improve disinfection of Clostridium difficile isolation rooms.” Infect Control Hosp Epidemiol. 2013 May;34(5):459-65. 9. Levin J, Riley LS, Parrish C, et al. “The effect of portable pulsed xenon ultraviolet light after terminal cleaning on hospitalassociated Clostridium difficile infection in a community hospital.” Am J Infect Control. 2013 Aug;41(8):746-8. 10. Nerandzic MM, Thota P, Sankar T, et al. “Evaluation of a pulsed xenon ultraviolet disinfection system for reduction of healthcare-associated pathogens in hospital rooms.” Infect Control Hosp Epidemiol. 2015 Feb;36(2):192-7. 11. Ghantoji SS, Stibich M, Stachowiak J, et al. “Non-inferiority of pulsed xenon UV light versus bleach for reducing environmental Clostridium difficile contamination on high-touch surfaces in Clostridium difficile infection isolation rooms.” J Med Microbiol. 2015 Feb;64(Pt 2):191-4.