Understanding Injecting Drug Use
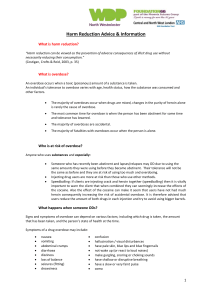
advertisement

UNDERSTANDING INJECTING DRUG USE Various routes through which drugs can be taken Only very few drugs can be taken through oral route In general oral route is one of the least efficient route of drug intake since A lot of drug is destroyed before it reaches the brain It takes substantially longer for the drug to reach the brain and exert its effects However, oral route is also least harmful for taking drugs, in general Oral Various routes through which drugs can be taken •Drug reaches the blood circulation through lungs and then onwards to the brain fairly early •This route is harmful as it damages the linings of the lungs and can give rise to various respiratory diseases Smoking Various routes through which drugs can be taken •The most efficient route of drug intake •Drug reaches brain fairly quickly and gives sudden effects •Requires much less amount of drug (hence cheaper) •Most damaging or harmful route of taking drugs Injecting Common drugs injected in India Heroin (pure/white heroin/ ‘No. 4’): mainly in the northeastern states. Heroin (Smack / brown sugar): not readily injectable as it comes in the form of crude, impure powder. • Before injecting, a user has to prepare or ‘cook’ the drug. • Most users mix the powder with an injectable sedative drug (like chlorpheniramine), boil it, filter it with a cotton swab and then inject it. Buprenorphine (Tidigesic/Norphine) or pentazocine (Fortwin): probably the most popular drugs for injecting among IDUs in India. • Most users mix them with one or more of the following sedatives for enhancement of the effects: • Diazepam (calmpose), • Chlorpheniramine (Avil), • Promethazine (Phenargan). Dextrprpoxyphene (Proxyvon / Spasmo- Proxyvon / SP): available as capsules and NOT AS INJECTIONS. • Users open the capsules, take the powder out, mix it with another liquid / drug and then inject it. • Seen only in the northeastern states, very rare in other parts of the country INJECTING DRUG USE IN INDIA History Opioids in modern India 8 Early 1980s: Opium replaced with heroin Rural areas: Opium users continued with Opium, some switched to heroin Urban areas: Heroin use started spreading Opium in modern India 9 India’s proximity to ‘Golden Triangle’ and ‘Golden Crescent’ Opioids in modern India 10 Early 1990s: Injecting Drug Use started in North East India; gradually spread to other parts IDU in India Currently, India figures among the developing and transitional countries with the “largest populations of IDUs”. The National AIDS Control Organisation estimates that currently there are about 2 Lakh IDUs in India. HIV among IDUs in India the HIV among IDUs is also progressing in India at an alarming rate. At the national level IDU is the vulnerable group (among other vulnerable groups such as Female Sex Workers and Men-Who-Have-Sex-with-Men) which has highest prevalence of HIV. The states / areas particularly affected by HIV among IDUs are: Manipur, Nagaland, Mizoram, Punjab, Chandigarh, Delhi, Kerala, Tamil Nadu and parts of Orissa, Bihar, and UP. HIV estimates in India, 2008 HIGH-RISK GROUPS: IDU – high prevalence (NACO ,2007) The usual drug use career Prescription by a doctor Injection Tidigesic / Fortwin Heroin / Smack Charas / Ganja Alcohol / Tobacco Pain Profile of a usual IDU Most vulnerable: underprivileged section of the Society IDUs catered to by an IDU TI: belong to poorest section of the society The typical IDU A man, in his productive years, but not likely to be regularly and gainfully employed. May be married, but likely to have poor social support. Severe dysfunction in almost all aspects of his life. Profile of a usual IDU Also likely that a IDU TI will encounter IDUs who are: Thus, IDU would require help regarding poor, homeless, may have limited means to sustain themselves, to maintain their hygiene, or even to have two square means a day. In conflict with law high-risk behaviours many other areas of life. Exceptions, i.e. atypical IDUs which may require attention Women IDUs, IDUs belonging to better socio-economic strata, holding white collar jobs and staying with their families IDUs which are also other HRG members (FSWs, MSM etc.) Injecting practices When injections are administered in a health-care setting usual aseptic precautions Location: clean and hygienic. The area to be injected: thoroughly cleaned with a disinfectant, Body parts: safe for injecting Injecting equipment: sterile needle and syringe After injecting: the site is pressed with a clean cotton swab for few seconds (to prevent bleeding). For IDUs not possible to maintain aseptic precautions Location: hidden from public (parks, public toilets, unused buildings or open spaces, garbage dumps, near the drains and nullas etc. ) The area to be injected: not usually cleaned Body parts: Unsafe parts of body such as groin / thigh or neck Injecting equipment: reuse or sharing Sharing Which of the following YOU can share with a friend of yours? A towel / napkin A plate of food A spoon A glass for drinking a beverage A dress Undergarments Toothbrush Sharing Injecting is very often a group activity The sharing may involve: Sharing needles Sharing Syringes Sharing injecting paraphernalia (i.e. the cookers or pots in which drug has been prepared for injecting). Why do IDUs share? Economic reasons: Unavailability of injecting equipments - the drug may be procured from a drugpeddler, but the injecting equipment may be available only at a pharmacy, which may be reluctant to sell needles-syringes or may choose to sell them at a premium. Psychological reasons: Sometimes IDUs may choose to share their injecting equipments, just because they feel their bonding with each other will be strengthened by this act. Poor awareness: of consequences of sharing or of safe injecting practices also contributes to risky practices Risks of sharing Transmission of blood borne infections such as HIV HBV HCV Risks of Injecting Risk of local (injection site) infections like Thrombophlebitis (blocked veins), abscess, gangrene, amputation etc. Risk of spread of local infection to other parts of body like septecemia, endocarditis, etc. Risk of accidental injury to arteries leading to severe bleeding Risk of spread of blood borne infections like HIV, Hep-B and Hep-C Risk of overdose and Toxicity