Analysis of Outcomes - Nurse Educator Portfolio
advertisement

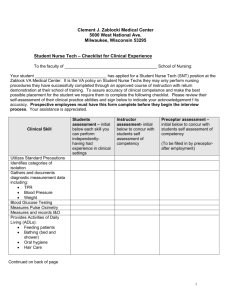
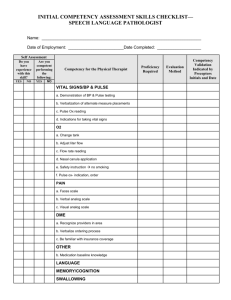
Running head: COMPETENCY CHECKLIST Resource Nurse Competency Checklist Betty J. Sousley Ferris State University 1 COMPETENCY CHECKLIST 2 Abstract Emergency Nurses Association [ENA] (2011) relies on the Standards for Practicing Nurses to define the standardization of competent skill sets for nurses in the emergency department. Emergency Nurses possess a specialized set of skills within their area of expertise. Benner’s Theory (1984) from Novice to Expert, identifies categories in which a nurse is functioning, based on skill level. Nurses that have the knowledge, experience, and skill to perform at the proficient and expert level are suitable candidates as a resource nurse. The duties that the resource nurse is responsible for are numerous, and performed at the proficient and expert level. Although there has not been a standardization defined for the resource role, identifying the role’s responsibilities and competencies are necessary. The development of a resource nurse competency checklist will set the foundational standards for this vital and integral role. Keywords: resource nurse competency checklist, proficient, expert COMPETENCY CHECKLIST 3 Resource Nurse Competency Checklist Accurate documentation of skills and competencies for the individual nurse should be concise and standardized. Competency checklists can vary, depending on the responsibilities and skill level of the nurse. A standardized competency checklist that identifies the roles and responsibilities of the resource nurse was researched. Through the research conducted, managerial responsibilities and extra duties assigned to the resource nurse were identified. These tasks and duties are not identified in the current competency checklist at Allegan General Hospital (AGH). The current competency checklist used at AGH (see Appendix A) is utilized for initial orientation, six-month evaluation, annual evaluation, and any progression that would indicate advancement in skill level. This checklist became cumbersome with various dates and signatures. Leading to difficulty in the differentiation of which skill was mastered, date and time of the accomplished skill and the name of the preceptor signing the form, indicating that the employee can perform at set of skills, and at which skill level. The competency checklist included all the skill levels, from novice to expert, on the same checklist, leading to confusion. In any setting, emergency nurses must integrate critical thinking skills and evidencebased knowledge into their practice (ENA, 2011). Small community hospitals, like AGH, have fewer resources to rely on and therefore count on the skill and expertise of the nurses. With the lack of immediate access to specialized care and limited diagnostic capabilities, it is imperative that the nurse functions at the proficient and expert skill level. The purpose of this paper is to: identify and incorporate the common threads of responsibilities and tasks assigned to the resource nurse to the competency checklist, discuss the development and presentation of the project, including the goals and objectives, and an analysis COMPETENCY CHECKLIST 4 the outcome of the project. A PowerPoint presentation and evaluations from the stakeholders and preceptor of the scholarly project are identified, along with a self-evaluation (see Appendix D, E, F). Overview of Scholarly Project In a time when knowledge and technology is ever increasing and nursing is practiced in various settings, it is essential that the new nurse be prepared to provide safe, accurate, and compassionate care (Benner, Sutphen, Leonard, & Day, 2010). Nurses must be able to assess a patient, understand their disease or illness, and be able to apply care based on the knowledge and skills they have gained. The heightened levels of responsibility and duties that accompany the resource role necessitates that the nurse possess a measureable competency in clinical experience and skills. According to Benner’s Theory (1984) from Novice to Expert, the skill level of a nurse varies and can vacillate between levels, depending on environment. The advanced beginner relies on textbook accounts of patient signs and symptoms related to disease, injuries, and therapies but cannot recognize subtle variations or gauge the severity in relation to other situations (Benner, 2004). The expert nurse integrates the grasp of the situation into the action taken (Benner, 2004). Eggenberger (2012) identifies the resource nurses as the ones that provide a unique leadership perspective, supporting frontline care that improves quality of care, safety, and patient satisfaction. The ENA (2011) defines the resource role as being that of the expert nurse that possess excellent clinical experience and skill that supports evidence-based best practices for safety. The use of a competency checklist documents the aptitude of these skills. However, not all competency checklists are identical. COMPETENCY CHECKLIST 5 Allegan General Hospital is a critical access hospital in Allegan, MI. The emergency department continues to grow and the current competency checklist must reflect the changes that have occurred within the environment. A research of the surrounding emergency departments was conducted within a 50-mile radius, in hopes to obtain data as to their resource nurse competencies. The objective was to compare the resource nurse competency checklist being utilized by these facilities and incorporate the findings with the current competency checklist for revision. The research involved seven hospitals, starting with the four smaller organizations that were comparable to the culture of AGH. It did not take long to identify lack of uniformity or standardization of a competency checklist for the resource nurse within these smaller organizations. The research began with interviewing emergency department representatives from Lakeview, Borgess-Pipp, Three Rivers, and Pennock hospitals as to their competency checklist for the resource roles and practices. T. Johnson (personal communication, January 21, 2012) identified the emergency department at Lakeview Hospital as one that did not have a designated resource nurse. The hospital is not a trauma center and therefore utilizes the house supervisor as the resource “charge” nurse. The only qualification is that the house supervisor has taken a Trauma Nursing Core Curriculum (TNCC) course. B. Chrisman (personal communication, January 22, 2012) describes the emergency department at Borgess-Pipp Hospital similar to that of Lakeview Hospital. The house supervisor serves as the resource nurse. There only specific qualification is that the house supervisor