Cecil 40 [4-20
advertisement

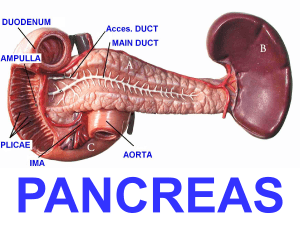
Cecil’s Chapter 40: Diseases of the Pancreas The head of the pancreas is nestled in the C loop of the duodenum, and the tail extends posterior the stomach toward the spleen The pancreas has acinar cells and islet cells: - Acinar cells are about 95% of the pancreas, and islet cells are only 1-2% Islet cells – endocrine pancreas that makes – insulin, glucagon, somatostatin, and pancreatic polypeptide Acinar cells – make up the exocrine pancreas o Exocrine pancreas also includes the ductal epithelial cells o Acinar cells make proteolytic digestive enzymes, which get packaged in the golgi into vacuoles, and then go as inactive zymogens to the apical cell, and then discharged into the duct by exocytosis The ductules keep adding together to form larger ducts, before joining the duodenum at the ampulla of Vater Small bowel enterocytes activate the inactive zymogens by secreting enterokinase - Trypsinogen gets converted to trypsin by enterokinase, and becomes the trigger enzyme to convert the other enzymes into their active forms Lipase, amylase, and ribonucleuse are secreted already active The duct cells secrete mainly water and electrolytes, which decreases the viscosity of the protein-rich acinar secretions, and alkalinzes gastric contents emptied into the duodenum to levels at which the pancreatic enzymes become catalytically active (pH 3.5-4) Pancreas development: - At 4 weeks gestation, the dorsal pancreas forms from the duodenum, and shortly after the ventral pancreas then forms from the hepatic diverticulum At 7-8 weeks, the duodenum rotates so that they’re close to each other, and their main ducts start to fuse o If fusion is incomplete, the duct of wirsung drains only the ventral pancreas through the major ampulla, and the duct of santorinin drains the dorsal pancreas (most of the pancreas) through the small accessory ampulla Called pancreas divisum – seen in 5-10% of people Can cause acute and chronic pancreatitis Acute pancreatitis – acute inflammation of the pancreas, that can be reversed - Page 446 – pancreas anatomy Most cases are mild and they recover with normal pancreas function - - - - - - 10-20% of cases, the inflammation leads to systemic inflammatory response syndrome (SIRS) o SIRS can cause multiple organ issues, or pancreatic necrosis The initiating event in acute pancreatitis is conversion in the acinar cells, of trypsinogen to trypsin, causing acute intracellular injury, autodigestion of the pancreas, and lots of systemic issues if the activated enzymes get leaked into the blood o Initiating events to trigger this could be obstruction of the pancreatic duct, overdistention of the pancreatic duct, reflux of bile or duodenal juices into the pancreatic duct, changes in permeability of the pancreatic duct, ischemia of the pancreas, and toxin caused cholinergic hyperstimulation o Gallstones causes half of cases of acute pancreatitis, alcohol causes 1/3 o Page 447 – pic showing the chain of things happening to cause acute pancreatitis Clinical manifestations of acute pancreatitis: o Abdominal pain is almost always seen in acute pancreatitis The pain often radiates to the back, and is usually worse when supine The pain is often unbearable, and continues without relief for more than a day o Physical exam shows severe upper abdominal tenderness, along with sometimes guarding o Ilieus happens when the inflammatory process extends into the small intestine and colon o Other signs are nausea, vomiting, fever (from inflammatory process and release of cytokines) The release of the pancreatic enzymes into the surrounding body can cause chemical irritation, and can add to loss of proteins in fluid, hypovolemia, and hypotension o If they get into systemic blood, they can add to subcutaneous fat necrosis, hurt organs, and cause shock, renal failure, and respiratory insufficiency Hemorrhagic pancreatitis can sometimes show Grey Turner sign (ecchymosis (ruptured blood into subcutaneous skin aka bruise) of the flank) or Cullen sign (ecchymosis in the periumbilical area) Metabolic problems in acute pancreatitis include hypocalcemia, hyperglycemia, and acidosis o Hypocalcemia in acute pancreatitis is most often caused by