pancreas - Caangay.com
advertisement
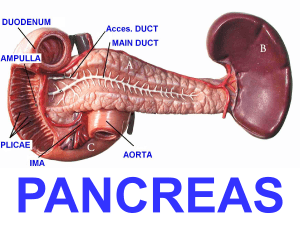
I. Pancreas A. Anatomy - retroperitoneal - extends transversely behind the stomach - weight – approximately 85 grams - length – 12-15 cm. 1. Anatomic relationships a. head of the pancreas – lies over the aorta and under the stomach and transverse colon, posteromedial to the IVC i. superior limit – portal vein ii. anterior limit – gastro-duodenal artery iii. CBD courses posteriorly to the head and partially within iv. Common blood supply with the duodenum b. uncinate process – lies posterior to the SMV and anterior to the IVC c. tail – closely related to the spleen d. neck – lies at the confluence of splenic and mesenteric veins B. Blood supply 1. Anterior and posterior arcades – supply the head of the pancreas; superior component comes from the gastroduodenal artery and the inferior component comes from the superior mesenteric artery 2. Inferior pancreatic artery –runs inferior to the organ, in intimate contact with the pancreas 3. Superior pancreatic artery – present 50%-90% of patients a. arises from the splenic artery, hepatic artery, superior mesenteric or iliac artery b. postero-superior portion of the neck and body of the pancreas 4. Splenic and left gastroepiploic artery – supplies body and tail of the pancreas in 5. Venous drainage a. follows the course of the arteries b. confluence of right gastroepiploic vein, anterosuperior pancreaticoduodenal vein, middle colic vein c. forms the gastrocolic trunk which empties directly to the SMV at the inferior border of the neck of the pancreas 6. Ductal system – drains into the duodenum a. Duct of Wirsung – empties into the ampulla of Vater together with the CBD b. Duct of Santorini – drains into the minor papilla approximately 2 cm above and medial to the ampulla of Vater (minor ductal system) II. Pancreatitis A. Acute pancreatitis 1. Gallstone pancreatitis a. needs a common channel between the CBD and the pancreatic duct b. high proportion of causes with gallstone pancreatitis have recoverable biliary calculi in the stools c. spasm of the sphincter of Odi as a stone passes causes reflux of bile into the pancreatic duct which results in the destruction of the pancreatic parenchyma 2. Alcohol pancreatitis a. alcohol causes increase in protein concentration in the pancreatic juice calcifications in duct b. ductal obstruction causes inflammation destruction of parenchyma the 3. Post-operative pancreatitis a. occurs ususally after gastric, biliary tract surgery, or splenectomy b. ligation or laceration of the duct may be the cause of the pancreatitis c. mortality – approximately 50% B. Clinical manifestations of acute pancreatitis 1. mild abdominal discomfort to profound shock 2. epigastric pain radiating to the back nausea and vomiting with 3. discomfort may be relieved by sitting and aggravated by lying down 4. may have mild to moderate abdominal tenderness 5. may present with a surgical abdomen 6. severe pancreatitis may lead to retroperitoneal hemorrhage which leads to a. 3rd space fluid loss b. hypovolemia c. hypotension d. tachycardia e. blood dissection– Grey Turner’s sign (flank ecchymosis) - Cullen’s sign (periumbilical ecchymosis 7. pain usually follows 1-4 hours after a heavy meal and intake of alcohol C. Diagnosis 1. History and Physical Exam a. serum amylase – increased in 95% of cases; 5% false negative i. 75% of patients with abdominal pain and increased amylase have pancreatitis ii. other causes of increased amylase - acute cholecystitis - CBD stone with or without cholangitis - Perforated peptic ulcer - Strangulated small bowel - acute alcoholism - Cancer of the pancreas - Mumps iii. amylase level over 1,000 Somogyi-Nelson units often indicates biliary tract disease with panceatitis iv. 200-500 units indicates alcoholic pancreatitis b. amylase – creatinine ratio - diagnostic when amylase output in the urine exceeds 300 u in one hour and ratio of amylase:creatinine clearance of >5 c. serum calcium - <7.5 mg/dl generally indicates poor prognosis d. radiology (x-ray) – relatively insensitive e. barium studies – i. widened duodenal C-loop ii. Pad sign – obliteration of the duodenal mucosal folds f. ultrasound – swelling of the pancreas and loss of tissue planes g. CT scan – findings similar to ultrasound but with a higher resolution D. Treatment 1. Resuscitation – replacement of fluid losses and electrolytes 2. Blood transfusion in hemorrhagic pancreatitis 3. Calcium gluconate through IV 4. NGT suction – decrease GIT and pancreatic stimulation distension 5. Antibiotics – reduce risk of abscess formation 6. Meperidine 7. Surgery a. confirm diagnosis in cases which do not respond medically b. relieve ductal obstruction c. drain the lesser sac E. Prognosis – Ranson’s Criteria 1. Admission a. > 55 years old b. WBC count > 16000 c. FBS > 200 mg/dl d. LDH > 350 units/ml e. SGOT > 250 2. 