is an experienced practicing nurse of five years. COMPETENCY CHECKLIST 6 L. Kent (personal communication, January 23, 2012) serves as the clinical coordinator at Three Rivers Hospital. The hospital utilizes the clinical coordinator as the resource “charge” nurse. The only qualification is that the house supervisor has taken the TNCC course. J. Wolf-Duis (personal communication, January 24, 2012) is a registered nurse in the emergency department at Pennock Hospital. They have natural leaders within the department, and they are the nurses designated and resume the resource role. Their qualifications are that they have to have taken Advanced Cardiac Life Support (ACLS) and TNCC at some point in their career. The TNCC certification is valid for four years after completion of the course and they do not have to renew their certification. The lack of support from the research conducted required an expansion, and three larger hospitals were then interviewed. A. Freeze (personal communication, January 25, 2012) described the emergency department at Metro Health Hospital as one that utilizes clinical coordinators as their resource nurses. The qualifications for these resource nurses is that they must have a minimum of four years emergency nursing experience and be certified in TNCC, Emergency Nursing for Pediatric Course (ENPC), ACLS, and hold a Baccalaureate degree. D. Dominguez (personal communication, January 28, 2012) describes the emergency department at Bronson Methodist Hospital as one that requires the resource nurse to have two years’ experience on the trauma team and one-year experience in triage. The resource nurse has an extensive interview process with two resource nurses and one emergency physician. The mandatory competencies are TNCC, ENPC, ACLS, and Pediatric Advanced Life Support (PALS). J. Beckman (personal communication, February 2, 2013) describes the emergency department at Spectrum Health Hospital as one that has an extensive orientation and resource COMPETENCY CHECKLIST 7 nurse responsibilities. The resource nurse is required to follow their patient to the Cardiac Catherization Lab, shadow at the Burn Center, spend two hours with a physician, two hours with a pharmacist, and four hours with a respiratory therapist. They have 20 classes to complete which include their computer system, core classes, triage class, lab, culture safety, and electrocardiographic interruption. The certifications and qualifications requirements include TNCC, ENPC, and ACLS. The research from the surrounding hospitals lacked support from governance committees, evidence based practices, or standardization in regards to resource specific competency checklist. Therefore, I turned to the ENA experts for guidance and support. The set standards and measuring criteria set by the ENA (2011) mirrored that of the core competencies from the NLN (2005). The research conducted provided a plethora of orientation information on the role of the resource nurse, but not reflective solely to the competencies for the resource nurse. Additional research will be required in identifying standardization for a resource nurse competency checklist. The common threads found during the research were that of leadership responsibilities, counseling, precepting, throughput and workflow. These common threads reflect a compilation of core practice competencies (see Appendix B) that served as the foundation for the revision of the current competency checklist. The orientation information obtained from the research was woven into the revised competency checklist. These competencies assisted in meeting the goal of developing and implementing a resource competency checklist that was user friendly, easier to follow, with clear timeframes, expectations, and performance at the proficient and expert level at AGH (see Appendix C). Evidence supports that the proficient and expert skill level nurses provide the best evidence-based practices and have better outcomes (ENA, 2011). COMPETENCY CHECKLIST 8 Personal and Professional Accountabilities A responsibility of nurse educators is to function as a change agent and improve the quality of the care. Through the revision and implementation of the competency checklist, the care delivered at Allegan General Hospital can be improved. Through the implementation of the revised competency checklist, the resource nurse will have a better understanding and clearer expectations of what the role entails and hold the resource nurse accountable, not only to the organization, but to the professional standards in which they are governed. The revised competency checklist may facilitate a domino effect within the organization. Job titles reflecting of the competency checklist will be required. The job description will require mirroring that of the competency checklist, and the orientation will require a makeover. ENA (2007) identifies the orientation of emergency registered nurses requires a global knowledge base established through the application of a specific body of evidenced-based knowledge. As an educator, there is a desire to bridge the gap between the manners in which we currently practice and practice that is supported and governed through accrediting bodies (NLN, 2005). As practicing nurses, it continues to be our responsibility to search for opportunities to bring the best evidence based practices to our work place and institute necessary changes. Institute of Medicine (2010) identify that emergency registered nurses be encouraged to participate in lifelong learning, pursue certifications, obtain advanced degrees, and hold active membership in in their professional organizations. The development of the resource nurse competency checklist aligns with the Core Competencies V: Function as a change agent and leader and Core Competency VI: Pursue continuous quality improvement in the nurse educator role (NLN, 2005). The nurse educator is COMPETENCY CHECKLIST 9 responsible for implementing change and being the change agent. This allows educators the opportunities to develop leadership skills to promote and implement change. Kirby and DeCampi (2008) state nursing leadership is vital to the effectiveness and efficiency in the emergency setting and provides the building blocks for safe practice and care. Core Competency V: Function as a Change Agent and Leader The goal was to revise the current resource nurse competency checklist. The revision would identify and reflect the resource nurse as one who functions at the proficient and expert level. Benner (2011) identified that the emergency nurse leader as one that is supported and proactively engaged in their personal and professional growth as they advance form novice to expert through lifelong learning, coaching, mentoring, and classroom experience. The personal