six sigma in healthcare
advertisement

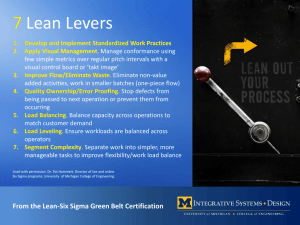
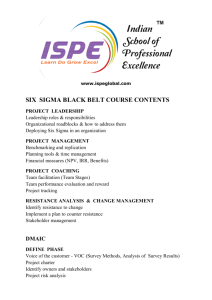
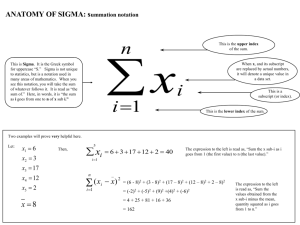
SIX SIGMA IN HEALTHCARE Matthew J. Liberatore, Villanova School of Business, Villanova University, Villanova, PA, USA Introduction The United States continues to devote substantial amounts of its resources to health care. U.S. health care spending growth decelerated in 2008, increasing 4.4 percent compared to 6.0 percent in 2007. Hospital spending growth increased 4.5 percent to $718.4 billion compared to 5.9 percent growth in 2007. Health spending growth for state and local and private sources of funds also slowed while federal health spending growth accelerated in 2008. Total health expenditures reached $2.3 trillion in 2008, which translates to $7,681 per person and an increase to 16.2 percent of the nation’s Gross Domestic Product (GDP). (US Department of Health and Human Services 2009). While health care spending continues to rise, so do concerns about health care quality. A major impetus toward recognizing the need to improve health care quality and patient safety occurred when the Institute of Medicine (IOM) released a report in November 1999 estimating that as many as 98,000 patients die as the result of medical errors in hospitals each year (IOM 2000). Through process and quality improvement efforts, the quality of health care for millions of Americans improved in 2007 but significant variations in performance continue to leave many people receiving substandard care. While quality improved for most people in private health insurance plans, there was little improvement in the care delivered to those enrolled in Medicare and Medicaid. Commercial health plans showed improvements on 44 of 54 measures of health care quality, with 16 significant gains in such areas as blood pressure control and postpartum care for women and their newborns. In contrast, health plans serving Medicare beneficiaries posted gains on only 24 of 45 measures of care, and many of those improvements were quite small. One area of notable improvement was the rate at which Medicare beneficiaries were kept on life-saving beta-blocker drugs six months after suffering a heart attack. There was little improvement in the quality of care provided to Medicaid beneficiaries. Among the 52 measures collected from Medicaid plans, only 26 showed any increase and most of those were very small. One exception was delivery of childhood immunizations. (National Committee on Quality Assurance 2008). The IOM report and the ongoing interest in improving operational cost and quality led a number of authors to suggest the application of Six Sigma to health care in the US and elsewhere (e.g., Chassin 1998; Guinane and Davis 2004; Harrington and Trusko 2005; Antony 2007). Some authors argue that Six Sigma grew out of the total quality management (TQM) movement. TQM had a number of shortcomings, including not providing evidence of better patient outcomes, increased satisfaction, or improved financials. These factors, along with its inability to remove root causes of problems and demonstrate a strategic importance, led it its eventual decline. In contrast, Six Sigma offers time and money deliverables; the sigma metric to indicate the current state of process, outcome, or service quality; and a focus on improving the “critical to quality” (CTQ) characteristics vital to internal and external customers (Black and Revere 2006). Overview of Six Sigma Six Sigma is credited with helping Motorola win the Malcolm Baldridge Award in 1988. Six Sigma is a process improvement goal that was developed by Motorola in the early 1980s and subsequently has been adopted by many organizations. Traditionally a capable process was one in which its natural variation of plus or minus three standard deviations, or sigma, from the mean was less than the target specifications. Under the assumption of normality, this translates to a process yield of 99.73 percent. Motorola's Six Sigma asks that processes operate such that the nearest target specification is at least plus or minus six sigma from the process mean. This translates into an error rate of 2 parts per billion. Often, an error rate of 3.4 parts per million is associated with Six Sigma quality, under the assumption that the process mean can shift 1.5 standard deviations on either side of the mean (Lucas 2002). Six Sigma projects are undertaken to improve the process of interest, focusing on the CTQ. A structured approach is used to uncover the root cause of problems using the DMAIC (Define-Measure-Analyze-Improve-Control) methodology: Define the problem within a process Measure the defects Analyze the cause of defects Improve the process performance to remove causes of defects Control the process to make sure defects do not recur. DMAIC is a data-driven process that uses various quality and process improvement tools that have been developed over time, including: statistical analysis, cause and effect diagrams (fishbone, Ishikawa), control charts, design of experiments, Pareto Analysis, process mapping, Failure Modes and Effects Analysis (FMEA), Quality Function Deployment (QFD)/House of Quality, and