48 hours after admission a. drop in hematocrit by > 10% b. increase in BUN of 5 mg/dl c. calcium level < 8 mg/dl d. PaO2 below 60 mmHg e. base deficit > 4 meq/L f. third space fluid loss > 6 L *Prognosis Number of criteria present 0-2 Mortality rate 0.9% 3-6 33% 7-8 100% III. Chronic Pancreatitis - clinical entity rather than a pathologic process - organ becomes small, indurated and nodular and edges become rounded - alternating areas of strictures and dilatations in the duct with calcifications -primary etiology: chronic alcoholic pancreatitis with progressive fibrosis without ductal dilatation or calcification A. Clinical manifestation 1. late 30’s or 40’s 2. history of alcoholism and recurrent attacks of pancreatitis 3. pain 4. may diabetes or steatorrhea 5. frequent finding of pseudocyst 6. anorexia and weight loss B. Diagnosis 1. upper GI series 2. ERCP 3. ultrasound/CT scan 4. calcifications on x-rays C. Treatment 1. analgesics 2. endocrine and exocrine replacement 3. stop alcohol intake 4. surgery (Peustow procedure) IV. Psedocyst of the Pancreas A. Causes 1. pancreatitis – 75% - alcoholic pancreatitis - 4th and 5th decade of life 2. trauma – 25% B. Pathology 1. fibrous wall surrounding a collection of pancreatic juice and necrotic or suppurative pancreatic juice 2. unilocular and located in the lesser sac 3. fluid varies from clear and colorless to brown or green C. Clinical manifestations 1. pain, fever, and ileus appearing 2-3 weeks after an initial attack of pancreatitis 2. pain radiating to the back 3. jaundice d. non-tender palpable mass – (75% of patients) 4. change in size of the mass due to partial drainage D. Diagnosis 1. continued elevation of serum amylase 2. CT scan – diagnostic tool of choice 3. ultrasound 4. upper GI series 5. ERCP E. Treatment 1. surgery a. to prevent complications such as infection, hemorrhage, rupture b. pseudocysts rarely resolve once thick fibrous wall has developed c. pseudocyst should be treated only after 5-6 weeks from discovery 2. types of surgery a. external drainage b. internal drainage - best i. cystenterostomy ii. cystgastrostomy c. cyst wall should be excised for histopathology to rule out malignancy V. Pancreatic Tumors A. Etiology 1. cigarette smoking 2. coffee 3. biliary lithiasis B. Pathology 1. Cystadenoma/Cystadenocarcinoma a. rare; predilection for females b. cystic spaces divided by firbous septa; vascular c. better prognosis than adenocarcinoma d. Tx. - resection 2. Adenocarcinoma a. 90% of cases; usually at the head b. periampullary malignancy i. head of the pancreas – 83% ii. Ampulla of Vater – 10% iii. Duodenum – 4% iv. Common bile duct – 3% c. Clinical manifestations i. weight loss – most common ii. pain – dull epigastric pain that radiates to the back; aggravated by eating iii. progressive jaundice – 75%; head of the pancreas iv. anorexia and weakness – 50% v. pruritus vi. hepatomegally vii. enlarged palpable gallbladder – Courvesiure’s gallbladder d. Laboratory work-up i. alkaline PO4, transaminases, Bilirubin ii. UGIS iii. CT scan – CT scan guided biopsy iv. ERCP/PTC e. Treatment i. Prior to surgery – improve overall condition of the patient ii. Whipple’s surgery – for resectable lesions – renal failure most common complication iii. Cholecystojejunostomy/ Gastrojejunostomy – bypass for unresectable lesions iv. injection of 95% alcohol to the celiac plexus – relief of pain v. poor risk patients - PTC/PTBD - 5-FU/external beam radiation 3. Zollinger-Ellison Sybdrome – Ulcerinogenic Tumors of the Islets a. male>female; 3rd to 4th decade b. slow growing tumor of the Islets of Langerhan c. associated with Multiple Endocrine Neoplasia – adenoma of the pituitary, parathyroid, pancreatic islets (beta cells), and adrenal cortex d. secretes GASTRIN e. Triad i. fulminant and complicated peptic ulcers often in atypical locations ii. Extreme gastric hypersecretion iii. Non- beta cell tumor of the Islets f. signs and symptoms i. acid peptic disease ii. Distressing watery diarrhea iii. steatorrhea g. diagnosis i. UGIS ii. Gastroscopy iii. Serum gastrin determination iv. CT scan h. treatment i. total gastrectomy ii. Resection of the tumor iii. Proton pump inhibitor iv. Streprozotocin - metastasis 4. Hyperinsulinism – Islet cell tumor - b-cells – hypersecretion of insulin causing hypoglycemia a. pathology i. benign adenoma – 75% ii. Suspected malignant – 13% iii. Clearly malignant – 12% iv. Diffuse adenomatosis v. size of the tumor has no relation to severity b. clinical manifestation i. 4th-7th decade ii. Associated with MEA-I hyperinsulinism iii. Two general forms - rapid fall of blood sugar - gradual fall in blood sugar iv. Whipple Triad - hypoglycemic attack during fasting or exertion - FBS > 50 mg/dl - symptoms relieved by intake of glucose c. diagnosis i. blood sugar and insulin levels ii. Pancreatic angiography and venous sampling iii. CT scan d. treament i. pre-operative management - adequate provision of glucose - ACTH and Cortisol - Diazoxide – inhibits release of insulin ii. Surgery - benign – excision - malignant – pancreatic resection - improvement seen 30 minutes after excision of the lesion - Streptozoticin - metastasis