accountability was demonstrated by functioning as a change agent and leader through the research conducted to support the necessary changes and identify the commonalities of the roles and responsibilities of the resource nurse. A competency checklist should mirror that of the proficient and expert nurse along with the core practice standards and additional responsibilities assigned. The development of a PowerPoint presentation to the stakeholder at AGH based on the research obtained and the integration of the common threads of standardized core practices was conducted. After the presentation, analysis of the evaluations, and making any potential revision based on feedback, I would then present the scholarly project to the Medical Director and the forms committee for implementation. Having the ability to bridge the gap between the research and knowledge allows the opportunity to become a change agent and channel the evidence back into practice. COMPETENCY CHECKLIST 10 Core Competency VI: Pursue continuous quality improvement in the nurse educator role The goal was to pursue continuous quality improvement in the nurse educator role. The objective was to identify the role of the resource nurse as being at the proficient and expert level, provide clarity of the checklist, and be user friendly. The nurse educator is responsible for continuous quality improvements. The personal accountability was demonstrated through the initiation of improving the current competency checklist to reflect best practices and the changes within the environment of the emergency department. The emergency department has acquired additional rooms, equipment, and implementation of electronic medical record (EMR) system. The current competency checklist lacked the identification of the new space, equipment, and EMR. It also lacked ease of identifying timeframes of completion of skills and tasks. The revisions clearly identify specific periods and timeframes in which skills and tasks are accomplished. By identifying the resource nurse at the proficient and expert level, the competencies are identified for that specific role and responsibilities. As nurses orientate, they are given a competency checklist. Due to the complex checklist and the lack of ease with the current competency checklist (see Appendix A) at AGH is utilized for orientation, six-month evaluation, annual evaluation, and during the nurses’ advancement in their skills. This checklist is cumbersome and difficult to differentiate between achieved skills and not completed skills. By the end of one year, the individual’s competency checklist had various dates, checkmarks, and signatures leaving the checklist indiscernible. The revisions made to the competency checklist will improve the processes in which novice though expert nurses can be differentiated along with the skills, and tasks assigned (see Appendix C). COMPETENCY CHECKLIST 11 Analysis of Outcomes Implications of the outcomes of this scholarly project will hold the nurses accountable for the role in which they practice. Historically, if a nurse has been practicing within a specialty area for greater than a year, that nurse would qualify as a resource nurse. Organizations are placing inexperienced nurses in positions that require additional education and training. Without proper training and education, nurses would not be meeting or practicing within their scope and standards for practice. This could potentially set the stage of noncompliance to the ENA (2011) and NLN (2005). Nurse educators are challenged as the experienced nurses are leaving the workforce and inexperienced nurses are replacing them. Valdez (2009) identified that with the increasing number of nurses leaving the workforce, due to burnout, complacency, or the aging population this leaves the inexperienced nurses practicing. This positions the nurse educators to develop educational opportunities for those left to fill the shoes of those experienced nurses departing the emergency department (Valdez, 2009). With budget cuts and downsizing, utilizing experienced nurses to educate those requiring experience and skill in the development of critical thinking, clinical judgment, and reasoning would be the best manner in which to alleviate additional financial burden to an existing problem. Providing the opportunity to capitalize on the experienced nurses mentoring and sharing their experiences remains a focus for the educators. ENA position statement (2011) states that nurse leaders in the emergency department possess licensure as a registered nurse with experience in the specialty of emergency nursing. Leaders of organizations are to ensure that the registered nurses are qualified and competent to practice. Legal and Ethical Concerns Emergency nurse leaders consistently apply ethical principles that demonstrate honesty, integrity, and respect (ENA, 2011). There are legal and ethical ramifications for holding nurses COMPETENCY CHECKLIST 12 accountable for the job they perform. They must be practicing within their scope of practice and be able to delegate to others. Legally, the job description and education of the individual performing in that role can be called to question. The ethical question may come in to play when the job description and title are not disclosed in its entirety and changed for the organizations benefit. As a case in point, the staffing ratio is typically 2:1, staff is on vacation, and it is a holiday weekend so the ratio increases to 3:1. The staff that was on orientation suddenly is off orientation because staffing is short and now there is a need. Vacancies in staffing and safety ratios are not for the benefit of the organization or manager convenience. Charge nurses cannot just be placed in that position because there is a need, training and competencies are required. A safe environment for the patients, staff, and organization are to be the frontline priority. The educational background, training, and qualifications may also be explored. Without standards that are outlined and evidence demonstrating the competency of the nurse functioning in that role, it can prove to be a danger. Humphries Lynch (1997) state that child and/or adult abuse and neglect, sexual assault victims, and other forms of violence are reportable mandates. The presence of the registered nurse in these situations is also required. Reportable mandates of these circumstances can and may go unreported when nurses are placed in situations they are not competent or have knowledge of these mandates. Nurses can be held civilly and criminally liable if he or she fails to make a report of suspected abuse (Lewin, 1994). If they contravene such obligations, they face penalties. In addition to the penalties, and when the nurse is functioning outside the scope and