ACID BASE BALANCE
advertisement

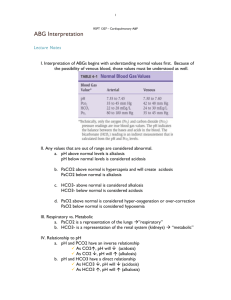
BLOOD GASES AND ACID–BASE DISORDERS Professor Magdy Amin RIAD Professor of Otolaryngology. Ain shames University Senior Lecturer in Otolaryngology University of Dundee CAPILLARY BLOOD GASES • pH: Same as arterial or slightly lower (Normal = 7.35-7.40) • pCO2: Same as arterial or slightly higher (Normal = 40-45) • pO2: Lower than arterial (Normal = 45-60) • O2 Saturation: >70% is acceptable. CAPILLARY BLOOD GASES • Saturation is probably more useful than the pO2 itself when interpreting a CBG. • The heel is the most commonly used site • The CBG is often used for pediatric patients because it is easier to obtain than the ABG • less traumatic (no risk of arterial thrombosis, hemorrhage). blood gas machines • The blood gas machines in most labs actually measure the pH ,the pCO2 and the pO2. • The [HCO3-] and the base difference are calculated values using the HendersonHasselbalch equation For a rough estimate of [H+] • • • • [H+] = (7.80 -pH) x100. This is accurate from a pH 7.25 to 7.48; 40 mEq/L = [H+] at the normal pH of 7.40. pH is a log scale, and for every change of 0.3 in pH from 7.40 the [H+] doubles or halves. • For pH 7.10 the [H+] = 2 x 40, or 80 nmol/L, and for pH 7.70 the [H+] = 1/2 x40, or 20 nmol/L. pCO2 and pH • A change in pCO2 up or down 10 mm Hg is associated with an increase or decrease in pH of 0.08 units. • As the pCO2 decreases, the pH increases; as the pCO2 increases, the pH decreases. base deficit and base excess • A pH change of 0.15 is equivalent to a base change of 10 mEq/L. • A decrease in base (i.e, [HCO3-]) is termed a base deficit, and an increase in base is termed a base excess. Acidosis and alkalosis • Acid-base disorders are very common clinical problems. • Acidemia is a pH <7.37, and • alkalemia is a pH >7.44. • Acidosis and alkalosis are used to describe how the pH changes. • The primary causes of acid-base disturbances are abnormalities in the respiratory system and in the metabolic or renal system. normal compensatory response • Any primary disturbance in acid-base homeostasis invokes a normal compensatory response. • A primary metabolic disorder leads to respiratory compensation, and a primary respiratory disorder leads to an acute metabolic response due to the buffering capacity of body fluids. • A more chronic compensation (1-2 days) due to alterations in renal function. Mixed acid-base disorder • Most acid-base disorders result from a single primary disturbance with the normal physiologic compensatory response and are called simple acid-base disorders. • In certain cases, however, particularly in seriously ill patients, two or more different primary disorders may occur simultaneously, resulting in a mixed acid-base disorder. • The net effect of mixed disorders may be additive (eg, metabolic acidosis and respiratory acidosis) and result in extreme alteration of pH; • or they may be opposite (eg, metabolic acidosis and respiratory alkalosis) and nullify each other’s effects on the pH. INTERPRETATION OF BLOOD GASES Step 1: • Determine if the numbers fit. • The right side of the equation should be within about 10% of the left side. • If the numbers do not fit, you need to obtain another ABG INTERPRETATION OF BLOOD GASES Step 2: determine if an acidemia (pH <7.37) or an alkalemia (pH >7.44) is present. Step 3: Identify the primary disturbance as metabolic or respiratory. • For example, if acidemia is present, is the pCO2 >44 mm Hg (respiratory acidosis), or is the [HCO3 -] <22 mmol/L (metabolic acidosis). • In other words, identify which component, respiratory or metabolic, is altered in the same direction as the pH abnormality. • If both components act in the same direction (eg, both respiratory [pCO2 > 44 mm Hg] and metabolic [HCO3 - <22 mmol/L] acidosis are present), then this is a mixed acid-base problem. • The primary disturbance will be the one that varies from normal the greatest, that is, with a [HCO3 -] = 6 mmol/L and pCO2 = 50 mm Hg, the primary disturbance would be a metabolic acidosis, the [HCO3 -] is about one-quarter normal, whereas the increase in pCO2 is only 25%. Step 4: • Calculate the anion gap. • Anion gap = Na+ - (Cl- + HCO3 -). • Normal anion gap is 8-12 mmol. Step 5: If the anion gap is elevated • Then compare the changes from normal between the anion gap and [HCO3 -]. • If the change in the anion gap is greater than the change in the [HCO3 -] from normal, then a metabolic alkalosis is present in addition to a gap metabolic acidosis. • If the change in the anion gap is less than the change in the [HCO3 -] from normal, then a non gap metabolic acidosis is present in addition to a gap metabolic acidosis. METABOLIC