Suppliers, Inputs, Process, Outputs, and Customers (SIPOC diagrams), among others. Organizations that use Six Sigma emphasize employee participation and training through three levels: Green belts: individuals that have completed basic training and participate in Six Sigma projects Black belts: individuals competent to serve as on-site consultants and lead project teams Master black belts: individuals who have mastered the Six Sigma process and are capable of teaching it to others and acting as resources for project teams (Eckes 2001; Pande, Neuman, and Cavanagh 2000). Six Sigma is sometimes combined with lean management, which is based on the principles of the Toyota Production System (Womack et al. 1990; Womack and Jones 1996), and the resulting method is called Lean Six Sigma. Since Six Sigma is applied to ongoing processes, a related methodology, called Design for Six Sigma (DFSS) is used to determine the needs of customers and the organization, and driving those needs into the process solution developed. DFSS is applied for process generation in contrast with process improvement, and replaces DMAIC with the DMADV methodology: Define-Measure-Analyze-Design-Verify. Research Methodology To identify those journal articles that describe the application of Six Sigma in health care, an extensive search was conducted of the literature. The research process included used the keyword “six sigma,” in combination with the keywords “healthcare,” “health care,” and “hospital.” We searched Pub Med, ABI/Informs Proquest (business), Compendex (engineering), CINAL (The Cumulative Index to Nursing and Allied Health Literature), and PsycINFO using these keywords. The topics of the articles that were uncovered in the database searches were screened to determine if the Six Sigma methodology had either been recommended for application or actually applied in a health care context. Our search excluded conference proceedings and doctorial dissertations since we assume that important research will eventually appear in academic or profession journals. We also exclude non-English language publications from our search. Analysis There are some studies that have attempted to assess the implementation of Six Sigma in health care. Feng and Manuel (2007) surveyed health care organizations using online listsevs hosted by the Healthcare Information and Management Systems Society and the Society for Health Systems. Fifty-six organizations responded to the survey, a 1.72% response rate. Of the respondents, 15 organizations are practicing Six Sigma. Various types of projects have been performed by the respondents, and these tend to focus on cycle time reduction, process flow improvement, and medical-error reduction. These projects were performed in various departments, from emergency to surgical rooms, from purchasing to billing, from pharmacy to radiology. Only four of the respondents had both implemented the program for more than one year and provided information on annual savings and costs. Antony et al. (2007) include a summary of outcomes and financial savings from ten health care organizations having Six Sigma programs. Again, a broad range of CTQs and process metrics were improved, including: waiting times, patient transfer times, throughput, post-op infection rate, medication and laboratory errors, discharge time, patient satisfaction, time to pain management, and turnover time. Of the ten firms, six were able to estimate cost savings and/or revenue increases. All of these applications are found in more detail in specific articles found in the literature review. To obtain a better understanding of the extent of successful Six Sigma implementation, those articles describing specific Six Sigma applications were classified by area of application within health care delivery along with the metrics improved. We also note whether data on the level of improvement of the metric(s) are provided, and whether the application is Six Sigma, Lean Six Sigma, or DFSS. Since most of the reported applications are in hospitals or medical centers, we organized the applications into categories and sub-categories as follows: For Hospitals/Medical Centers: Inpatient Care – Admission, Medical/Surgical, Perinatal/Obstetrical, Intensive/Critical, Psychiatric, Rehabilitation/SNF, Hotel Services, Discharge, Other Therapeutic Support – Laboratory, Diagnostics, Pharmacy, Respiratory Emergency Care – Admission, Treatment, Discharge Ambulatory Care -- Home Health, Surgical, Clinic, Rehabilitation For Physician Practice (one category) The process performance metrics were categorized as: Process Time, Defect/Defect Rate, Compliance, Productivity, Revenue Increase, Cost Decrease, Satisfaction, Other. Within each metric category, specific metrics are noted. For example, within process time, specific metrics include wait time, turnaround time, throughput time, cycle time, and off load times. Conclusion The categorization of the Six Sigma application literature is in process. Expected findings include those areas that have seen the most successful application, potential application areas, and the extent to which metrics have improved, enabling the assessment of the overall effectiveness of Six Sigma in healthcare.