standard of practice, that individual can jeopardize their license. When certain situations are presented in the court of law, you are subjecting your licensure to a potential disciplinary action and the organization to financial retribution and settlements. COMPETENCY CHECKLIST 13 Nursing Concerns The Standards of Emergency Nursing Practice (ENA, 2011) states that nurses’ practice is guided by the Code for Nurses (ENA, 2011) and identify that “the emergency nurse functions autonomously to the extent that knowledge, skills, and role permit” (p. 44). Utilizing unqualified nurses and placing them in roles that they are not equipped to perform in, whether it is through knowledge or skill level is concerning, unethical, and may have legal ramifications. Without accountability, the threshold for patient advocacy can atrophy. Nursing can improve upon the manner in which they practice. By remaining diligent and researching, the best practices they improve upon the care they delivery and can implement change. It is only through lifelong learning that we remain on the cutting edge of technology and improving outcomes. Bringing the best practices to the profession for better outcomes is in turn being the best advocate for the patients. Change is inevitable and constant; we must become part of that change. Organizational Concerns Nurses must have knowledge and understanding to protect the organization (ENA, 2011). Interfacility transfer guidelines as mandated by Consolidation Omnibus Budget Reconciliation Act of 1986 (COBRA)/Emergency Medical Treatment and Active Labor Act (EMTALA) legislation require compliance. There are fines attached to violations for these serious infractions. It is the obligation of the nurse to have knowledge of guidelines and mandates. Bond (2008) identified implications of EMTALA during the triage process. When nurses are assigned duties and they lack knowledge of regulatory mandates the organization could suffer the ramifications of improper processes related to EMTALA and COBRA. Allowing inexperience nurses to function in a resource nurse role for which they have not been properly prepared sets the stage for unnecessary potential limitations. Inexperienced nurses may find COMPETENCY CHECKLIST 14 themselves in situations that require adherence to guidelines and mandate requirements they were for which they are unaware. General Concerns The issues, concerns, and challenges encountered during this scholarly project largely centered on the fact that there was no standardization specific to the resource role and responsibilities identified on the competency checklist. The research conducted identified similar orientation standards and core practice competencies that were included in the revised competency checklist (see Appendix B). These core practice competencies address and align with the Standards of Emergency Nursing Practice according to the ENA (2011). These competencies align with that of the expert nurse as well, and have been adopted into the revised resource nurse competency checklist (see Appendix C) for Allegan General Hospital. The emergency department manager and reflection in the job description of the resource nurses can also utilize this core practice competencies during annual evaluations. The ease of adapting this within the organization and flowing through to other department would be practicable. The greatest concern was the lack of identifying the resources role into the proficient and expert level of nurse and the skills required to maintain that position. Without standardization, care of the clients and communities can be compromised. ENA (2011) state evaluation of specialized knowledge and clinical judgment by a credentialing agency contributes to quality of care. Nurses who function at capacities in which they are not educated to practice should be informed of the legal and ethical concerns that may be encountered. The implementation for change was addressed to the stakeholders at Allegan General Hospital through the awareness of a presentation of the revisions to the competency checklist. Even though change is constant, it continues to be met with resistance. By pointing out the difficulties within the current COMPETENCY CHECKLIST 15 competency checklist, the presentation would reflect the ease of use, clarity, improve outcomes and the care delivered, motivating buy-in. Evaluation of Scholarly Project An evaluation is a tool that measures objects, events, or people into categories (Wood & Ross-Kerr, 2011). Once the data is collected and analyzed, the evaluator can identify areas that require improvements and areas that were positive. Polit and Beck (2012) state a Likert Scale indicates the degree in which a respondent agrees or disagrees with a statement. Open-ended questions are geared towards the identification of perception or opinion of the evaluator, not limiting the answers to pre-established alternatives (Polit & Beck, 2012). The open-ended comments will provide feedback for further growth and areas of improvement, serving as a valuable tool. One of the most valuable tools for the growth of individuals is that of the feedback from the evaluations. The completed evaluations from the stakeholders (see Appendix D) and preceptor for this scholarly project (see Appendix E) were reviewed and analyzed. Areas of strength were consistent in the fact that the presenter had a great deal of knowledge of the topic, workflow, and challenges in the emergency department at AGH. Knowing the audiences skill level and knowledge base provided the presenter insight to determine the depth that explanations would need to be to make a point or relay information. Specific meaning and theorist did not require additional defining as this was a familiar topic to the stakeholders. Knowing the audience and their knowledge base provided the presenter with an ease as to the word usage and set the pace in which to articulate. Brouse (2007) states the importance of connecting and knowing your audience is relevant, the audience wants to know what information they can learn for themselves and are interested in what the speaker has to say. Key factors during a presentation or public COMPETENCY CHECKLIST 16 speaker is commonality and the culture of the audience. The feedback provides areas of strengths, weaknesses, and comments for the presenter to reflect and grow for future scholarly work. A self-evaluation (see Appendix F) completes the scholarly project. The feedback from the stakeholders and preceptor provided an opportunity to self-reflect and accept considerations for areas of growth. The feedback and comments provide insight into areas of improvements. Knowing that the topic was intertwined with the role, confusion occurred for brief periods. Having this pointed out in an