ACIDOSIS: DIAGNOSIS AND TREATMENT • Metabolic acidosis represents an increase in acid in body fluids . • Reflected by a decrease in [HCO3 -] and a compensatory decrease in pCO2. Anion Gap Acidosis: • Anion gap >12 mmol/L; caused by a decrease in [HCO3 -] • balanced by an increase in an unmeasured acid ion from either endogenous production or exogenous ingestion (normochloremic acidosis). Non anion Gap Acidosis: • Anion gap = 8-12 mmol/L; caused by a decrease in [HCO3 -] balanced by an increase in chloride (hyperchloremic acidosis). Renal tubular acidosis is a type of non gap acidosis • The anion gap is helpful in identifying metabolic gap acidosis, non gap acidosis, mixed metabolic gap and non gap acidosis. If an elevated anion gap is present, a closer look at the anion gap and the bicarbonate helps differentiate among (a) a pure metabolic gap acidosis (b) a metabolic non gap acidosis (c) mixed metabolic gap and non gap acidosis, and (d) a metabolic gap acidosis and metabolic alkalosis. Treatment of Metabolic Acidosis 1. Correct any underlying disorder (control diarrhea, etc). 2. Treatment with bicarbonate should be reserved for severe metabolic gap acidosis. If the pH <7.20, correct with sodium bicarbonate. The total replacement dose of [HCO3 -] can be calculated as follows: 3. Replace with one-half the total amount of bicarbonate over 812 h and reevaluate. • Be aware of sodium and volume overload during replacement. • Normal or isotonic bicarbonate drip is made with 3 ampules NaHCO3 (50 mmol NaHCO3/ampule) in 1 L D5W. METABOLIC ALKALOSIS: • Metabolic alkalosis represents an increase in [HCO3 -] with a compensatory rise in pCO2. Differential Diagnosis • In two basic categories of diseases the kidneys retain [HCO3 -] • They can be differentiated in terms of response to treatment with sodium chloride • and also by the level of urinary [Cl-] as determined by ordering a Spot,or random urinalysis for chloride (UCl). Chloride-Sensitive (Responsive) Metabolic Alkalosis: • The initial problem is a sustained loss of chloride out of proportion to the loss of sodium (either by renal or GI ) • This chloride depletion results in renal sodium conservation leading to a corresponding reabsorption of [HCO3 -] by the kidney. • In this category of metabolic alkalosis, the urinary [Cl-] is <10 mEq/L, • and the disorders respond to treatment with intravenous NaCl. Chloride-Insensitive (Resistant) Metabolic Alkalosis: • The pathogenesis in this category is direct stimulation of the kidneys to retain bicarbonate irrespective of electrolyte intake and losses. • The urinary [Cl-] >10 mEq/L, and these disorders do not respond to NaCl administration. Treatment of Metabolic Alkalosis • Correct the underlying disorder. 1. Chloride-responsive a. Replace volume with NaCl if depleted. b. Correct hypokalemia if present. c. NH4Cl and HCl should be reserved for extreme cases. 2. Chloride-resistant a. Treat underlying problem, such as stopping exogenous steroids. RESPIRATORY ACIDOSIS: DIAGNOSIS AND TREATMENT • Respiratory acidosis is a primary rise in pCO2 with a compensatory rise in plasma [HCO3 -]. • Increased pCO2 occurs in clinical situations in which decreased alveolar ventilation occurs. Differential Diagnosis 1. Neuromuscular Abnormalities with Ventilatory Failure 2. Central Nervous System Drugs, Sedative,,Central sleep apnea 3. Airway Obstruction a. Chronic (COPD) b. Acute (asthma) c. Upper airway obstruction d. Obstructive sleep apnea 4. Thoracic/Pulmonary Disorders a. Bony thoracic cage: Flail chest, kyphoscoliosis b. Parenchymal lesions: Pneumothorax, pulmonary edema, c. Large pleural effusions d. Scleroderma e. Marked obesity (Pickwickian syndrome) Treatment of Respiratory Acidosis • Improve Ventilation: Intubate patient and place on ventilator, increase ventilator rate, reverse narcotic sedation with naloxone (Narcan), etc RESPIRATORY ALKALOSIS: • Respiratory alkalosis is a primary fall in pCO2 with a compensatory decrease in plasma [HCO3 -]. • Respiratory alkalosis occurs with increased alveolar ventilation. Differential Diagnosis 1. Central stimulation a. Anxiety, hyperventilation syndrome, pain b. Head trauma or CVA with central neurogenic hyperventilation c. Tumors d. Salicylate overdose e. Fever, early sepsis 2. Peripheral stimulation a. PE b. CHF (mild) c. Interstitial lung disease d. Pneumonia e. Altitude f. Hypoxemia: 3. Miscellaneous a. Hepatic insufficiency b. Pregnancy c. Progesterone d. Hyperthyroidism e. Iatrogenic mechanical overventilation Treatment of Respiratory Alkalosis • Correct the underlying disorder. • Hyperventilation Syndrome: Best treated by having the patient rebreathe into a paper bag to increase pCO2, decrease ventilator rate