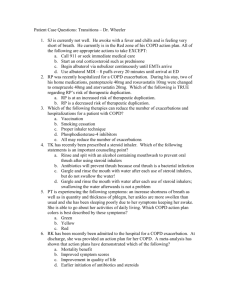
Routes of Steroid Administration for COPD Exacerbation

USE OF STEROIDS IN PATIENTS
WITH COPD EXACERBATION
Richard C. Walls
Patient Case: JS
64 yo female who presented with increasing shortness of breath, wheezing, and hypoxia that did not adequately respond to oxygen supplementation and intensified bronchodilator therapy.
PMH and Home Medications
Atrial Fibrilation
Aspirin 81 mg daily
Digoxin 0.25 mg daily
Diltiazem 240 mg daily
Depression/Anxiety
Duloxetine 30 mg daily
Lorazepam 1 mg BID prn
Quetiapine 150 mg qhs
COPD
Ipratropium 2.5 mL q6h prn
Hypothyroidism
Levothyroxine 25 µg daily
Type II Diabetes
Metformin 500 mg BID
Hyperlipidemia
Simvastatin 20 mg qhs
Inpatient Medications
Albuterol 2.5 mg prn
Azithromycin 500 mg po
Methylprednisolone 60 mg IV
Why Steroids?
Niewoehner et al. (1999) 1
271 patients: 3 Treatment Groups
Placebo (n=111)
3 days of methylprednisolone 125 mg q6h IV followed by
Oral prednisone tapered over 2 weeks (n=80)
Oral prednisone tapered over 8 weeks (n=80)
Primary outcome: death, intubation, readmission, or intensification of COPD therapy
Why Steroids?
30 days
90 days
6 months
Percentage of Patients With a Primary Outcome Event 1
Placebo 2 Weeks Steroids 8 Weeks Steroids
33% (3% death)
48% (4%)
54% (4%)
24% (0%)
38% (2%)
49% (2%)
22% (2%)
36% (2%)
52% (4%)
Fewer events with steroids after 30 & 90 days
No effect on mortality
No effect on all-cause mortality
No difference between duration of steroid treatment
Placebo length of stay 1.2 days longer than steroid
More adverse events with steroids
Hyperglycemia the most common significant adverse event
Why Steroids?
Davies et al. (1999) 2
14 days of 30 mg prednisone po (n=29) daily or placebo (n=27)
Greater increase FEV
1 treatment) with prednisone (92% vs. 85% at day 5 of
Placebo length of stay 2 days longer than steroid
GOLD guidelines 3
Recommend 30-40 mg prednisolone daily for 10-14 days in patients with COPD exacerbation
Recently updated (2013) to include all patients with COPD exacerbations
Recommendation graded Evidence Category D indicating a panel consensus judgment
Controversies
Is oral administration as effective as IV?
Is there a role for inhaled steroids in the treatment of COPD exacerbations?
Does the evidence support 30-40 mg prednisone daily for 10-14 days as an ideal regimen?
Oral vs. IV Steroids
de Jong et al. (2007) 4
5 days of 60 mg prednisolone daily either IV (n=107) or po (n=103)
Evaluated treatment failure: death, ICU admission, readmission to ICU due to
COPD, or intensification of therapy within 90 days of treatment
Oral (56.3%) non-inferior to IV (61.7%)
Overall treatment failure higher than 2 week regimen in Niewoehner trial (38%) 1
First three days of Niewoehner trial featured steroid doses 2.6 times higher 5
No data reported on adverse events
Ceviker, Sayiner (2013) 6
7 days of 32 mg methylprednisolone po daily (n=20)
4 days 1 mg/kg/day methylprednisolone IV then 3 days of 0.5 mg/kg/day (n=20)
Both groups showed improvement in FEV
1
(49.1% oral vs. 40.0% IV)
Less incidence of hyperglycemia in oral (22.2% vs. 55%)
Did not compare equipotent steroid doses
Systemic vs. Inhaled Steroids
Gunen et al. (2009) 7
Reviewed trials comparing nebulized budesonide to systemic steroids
No difference in efficacy, fewer adverse events
(especially hyperglycemia) with budesonide
Only reviewed 7 trials
Small trials (Averaged 88 patients)
Short trials (Longest was 16 days)
3 of the trials were for asthma exacerbation
Implications for JS
Literature Summary
Suggest usefulness in COPD exacerbation
No clearly ideal dose, duration, or route of administration
Suggests dose-response/dose-toxicity relationship
Pertinent Patient Specific Factors
Type II Diabetes: Risk of hyperglycemia with high doses
Exacerbation possibly secondary to infection: Do we really want to expose JS to another route of infection?
JS is currently tolerating oral medications
Exacerbation is not so severe that it is immediately life threatening
Implications for JS
Given the patient’s clinical picture that puts her at risk for corticosteroid and IV access related complications, IV therapy at this point is likely inappropriate, and initiating a course of 30 mg oral prednisone daily would be more appropriate.
References
5.
6.
7.
1.
2.
3.
4.
Niewoehner DE, Erbland ML, Deupree RH, Collins D, Gross NJ, Light RW, et al. Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. Department of Veterans
Affairs Cooperative Study Group. N Engl J Med 1999 Jun 24;340(25):1941-1947.
Davies L, Angus RM, Calverley PM. Oral corticosteroids in patients admitted to hospital with exacerbations of chronic obstructive pulmonary disease: a prospective randomised controlled trial. Lancet
1999 Aug 7;354(9177):456-460.
Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. NHLBI/WHO workshop report. Bethesda, MD:
National Heart, Lung, and Blood Institute; April 2001. Updated February
2013, http://www.goldcopd.com/ .
de Jong YP, Uil SM, Grotjohan HP, Postma DS, Kerstjens HA, van den Berg JW. Oral or IV prednisolone in the treatment of COPD exacerbations: a randomized, controlled, double-blind study. Chest 2007
Dec;132(6):1741-1747.
National Adrenal Diseases Foundation. Corticosteriod Comparison Chart. http://www.nadf.us/tools/adrenalhormone.pdf
Ceviker Y, Sayiner A. Comparison of two systemic steroid regimens for the treatment of COPD exacerbations. Pulm Pharmacol Ther 2013 Mar 18.
Gunen H, Mirici A, Meral M, Akgun M. Steroids in acute exacerbations of chronic obstructive pulmonary disease: are nebulized and systemic forms comparable? Curr Opin Pulm Med 2009 Mar;15(2):133-137.