evaluation confirmed the need for the presenter to clarify and be mindful of being concise and clear as to the topic. This experience has provided the presenter the opportunity to meet the core competencies according to the NLN (2005) Scope of Practice for Academic nurse Educators. Having the opportunity to develop and present this resource nurse competency checklist was an experience every student should embrace. Recommendations It has been clearly identified that competency checklists differ from organizations and are based on the culture of the organization. The separation of nurse skill levels, from the original competency checklist, would ease the use of the competency checklist, along with decreasing the confusion as to what skill a nurse is competent. The resource nurse competency checklist defines the specific role and responsibilities to which the nurse is held accountable. By identifying the dates and preceptor’s signature, on the competency checklist the individual nurse, preceptor, and manger will be able to identify the progress of the nurse. A recommendation for the original competency checklist is to separate the skill levels into the identifying roles of the nurses, using Benner’s Theory from Novice to Expert skill level. The resource nurse needs to function at the proficient and expert level. According to the COMPETENCY CHECKLIST 17 definition of roles at AGH, the resource nurse is considered first-person. Once the revised competency checklist is implemented, the secondary and tertiary roles will need to be revised and have a checklist to reflect specific skill level and responsibilities. Utilizing ENA (2011) Standards of Emergency Nursing Practice as a starting point for competencies, provided a solid foundation for the checklist and provides unity across the profession. Providing a competency checklist that mirrors NLN (2005) Scope and Standards for Practice will assist in guiding the nurses toward providing the best evidence-based practices for better outcomes. Evidence suggests that the expert nurse is proficient and processes expert clinical experience and skills (Benner, 2011). Research has indicated that a nurse practicing at the proficient and expert level provides the environment in which best outcomes can be achieved. Conclusion Retaining records of competencies that reflect an individual’s accomplishment of skills and tasks is imperative. These skills and tasks are recorded on a competency checklist. Clarity and ease of identifying competencies is crucial. The original competency checklist utilized at AGH had identifiable areas requiring revision. During the project for standardizing a competency checklist at AGH, research was conducted within a fifty-mile radius. Seven hospitals were interviewed in regards to practices they currently use for the resource nurse. Unfortunately, there was not a standardized checklist. Common threads of core practices were identified from the research and utilized as a foundation for the revision of the original checklist. Commonalities for the resource nurse were managerial tasks and additional duties. Research has identified that nurses practicing at the proficient and expert level have additional responsibilities, and are held accountable to various other duties. The competency COMPETENCY CHECKLIST 18 checklist should reflect the additional responsibilities assigned. Nurses should be aware of the legal and ethical ramifications, to themselves and the organization, if they are practicing outside of their scope and standards for practice. Research also suggests that the proficient and expert nurses have a more global view of their environment, organization, and profession (ENA, 2011). A resource nurse competency checklist that identifies the nurse at the proficient and expert level was developed. A Power Point presentation of the revised checklist that includes the roles and responsibilities of the resource nurse was presented to the stakeholders at AGH. Through the implementation of the scholarly project, change and continuous quality improvements can benefit patients, the nursing profession, and organization collectively. COMPETENCY CHECKLIST 19 References Benner, P. (1984). From novice to expert: Excellence and power in clinical nursing practice. Reading, MA: Addison-Wesley. Benner, P. (2004). Using the Dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education. Bulletin of Science Technology & Society, 24, 188-199. doi: 10.1177/0270467604265061. Benner, P. (2011). From novice to expert. Retrieved from http://currentnursing.com/nursing_theory/Patricia_Benner_From_Novice_to_Expert.html Benner, P. B., Sutphen, M., Leonard, V., & Day, L. (2010). Educating nurses: A call for radical transformation. San Francisco, CA: Jossey-Bass. Bond, P. G. (2008). Implications of EMTALA on nursing triage and ED staff education. Journal of Emergency Nursing, 34, 205-206. Brouse, C. (2007). Promoting discussions about cultural competence in an undergraduate health course. Health Education Journal, 66(2), 179-187. Eggenberger, T. (2012). Exploring the charge nurse role holding the frontline. Journal of Nursing Administration, 42(11), 502-506. doi:http://0dx.doi.org.libcat.ferris.edu/10.1097/NNA.0b013e3182714495 Emergency Nurses Association. (2007). Emergency nursing orientation online. Des Plaines, IL: Author Emergency Nurses Association. (2007). Trauma nursing core course (6th ed.). Des Plaines, IL: Author. COMPETENCY CHECKLIST 20 Emergency Nurses Association. (2011). Emergency nursing scope and standards of practice (1st ed.). Des Plaines, IL: Author. Humphries Lynch, S. (1997). Elder abuse: What to look for, how to intervene. American Journal on Nursing, 97,27-32. Institute of Medicine. (2010). The future of nursing: Leading change, advancing health. Washington, DC: National Academies Press. Kirby, K. K., & DeCampli, P. (2008). Nurse manager development beyond the classroom. Nurse Leader, 6(2), 44–47. Lewin, L. (1994). Child abuse: Ethical and legal concerns for the nurses. Journal of Psychosocial Nursing and Mental Health Services, 32(12), 15-8. National League for Nursing. (2005). The scope and practice for academic nurse educators. New York, NY: National League for Nursing. Polit, D. F., & Beck, C.T. (2012). Nursing research: Generating and assessing evidence for nursing practice (9th ed.). Philadelphia, PA: Wolters Kluwer Health. Valdez, A. (2009). So much to learn, so little time: Educational priorities for the future of emergency nursing. Advanced Nursing Journal, 31(4), 337-353. doi: 10.1097/TME.0b013e3181bcb571 Wood, M. J. & Ross-Kerr, J. C. (2011). Basis steps in planning research: from question to proposal (7th ed.). Sudbury, MA: Jones and Bartlett. COMPETENCY CHECKLIST 21 Appendix A Name:______________________________________________ Unit/Department:_______________________ COMPETENCY SUMMARY FOR E.D. REGISTERED NURSES This document may be used for: o Orientation o Performance Updates o Annual Review It is required for Resource qualified personnel to achieve all P and/or E ratings COMPETENCY LEVEL N-Novice Needs assistance of other user or manual to perform function. Follow rules/guidelines AB-Advanced Beginner Performs function with minimal assistance, can describe function. Simple decision making. C-Competent P-Proficient E-Expert (Expected level one year post-hire) Comfortable, familiar with function. Consistently accurate in performing function. More complex decision making. Similar to competent can perform with increased speed. Can demonstrate function to another. Comfortable with complex decisions. Able to teach another how to perform function. Understands how function impacts other users of system. Able to mentor others. Preceptors to evaluate competence level, check appropriate boxes, initial, date and sign form. Return to manager or________________ when complete. This document will be stored in Unit Personnel file and COMPETENCY CHECKLIST 22 reviewed annually. Signatures: Preceptor: ___________________ Preceptor: _____________________ Preceptor: Date: ____/______/______ Date: _____/_____/______ _________________________ Date: ____/_____/____ Unit Specific-Emergency Department Environment Work with preceptor Order entry Work with preceptor Computer classes Care of the patient with a burn Work with preceptor Emergency Nursing Core Curriculum 5th Edition (pg 184-191) Care of the patient who is having a pelvic exam Work with preceptor Locate supplies Document correct information Determine what physician is on call from the call schedule list Preceptor will confirm ability to: Accurately enter lab and x-ray orders [ ] Perform lab inquiry [ ] Cancel lab or x-ray orders [ ] Order blood [ ] Microbiology orders [ ] Preceptor will confirm ability to care for a patient with a burn: Fluid replacement (Parkland formula) Assessment of airway Burn dressing – Verbalize special considerations for facial burns – Splinting burns for maximum function after healing Recheck of a burn patient Preceptor will confirm ability to: Assist with routine pelvic exam Select the correct culture media Assist with vaginal bleeding patient I C A A D G Evaluation Date Age Specific I–Infant (Birth-1) C-Child (2-12) A-Adolescent (13-18) AD-Adult (19-65) G-Geriatric (>65) Blank – N/A Month/Day/Year Place competence code in appropriate Age Specific level. N-Novice AB-Advanced Beginner C-Competent P-Proficient E-Expert Verification Method V-Verbal D-Demo L-Lab C-Computer Initials Evaluation Mechanism Hands On Learning Options Review Performance Criteria Evaluator’s/Preceptor’s Employee: _______________________________________ Date: ______/______/_ COMPETENCY CHECKLIST Care of the alleged sexual assault victim Work with preceptor Care of a patient of alleged domestic abuse Care of the patient with an eye injury/complaint Work with preceptor Domestic Abuse booklet Work with preceptor Emergency Nursing Core Curriculum 5th Edition (pg. 467-486) Eye Injury/Complaint (cont.) Care of the patient with epistaxis Work with preceptor Emergency Nursing Core Curriculum 5th Edition (pg. 158-160) Care of the patient with a laceration Work with preceptor Emergency Nursing Core Curriculum 5th Edition (pg 661-677) Care for a patient requiring intubation Work with preceptor Work with RT ACLS Intubation (cont.) 23 Assist with spontaneous abortion: complete vs. incomplete Preceptor will confirm ability to: Accurately assist with a sexual assault case as outlined in NMH administrative policy. Preceptor will confirm ability to: Care for the patient as outlined in the NMH policy. Preceptor will confirm ability to: Anticipate and provide appropriate assessment/meds for eyes. Perform visual acuity exam Select the appropriate exam equipment Irrigate an eye Apply an eye patch Position patient at the slit lamp Recognize urgent vs. non-urgent eye conditions (welder burn, rupture vitreous, Foreign Body, Chemical Burns acid/alkaline.) Preceptor will confirm the ability to: Apply nose plug Verbalize difference between ant/post bleed, care and potential complications. Meds/medical condition affecting nosebleed. How to treat. Anticipate physician needs: - Select appropriate exam equipment - Set up prior to physician seeing patient Assist physician Preceptor will confirm ability to: Set up suture tray, sterile fields Assist physician: e.g. cut suture, maintain blood free field Ability to Control Bleeding Apply appropriate dressing Simple Complex: tube gauze, splint Support/distract etc. pediatric patients to facilitate a positive experience for the child and parent Appropriate restraints Suture removal/staple removal: - Identify healed vs healing - Identify infectious process Preceptor will confirm ability to: Locate intubation equipment Identify and know use of intubation equipment, including: - Magill forceps - Differentiate between straight and curved blades CO2 detector Confirm bilateral breath sounds Assist physician Correctly utilize bag-valve-mask devise Anticipate medications required, including RSI - COMPETENCY CHECKLIST 24 Appendix B Competencies for Resource Nurse in the Emergency Department Core Practice Competency #1 Assessment and Intervention Skills Assist with nursing tasks such as assessments, IV starts, discharges, admissions, and transfers Maintains a safe patient care environment using National Patient Safety Goals and Emergency Nurses Association (ENA) recommended practices. Has successfully completed the annual competency checklist at the proficient or expert level Core Practice Competency #2 Communication Skills Demonstrates excellent communication skills and teamwork behaviors Maintains customer service in accordance with the Behavioral Standards set by Allegan General Hospital Demonstrates effective conflict resolution skills Appropriately handles complaints and requests from waiting room patients and families Communicates with management, and physicians if necessary, when the department is at capacity Maintain confidentiality Assists with multiple agency coordination Core Practice Competency #3 Critical Thinking Skills Demonstrates the ability to work through complex situations Assists staff members in problem solving situations Assists in the management of patients requiring constant cardiac monitoring Assists in the management of trauma patients Demonstrates the ability to work with the different age populations Identifies urgent/emergent situations Implements protocol orders Identifies situations which require incident/occurrence reporting Reprioritizes patient care when unexpected events occur Manages acute changes in patients condition Demonstrates knowledge of