hypoalbuminemia Trypsin can activate plasminogen to plasmin, causing clot lysis, but trypsin can also activate prothrombin to thrombin, causing thrombosis Fluid can accumulate around the pancreas as it leaks out of it, more often in serous pancreatitis Pancreatic pseudocysts – encapsulated collections of pancreatic juice o The fluid must have been there at least a month from the onset of pancreatitis to be called a pseudocyst o Most pseudocysts are asymptomatic o Symptoms, if any, can include abdominal pain, early satiety, nausea, and vomiting due to compression of the stomach o The pseudocysts can enlarge and damage stuff around them o - - - Most pseudocysts will resolve, but if they get big or might get infected, you can drain them Diagnosing acute pancreatitis o Needs 2 of these 3 things: Abdominal pain characteristic of acute pancreatitis Serum amylase or lipase more than 3 times higher than normal Characteristic findings of acute pancreatitis on computed tomography (CT) scan o Increased pancreatic enzymes is NOT used to diagnose cause it can happen in so many other things as well o The serum amylase and lipase rise rapidly, can stay high for 3-5 days, and lipase stays high longer than amylase, so the lipase is more helpful when the patient delays coming in Monitoring the amylase and lipase or seeing HOW high they are aren’t very helpful or reflect the severity of the pancreatitis o Positive CT’s for pancreatitis would be enlarged pancreas, inflammatory changes around the pancreas, and fluid collections outside the pancreas o When liver tests are elevated, especially aspartate aminotransferase (AST) that’s 3 times higher than normal, it suggests acute gallstone pancreatitis ¾ of acute pancreatitis cases will resolve with just supportive therapy o The other ¼ develop a complication 1/3 of them will die Early deaths within the first 2 weeks are from multisystem organ failure caused by release of inflammatory mediators and cytokines Late deaths are from infection o Ranson criteria of severity - page 449 Higher the score, the more likely it is to be severe, prolonged, and fatal Mortality is about 1% with less than 3 Ranson signs, 10-20% when there’s 3-5 signs, and more than 50% when 6 Ranson signs exist APACHE 2 test scores of over 8 also indicate severe pancreatitis Interstitial pancreatitis – characterized by an intact microcirculation, and uniform enhancement of the pancreas on contrast-enhanced CT scan Necrotizing pancreatitis – characterized by disruption of the pancreatic microcirculation so large that it makes large spots not enhance on CT o 20-30% of acute pancreatitis o Necrotizing pancreatitis has a worse severity, especially when the necrotic tissue gets infected Infection happens in 1/3-1/2 of necrotizing pancreatitis, but less than 1% of interstitial pancreatitis The mortality rate for infected necrosis is 30%, causing 80% of acute pancreatitis deaths Infection is suggested when there is fever, leukocytosis, and organ failure - You diagnose the infection with a percutaneous CT-guided needle aspiration, and then do gram stain or culture If they have an infection, surgery is needed Treating acute pancreatitis – supportive therapy, especially if you’re gonna rest the pancreas by withholding oral nutrition intake – so give nutrition through IV Chronic pancreatitis – inflammation of the pancreas that causes irreversible damage - - - - Chronic pancreatitis is classified as obstructive or nonobstructive o The most common nonobstructive cause is chronic alcoholism o If they aren’t alcoholics, the next most common cause is idiopathic (cystic fibrosis) o Gallstones are the major cause of acute pancreatitis, but almost never lead to chronic pancreatitis Alcoholic pancreatitis is caused by abnormal secretion and necrotic fibrosis of the pancreas o Chronic alcohol ingestion causes hypersecretion of protein from acinar cells, increased secretion of calcium, defects in duct bicarb secretion (which then decreases the solubility of secreted proteins), and decreased release of lithostathine (a protein that inhibits calcium carbonate crystal formation This all leads to favorable conditions for calcium-protein complexes, which then plug and obstruct the ducts The obstruction then leads to further