Seizure
advertisement

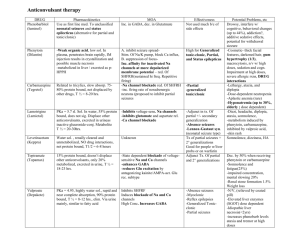
Pharmacology of Antiepileptic Drugs Basic Mechanisms Underlying Seizures and Epilepsy Seizure: the clinical manifestation of an abnormal and excessive excitation and synchronization of a population of cortical neurons Epilepsy: a disease characterized by spontaneous recurrent seizures Epileptogenesis: sequence of events that converts a normal neuronal network into an epileptic network Partial Seizures localized onset can be determined Simple Complex Secondary generalized Simple Partial Seizure • Focal with minimal spread of abnormal discharge • normal consciousness and awareness are maintained Complex Partial Seizures Local onset, then spreads Impaired consciousness Clinical manifestations vary with site of origin and degree of spread – Presence and nature of aura – Automatisms – Other motor activity Temporal lobe epilepsy most common Secondarily Generalized Seizures Begins focally, with or without focal neurological symptoms Variable symmetry, intensity, and duration of tonic (stiffening) and clonic (jerking) phases Typical duration up to 1-2 minutes Postictal confusion and somnolence Generalized Seizures In generalized seizures, both hemispheres are widely involved from the outset. Manifestations of the seizure are determined by the cortical site at which the seizure arises. Present in 40% of all epileptic Syndromes. Generalized seizures • Absence seizures (Petit mal): sudden onset and abrupt cessation; brief duration, consciousness is altered; attack may be associated with mild clonic jerking of the eyelids or extremities, postural tone changes, autonomic phenomena and automatisms (difficult diagnosis from partial); characteristic 2.5-3.5 Hz spike-and wave pattern • Myoclonic seizures: myoclonic jerking is seen in a wide variety of seizures but when this is the major seizure type it is treated differently to some extent from partial leading to generalized Generalized Seizures (cont) • Atonic seizures: sudden loss of postural tone; most often in children but may be seen in adults • Tonic-clonic seizures (grand mal): major convulsions with rigidity (tonic) and jerking (clonic), this slows over 60-120 sec followed by stuporous state (post-ictal depression) Generalized Tonic-Clonic Seizures • Recruitment of neurons throughout the cortex • • Major convulsions, usually with two phases: 1) Tonic phase: muscles will suddenly tense up, causing the person to fall to the ground if they are standing. 2) Clonic phase: muscles will start to contract and relax rapidly, causing convulsions • • • • • • Convulsions: motor manifestations may or may not be present during seizures excessive neuronal discharge Convulsions appear in Simple Partial and Complex Partial Seizures if the focal neuronal discharge includes motor centers; they occur in all Generalized Tonic-Clonic Seizures regardless of the site of origin. Atonic and absence Seizures are non-convulsive Video http://www.youtube.com/watch?v=frWcJJkXQFM Status Epilepticus • More than 30 minutes of continuous seizure activity • Two or more sequential seizures spanning this period without full recovery between seizures • Medical emergency Antiepileptic Drug A drug which decreases the frequency and/or severity of seizures in people with epilepsy Treats the symptom of seizures, not the underlying epileptic condition Goal—maximize quality of life by minimizing seizures and adverse drug effects Currently no “anti-epileptogenic” drugs available Therapy Has Improved Significantly • “Give the sick person some blood from a pregnant donkey to drink; or steep linen in it, dry it, pour alcohol onto it and administer this”. – Formey, Versuch einer medizinischen Topographie von Berlin 1796, p. 193 Current Pharmacotherapy • Just under 60% of all people with epilepsy can become seizure free with drug therapy • In another 20% the seizures can be drastically reduced • ~ 20% epileptic patients, seizures are refractory to currently available AEDs Choosing Antiepileptic Drugs Seizure type Epilepsy syndrome Pharmacokinetic profile Interactions/other medical conditions Efficacy Expected adverse effects Cost General Facts About AEDs • Good oral absorption and bioavailability • Most metabolized in liver but some excreted unchanged in kidneys • Classic AEDs generally have more severe CNS sedation than newer drugs (except ethosuximide) • Because of overlapping mechanisms of action, best drug can be chosen based on minimizing side effects in addition to efficacy Classification of AEDs Classical • • • • • • • Phenytoin Phenobarbital Primidone Carbamazepine Ethosuximide Valproate (valproic acid) Trimethadione (not currently in use) Newer • • • • • • • • • Lamotrigine Felbamate Topiramate Gabapentin/Pregabalin Tiagabine Vigabatrin Oxycarbazepine Levetiracetam Fosphenytoin Side effect issues • • • • • • • • Sedation - especially with barbiturates Cosmetic - phenytoin Weight gain – valproic acid, gabapentin Weight loss - topiramate Reproductive function – valproic acid Cognitive - topiramate Behavioral – felbamate, leviteracetam Allergic - many Cellular Mechanisms of Seizure Generation emedicine.com Targets for AEDs • Increase inhibitory neurotransmitter system— GABA • Decrease excitatory neurotransmitter system— glutamate • Block voltage-gated inward positive currents— Na+ or Ca++ • Increase outward positive current—K+ • Many AEDs pleiotropic—act via multiple mechanisms Epilepsy—Glutamate The brain’s major excitatory neurotransmitter Two groups of glutamate receptors – Ionotropic—fast synaptic transmission • NMDA, AMPA, kainate • Gated Ca++ and Gated Na+ channels – Metabotropic—slow synaptic transmission • Regulation of second messengers (cAMP and Inositol) • Modulation of synaptic activity Modulation of glutamate receptors – Glycine, polyamine sites, Zinc, redox site Epilepsy—Glutamate Glutamate Receptors as AED Targets • NMDA receptor sites as targets – Ketamine, phencyclidine, dizocilpine block channel and have anticonvulsant properties but also dissociative and/or hallucinogenic properties; open channel blockers. • AMPA receptor sites as targets – Since it is the “workhorse” receptor can anticipate major sedative effects Felbamate • Antagonizes the glycine site on the NMDA receptor and blocks Na+ channels* • Very potent AED lacking sedative effect (unlike nearly all other AEDs) • Associated with rare but fatal aplastic anemia, hence is restricted for use only in extreme refractory epilepsy Topiramate • Acts on AMPA receptors, blocking the glutamate binding site, but also blocks kainate receptors and Na+ channels, and enhances GABA currents (highly pleiotropic*) • Used for partial seizures, as an adjunct for absence and tonic-clonic seizures (add-on or alternative to phenytoin) • Very long half-life (20h) Epilepsy—GABA Major inhibitory neurotransmitter in the CNS Two types of receptors – GABAA—post-synaptic, specific recognition sites, CI- channel – GABAB —presynaptic autoreceptors, also postsynaptic, mediated by K+ currents GABAA Receptor Clonazapam • -Benzodiazepine used for absence seizures (and sometimes myoclonic): “fourth-line AED” • -Most specific AED among benzodiazepines, appearing to be selective for GABAA activation in the reticular formation leading to inactivation of T-type Ca2+ channels, hence its useful for absence seizures • -Sedating; May lose effectiveness due to development of tolerance (≤6 months) Lorazapam and Diazepam • Benzodiazepines used as first-line treatment for status epilepticus (delivered IV – fast acting) • Sedating Phenobarbital – Barbiturate used for partial seizures, especially in neonates. Oldest of the currently used AEDs – Very strong sedation; Cognitive impairment; Behavioral changes – Very long half-life (up to ~5days); #Induces P450 – Tolerance may arise; Risk of dependence – Primidone, another barbiturate metabolized to Phenobarbital, and Phenobarbital are now seldom used in initial therapy, owing to side-effects AEDs That Act Primarily on GABA Tiagabine – Interferes with GABA re-uptake Vigabatrin (not currently available in US) – elevates GABA levels by irreversibly inhibiting its main catabolic enzyme, GABAtransaminase Na+ Channels as AED Targets • Neurons fire at high frequencies during seizures • Action potential generation is dependent on Na+ channels • Use-dependent or time-dependent Na+ channel blockers reduce high frequency firing without affecting physiological firing Anticonvulsants: Mechanisms of Action Voltage-gated sodium channel Open Inactivated Na+ Na+ X I Na+ Carbamazepine Phenytoin A = activation gate I = inactivation gate McNamara JO. Goodman & Gilman’s. 9th ed. 1996:461-486. I Na+ Lamotrigine Valproate AEDs That Act Primarily on Na+ Channels Phenytoin, Carbamazepine – Block voltage-dependent sodium channels at high firing frequencies—use dependent Oxcarbazepine – Blocks voltage-dependent sodium channels at high firing frequencies – Also effects K+ channels Zonisamide – Blocks voltage-dependent sodium channels and T-type calcium channels Phenytoin • First-line for partial seizures; some use for tonicclonic seizures • Highly bound to plasma proteins – displaced by Valproate; #Induces P450 resulting in increase in its own metabolism, but its metabolism is also increased by alcohol, diazepam • Sedating • Fosphenytoin: Prodrug for Phenytoin, used for IM injection Carbamazapine • A tricyclic antidepressant used for partial seizures; some use in tonic-clonic seizures • #Induces P450 resulting in increase in its own metabolism; • Sedating; Agranulocytosis and Aplastic anemia (elderly); Leukopenia (10% of patients); Hyponatremia; Nausea and visual disturbances Oxcarbazapine • Newer drug, closely related to Carbamazapine, approved for monotherapy, or add-on therapy in partial seizures • May also augment K+ channels* • Some #induction of P450 but much less than that seen with Carbamazapine • Sedating but otherwise less toxic than Carbamazapine Zonisamide • Used as add-on therapy for partial and generalized seizures • -Also blocks T-type Ca2+ channels* • -Very long half-life (1-3days) Lamotrigine • Add-on therapy, or monotherapy for refractory partial seizures • Also inhibits glutamate release and (perhaps) Ca2+ channels (=pleiotropic*) • Metabolism affected by Valproate, Carbamazapine, Phenobarbital, Phenytoin • Less sedating than other AEDs; (Severe dermatitis in 1-2% of pediatric patients) Ca2+ Channels as Targets • General Ca2+ channel blockers have not proven to be effective AEDs. • Absence seizures are caused by oscillations between thalamus and cortex that are generated in thalamus by T-type (transient) Ca2+ currents Ethosuximide • Acts specifically on T-type channels in thalamus, and is very effective against absence seizures. • Long half-life (~40h) • Causes GI disturbances; Less sedating than other AEDs Gabapentin and its second generation derivative Pregabalin • -Act specifically on calcium channel subunits called a2d1. It is unclear how this action leads to their antiepileptic effects, but inhibition of neurotransmitter release may be one mechanism • -Used in add-on therapy for partial seizures and tonic-clonic seizures • -Less sedating than classic AEDs What about K+ channels? • K+ channels have important inhibitory control over neuronal firing in CNS—repolarizes membrane to end action potentials • K+ channel agonists would decrease hyperexcitability in brain • So far, the only AED with known actions on K+ channels is valproate • Retiagabine is a novel AED in clinical trials that acts on a specific type of voltage-dependent K+ channel (M-channel) Valproate (Valproic Acid) • First-line for generalized seizures, also used for partial seizures • Also blocks Na+ channels and enhances GABAergic transmission (highly pleiotropic*) • Highly bound to plasma proteins; #Inhibits P450 • CNS depressant; GI disturbances; hair loss; weight gain; teratogenic; (rare: hepatotoxic) Regulation of Neurotransmitter release • Several AED have actions that result in the regulation of neurotransmitter release from the presynaptic terminal, such as lamotrigine, in addition to their noted action on ion channels or receptors. • Levetiracetam appears to have as its primary action the regulation of neurotransmitter release by binding to the synaptic vesicle protein SV2A: Levetiracetam • -Add-on therapy for partial seizures • -Short half-life (6-8h) • -CNS depression Pleiotropic AEDs • Many AEDs act on multiple targets, increasing their efficacy • Felbamate, lamotrigine, topirmate, valproate Drug Interactions • Many AEDs are notable inducers of cytochrome P450 enzymes and a few are inhibitors. • Of the classic AEDs, phenytoin, carbamazipine, phenobarbital, and primidone are all strong inducers of cytochrome P450 enzymes. They are autoinducers, in other words they increase their own metabolism. • Valproate inhibits cytochrome P450 enzymes. Pharmacokinetic Considerations • Most AEDs undergo complete or nearly complete absorption when given orally. • Fosphenytoin (prodrug) may be administered intramuscularly if intravenous access cannot be established in cases of frequent repetitive seizures • Diazepam (available as a rectal gel) has been shown to terminate repetitive seizures and can be administered by family members at home. • Phenytoin, fosphenytoin, phenobarbital, diazepam, lorazepam and valproate are available as IV preparations for emergency use. • Most AEDs are metabolized in the liver (P450) by hydroxylation or conjugation. These metabolites are then excreted by the kidney. Gabapentin undergoes no metabolism and is excreted unchanged by the kidney. Treatment of Epilepsy • First consideration is efficacy in stopping seizures • Because many AEDs have overlapping, pleiotropic actions, the most appropriate drug can often be chosen to reduce side effects. Newer drugs tend to have less CNS depressant effects. • Potential of long-term side effects, pharmokinetics, and cost are other considerations Treatment of Epilepsy • Monotherapy is preferred: better patient compliance, less adverse effects • Add-on therapy is often necessary to eliminate “break-through” or refractory seizures AED Treatment Options Partial seizures Simple Complex Secondary Generalized Primary generalized seizures TonicClonic Tonic Myoclonic Atonic phenytoin, carbamazepine, phenobarbital, gabapentin, oxcarbazepine, pregabalin Absence Ethosuximide Check notes valproic acid, lamotrigine, topiramate, (levetiracetam, zonisamide) Status Epilepticus • More than 30 minutes of continuous seizure activity • Two or more sequential seizures spanning this period without full recovery between seizures • Medical emergency Status Epilepticus • Treatment – Diazepam, lorazapam IV (fast, short acting) – Followed by phenytoin, fosphenytoin, or phenobarbital (longer acting) when control is established Alternative Uses for AEDs • Gabapentin/pregabalin, carbamazepine—neuropathic pain • Lamotrogine, carbamazepine—bipolar disorder • Leviteracitam, valproate, topirimate, gabapentin— migraine Questions?