interqual criteria for admissions Core Practice Competency #4 Human Caring and Relationship Skills Demonstrates effective interpersonal relationship skills Acts as a patient advocate Acts as a staff advocate COMPETENCY CHECKLIST 25 Utilizes feedback from peers in order to improve practice Provides emotional, psychosocial and spiritual support Provides culturally sensitive care Involves patient/significant other in developing plan of care Provides hourly rounding on active and waiting room patients Communicates with physician/designee regarding patient status using Situation-BackgroundAssessment-Recommendation (SBAR) communication Core Practice Competency #5 Management Skills Assists in setting goals and objectives for the team in a positive and respectful manner Manages overall function and through put of the department Rounds in each area of the emergency department Answers the Hospital Emergency Radio Network (HERN) radio and assigns Emergency Medical Service (EMS) beds pre-arrival based on acuity level Core Practice Competency #6 Leadership Skills Demonstrates leadership by helping to facilitate and implement change Demonstrates involvement in process improvement for the department and organization Demonstrates appropriate and efficient delegation Demonstrates and enforces regulatory compliance Acts as a role model and clinical resource Demonstrates appropriate use of chain of command Participates in quality initiatives Collaborates interdepartmentally Core Practice Competency #7 Teaching Skills Assesses individuals need for help Assists with Electronic Medical Record (EMR) Educates the patients in regards to specific discharge instructions Orients students from different disciplines to the environment Core Practice Competency #8 Knowledge Integration Skills Demonstrates clinical expertise and skills Stays abreast of best evidence based practices through continual research and lifelong learning Demonstrates appropriate use of American Nurses Association (ANA) principles for nursing staff according to the Scope and Standards for Practice COMPETENCY CHECKLIST 26 Appendix C Revised Resource Nurse Competency Checklist This document may be used for: o Orientation o Performance Updates o Annual Review FIRST PERSON (Resource) COMPETENCY LEVEL N-Novice Needs assistance of other user or manual to perform function. Follow rules/guidelines. AB-Advanced Beginner Performs function with minimal assistance, can describe function. Simple decision-making. C-Competent P-Proficient E-Expert (Expected level one year posthire) Comfortable, familiar with function. Consistently accurate in performing function. More complex decisionmaking. Similar to competent can perform with increased speed. Can demonstrate function to another. Comfortable with complex decisions. Able to teach another how to perform function. Understands how function affects other users of system. Able to mentor others. Preceptors to evaluate competence level, check appropriate boxes, initial, date and sign form. Return to manager or________________ when complete. This document will be stored in Unit Personnel file and reviewed annually. Signatures: Preceptor: _________________ Preceptor: _____________________ Preceptor: _____________________ Date: ____/_____/____ Date: _____/_____/______ Date: ____/______/______ Employee: _______________________________________ Date: ______/______/_ COMPETENCY CHECKLIST Performance Criteria Environment Order entry Care of the patient with a burn Care of the patient having a pelvic exam Care of the alleged sexual assault victim Learning Options 27 Evaluation Mechanism Through Observation and/or Demonstration Locate and correctly charge for supplies Locate Fire Extinguisher and exits Locate Eye wash station Locate Hazmat showers and decontamination trailer Determine what physician and ultrasound technician is on call from the call schedule list or SharePoint Preceptor will confirm ability to: Process and acknowledge CPOE orders electronically Enter verbal orders through CPOE Cancel orders through CPOE Completes Patient Supply charging and processing electronically Preceptor will confirm ability to care for a patient with a burn: Assessment of airway Fluid replacement Burn dressing(s) Verbalize special considerations for facial burns Splinting burns for maximum function after healing Recheck of a burn patient Consult the Burn Clinic for referrals Preceptor will confirm ability to: Assist with routine pelvic exam Select the correct culture media Assist with vaginal bleeding patient Assist with spontaneous abortion: - complete versus incomplete Obtain proper containers from lab for expulsion of the product of conception Preceptor will confirm ability to: Accurately assist with a sexual assault case as outlined in NMH administrative policy 0-120 Days Preceptor Name Date 121-240 Days Preceptor Name Date 241-365 Days Preceptor Name Date COMPETENCY CHECKLIST Performance Criteria Learning Options Care of the patient with epistaxis Evaluation Mechanism Through Observation and/or Demonstration Care of a patient of alleged domestic abuse Care of the patient with an eye injury/complaint 28 Consult appropriate agency(s) Preceptor will confirm ability to: Care for the patient as outlined in the NMH administrative policy Consult appropriate agency(s) Preceptor will confirm ability to: Anticipate and provide appropriate assessment/meds for eyes Perform visual acuity exam pre and post treatment Select the appropriate exam equipment Irrigate an eye - Saline irrigation - Morgan Lens irrigation - Eye wash station Apply an eye patch Position patient at the slit lamp Recognize urgent vs. non-urgent eye conditions (welder burn, rupture vitreous, foreign body, chemical burns acid/alkaline) Preceptor will confirm the ability to: Apply nose clamp Verbalize difference between ant/post bleed, care and potential complications Meds/medical condition affecting nosebleed. How to treat. - Use of Afrin spray to stop bleeding - Silver nitrate - Set up Rhino rocket Anticipate physician needs: - Select appropriate exam equipment - Set up prior to physician seeing patient Assist physician Monitor patient pre and post procedures for patent airway and hypotension crisis 0-120 Days Preceptor Name Date 121-240 Days Preceptor Name Date 241-365 Days Preceptor Name Date COMPETENCY CHECKLIST 29 Appendix D Student Evaluation of Resource Competency Checklist for Betty Sousley, MSN student Name ____9 Stakeholders___ Date _04/22/2013___ Please check the appropriate box for evaluating the questions. The numeric value is below the degree of comment. Comment section is available. Thank you for your time. Strongly disagree Goal 1: Continuous Quality Improvement 1 Disagree Agree 2 3 Goals for scholarly project were identified Objectives for scholarly project were