destruction of duct cells and acinar cells o Alcohol may also be toxic to acinar cells, causing damage that causes necrosis followed by fibrosis, which causes obstruction Hereditary pancreatitis – the gene for trypsinogen is mutated so that protective inactivators in the pancreas can’t inactivate trypsinogentrypsin Chronic pancreatitis shows pain, and sometimes steatorrhea, diarrhea, and weight loss o Sometimes can show exocrine or endocrine issues, or be asymptomatic o Steatorrhea only happens when lipase release is less than 10% of normal o Diabetes is a late complication of chronic pancreatitis, only after 80-90% of the pancreas is damaged o Chronic pancreatitis can cause pseudocysts, fistulas, obstruction, cancer, small bowel bacterial overgrowth, and gastric varices from splenic vein thrombosis Diagnosing chronic pancreatitis – tests on pancreas structure and function o Lots of structural changes usually, but not always, correlate with severe functional impairment o Tests for pancreas structure: Findings that suggest chronic pancreatitis: Duct abnormalities – dilation, stones Parenchymal abnormalities – calcification, atrophy, not homogenous Pancreas contour changes Pseudocysts o o The first diagnostic test you should do if you suspect pancreatitis is plain film radiography, to look for calcifications ERCP and endoscopic ultrasound (EUS) are the most sensitive imaging studies of the pancreas ERCP can cause acute pancreatitis though Tests for pancreas function: The secretin stimulation test is the gold standard functional test for diagnosing chornic pancreatitis Also, bicarb making will be impaired in early chronic pancreatitis The 72-hour fecal fat determination is the gold standard to document steatorrhea Fecal fat greater than 7g per 24 hours = steatorrhea Low trypsinogen indicates exocrine pancreas acinar cells aren’t working Treating chronic pancreatitis: Treating with enzymes can help malabsorption, and is indicated if they lose more than 10% of their body weight, excrete more than 15g of fat per day in their stool, or have dyspepsia Most enzyme preparations have pancreatin, which is pig pancreas extract that has amylase, lipase, trypsin, and chymotrypsin Enzyme supplements aren’t absorbed from the GI, and are instead inactivated by gut bacteria or digestive secretions, and then pooped out Acid-stable encapsulated pancreatic enzymes are more effective enzyme supplements for chronic pancreatitis When gastric hyperacidity is present, proton pump inhibitors or histaminereceptor antagonists should be used to delay enzyme inactivation May have to take fat soluble vitamins if they have maldigestion and steatorrhea Medium chain tryglycerides (MCT’s) don’t need lipase to break them down in order to be absorbed If enzyme supplements don’t work, decrease their dietary fat to less than 50g per day, and substitute with MCT’s Pain relief can be helped by analgesics, and pancreas enzyme supplements, and avoiding alcohol Enzyme supplements decrease cholecystokinin-mediated pancreatic secretion, which can relieve the pain Surgical duct drainage along with lateral pancreaticojejunostomy (Puestow procedure) may decrease pain in about 80% of patients o Safe with low mortality, but the pain relief only continues for 5 years in half of patients Pancreas cancer – pretty common - Poor prognosis – less than 1/5 of patients survive a year - - - Most pancreas tumors are adenocarcinomas from duct cells Risk factors for pancreas cancer are age, being male, carcinogens, cigarettes, hereditary pancreatitis, chronic pancreatitis, and maybe high fat diets Common presenting signs and smptoms of pancreas cancer include jaundice, weight loss, and abdominal pain o The pain is usually constant, and radiates to the back o Most pancreas cancers start in the pancreas head, causing obstructive jaundice, or a large palpable gallbladder (called Courvoisier sign) o Curable lesions most often present with painless jaundice CT and MRI are the best first tests to look for a pancreas mass The major thing deciding if you can remove the tumor and survival is if the tumor invaded the vascular system, or metastasized o most pancreas tumors can’t be removed by surgery Treatment of pancreas cancer is the Whipple surgery operation