identified Lack of clarity in the current resource competency checklist were identified Strongly agree Comments 4 9 No comments noted 1 8 No comments noted 3 6 No comments noted 2 7 No comments noted Goal 2: Function as a change agent and leader Resource competency checklist clearly identifies the COMPETENCY CHECKLIST 30 proficient and expert levels required The core competencies were clearly outlined 2 7 No comments noted The presenter had a good knowledge base of the topic 1 8 No comments noted The presenter was succinct in teaching the information 1 8 No comments noted The presenter has good communication skills 2 7 No comments noted Additional comments: Nice job, Betty! It was eye opening to see the differences in ER resource roles or lack of roles. The new checklist looks easy to modify for other departments. Thank you for your hard work. Great information! Excellent work Betty! Very nicely done! Well organized plan. A lot of information presented in a small amount of time. Enthusiastic! Strong knowledge of nursing in the E.D. and process flow along with challenges in providing care to the community. Excellent presentation, thought provoking and Betty offered strong workable solutions to difficult process changes. Appreciate the pertinent data and the wide range of resources utilized. Strengths: Betty had a good understanding of the entire subject matter. Teaching handouts were excellent. She showed minimal signs of nervousness while presenting. She gave good examples. Your goals to help strength the work environment with more defined roles, allowing for better pt/staff flow. Great List/competency/research. Obviously knew her topic well. Seemed very confident with what she was presenting. Betty is a confident public speaker. Good words, no word whispers, fluent, had your attention. COMPETENCY CHECKLIST 31 In depth understanding of the E.D. environment. Very organized. Aware of audience. Weaknesses: Having access to other Critical Access Hospitals to compare their process/workflow with current practices @ AGH or larger institutions. None, good job, good analysis of materials! For me, there was a slight confusion between a project identified as “resource competency checklist” and the broader subject of resource nursing roles in the department during the presentation. For example, if a recommendation is being made that the resource nurse not take assignments in order to accomplish the important resource tasks, this would be outside of the “checklist”. That being said, all of the information presented was well done and helpful. COMPETENCY CHECKLIST 32 Appendix E Preceptor Evaluation of Scholarly Project for Betty Sousley, MSN student Name: ___Phyllis Wilson____________ Date _____04/22/2013_______ Please check the most appropriate box for the evaluation. Thank you for your time. Strongly disagree Goal 1: Continuous Quality Improvements Met with the preceptor throughout the semester Goals and objectives for scholarly project were identified and established Identification of the lack of clarity in the current resource competency checklist was established Provided evidence of the progression of the scholarly project Supporting literature for scholarly project was identified Overall Core Competency VI: Continuous quality improvements in the nurse educator role were met. 1 Disagree Agree Strongly agree 2 3 Comments 4 X Met frequently in person, via telephone, and via e-mail X Shared very early on in the process X X Kept me up to date throughout the process X Clear presentation of all references X COMPETENCY CHECKLIST Goal 2: Functioned as a Change Agent and Leader Developed a resource competency checklist that clearly identifies the expert clinical experience and skills Met with Preceptor and CCO for final approval Resource competency checklist was sent to forms committee Presented resource competency checklist to stakeholders The information was presented in a succinct manner The presenter demonstrated leadership abilities The presenter demonstrated herself in a professional manner Overall the Core Competency V: Function as a Change Agent and Leader was met 33 X Very clear, easy to read and understand. X Shared information in a thorough presentation prior to group presentation X X X X X X Additional comments: Betty also made suggestions of how this new format could be applied, with modifications, to other areas of nursing. Very nice work. Strengths: It has been a pleasure watching Betty develop and mature into here educator role. Weaknesses: COMPETENCY CHECKLIST 34 Appendix F Self-Evaluation of Scholarly Project for Betty Sousley, MSN student Name: ___Betty Sousley, BSN, RN_________ Date ___04/22/2013______________ Please check the appropriate box for evaluating the questions. Comment section is available. The numeric value is below the degree of comment. Thank you for your time. Strongly disagree Goal 1: Integrate Core Competency V: Function as a Change Agent and Leader (NLN, 2005) 1 Disagree Agree 2 Strongly agree 3 Comments 4 Compose resource nurse competency checklist X The checklist Meet with Preceptor and manager for feedback and approval X Had frequent meetings and conversations with preceptor, manager, and CCO Present final proposed resource competency checklist to preceptor and CCO prior to presentation for feedback X See comments on preceptor evaluation form. Present resource competency checklist to stakeholders X This went better than I had anticipated. COMPETENCY CHECKLIST 35 Goal 2: Integrate Core Competency VI: Pursue continuous Quality Improvements (NLN, 2005) Define lack of clarity in the current resource competency checklist. Provide evidence of support through research for a standardized competency checklist. Implement and institute changes to the resource nurse competency checklist X X I think I could have done a better job in this area. I continued to vacillate between the role of the resource nurse and the competency checklist. I did not stay focused on the competency checklist until I received my feedback from my draft and the stakeholder evaluations. X X This has to be presented to the medical executive committee for approval and then the forms committee. Additional Comments: The feedback was helpful in identifying areas of improvement and changes that will require adjustments. . Strengths: I knew what I was looking for during the research project, therefore I was able to identify the common threads and integrate those into the core practice competencies and expand on the way in which we practice at AGH. I know the workflow and responsibilities assigned to the resource role and was facilitated me with meeting my objectives. Weaknesses: Staying focused on the topic. The topic was not the responsibilities of the resource role; it was the competency checklist for the resource nurse.