Chapter 7
advertisement

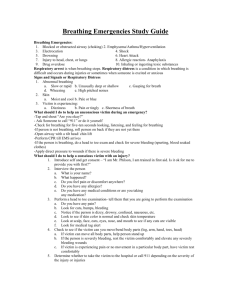
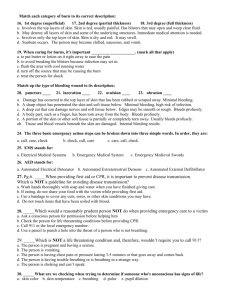
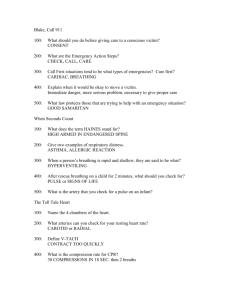
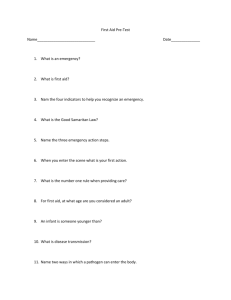
Chapter 7 Before Providing Care and Victim Assessment Bloodborne Pathogens Bacteria and viruses present in blood and body fluids that can cause disease in humans. Bacteria and viruses MOST COMMON forms of pathogens Found almost everywhere in our environment. Bacteria vs. Viruses BACTERIA Live can live outside of the body Commonly do NOT depend on other organisms of life Antibiotics and other medications often are used to treat the infection VIRUSES Depend on other organisms to live Once viruses are in the body, they are difficult to kill Prevention is CRITICAL Hepatitis B Liver infection caused by the hepatitis B virus. Severe or even fatal can be in body for up to 6 months before symptoms appear. Prevention: Hepatitis B vaccine (3 doses) Primarily spread through direct or indirect contact with infected blood or other body fluids Hepatitis C Liver disease caused by the hepatitis C virus Most common chronic bloodborne infection in US No vaccine against hepatitis C and NO treatment available to prevent infection after exposure Leading cause of liver transplants Primarily spread through direct or indirect contact with infected blood or other body fluids HIV Virus that causes acquired immunodeficiency syndrome (AIDS) Weakens the body’s immune system People with AIDS eventually develop life-threatening infections and can die from these infections. Currently NO vaccine against HIV Primarily spread through direct or indirect contact with infected blood or other body fluids How Pathogens Spread For any disease to be spread, ALL four of the following conditions must be met: 1. A pathogen is present 2. A sufficient quantity of the pathogen is present to cause disease 3. A person is susceptible to the pathogen 4. The pathogen passes through the correct entry site (eyes, mouth other mucous membranes; non-intact skin or skin pierced by needle sticks, human bites, cuts, abrasions and other means) How infections occur Present Entry Site Quantity Susceptible Direct Contact Occurs when infected blood or body fluid from one person enters another person’s body at a correct entry site. Example: *Infected blood splashing in the eye *Directly touching the body fluids of an infected person and that infected blood or other body fluid enters the body through a correct entry site Indirect Contact Occurs when a person touches an object that contains the blood or other body fluid of an infected person and matter enters the body through a correct entry site. Example: *Soiled dressings: when a person picks up blood-soaked bandages with bare hands and the pathogens enter through a break in the skin on the hand. *Equipment and work surfaces that are contaminated Droplet Transmission Occurs when a person inhales droplets from an infected person’s cough or sneeze Example: Flu Vector-Borne Transmission Occurs when the body’s skin is penetrated by an infectious source, such as an animal or insect bite or sting Example: *Malaria *West Nile Virus Risk of Transmission Very low but should be very cautious Neddlestick or cut exposure 30% chance if unvaccinated person for Hep B (depending on several factors) Risk of hep c is about 2% Risk of HIV infected blood less than 1% OSHA Occupational Safety and Health Administration “issue regulations about on-the-job exposure to bloodborne pathogens” Exposure Control Plan Written program outlining the protective measures that employers will take to eliminate or minimize employee exposure incidents. Standard Precautions Personal protective equipment (PPE) Good hand hygiene Engineering controls Work practice controls Proper equipment cleaning Spill clean-up procedures Personal protective equipment (PPE) Breathing barriers Non-latex disposable gloves Gowns Masks Shields Protective eyewear Guidelines for using PPE to prevent infection: Avoid contact w blood and other body fluids Use CPR breathing barriers when giving ventilations Wear disposable gloves when providing care Recommended Protective Equipment against Hep B, Hep C, and HIV transmission in prehospital settings Disposable Gloves Gown Mask Protective Eyewear Bleeding control with spurting blood Yes Yes Yes Yes Bleeding control with minimal bleeding Yes NO NO NO Emergency childbirth Yes Yes Yes Yes Oral/nasal suctioning; manually clearing airway No No No, No, unless splashing is likely unless splashing is likely Handling and cleaning contaminated equipment and clothing Yes No NO No, unless soiling is likely Good hand hygiene Most effective measure to prevent the spread of infection Wash hands frequently (for at least 15 seconds) Engineering controls objects used in the workplace that isolate or remove a hazard Biohazard bags and labels Personal protective equipment Sharps disposal containers Self-sheathing needles Safer medical devices Work practice controls- things done to help reduce the risk Placing sharp items in puncture-resistant containers Avoiding splashing, spraying, and splattering of droplets of blood Removing and disposing of soiled clothing Cleaning and disinfecting all equipment Washing hands thoroughly with soap and warm water immediately Not eating or drinking, smoking, applying cosmetics or lip balm, handling contact lenses, or touching the eyes, mouth or nose when in an area where exposure to infectious materials is possible Isolating contaminated areas so other employees or people do not walk through and become exposed Equipment cleaning and Spill-clean up procedures Always clean and disinfect the equipment and surfaces used Wear disposable gloves and other personal protective equipment when cleaning up spills Clean up spills immediately or as soon as possible after the spill occurs Dispose of the absorbent material used to collect the spill in a labeled biohazard container Flood the area with fresh disinfectant solution of approximately 1 ½ cups of liquid chlorine bleach to 1 gallon of water and allow to stand for about 10 minutes Use appropriate material to absorb the solution, and dispose of it in a labeled biohazard container Scrub soiled boots, leather shoes, and other leather goods, such as belts, with soap, a brush and hot water. If a uniform is worn to work, was and dry it according to the manufacture's instructions. If you are exposed Clean the contaminated area thoroughly with soap and water If you are splashed with blood or other potentially infectious material around your mouth or nose, flus the area with water. If your eyes are involved, irrigate them with clean water, saline for 20 minutes Report the exposure incident Document what happened (include time date) Seek immediate follow-up care General Procedures for injury or sudden illness on land 1. Size up the scene Move victim only if necessary for his or her safety 2. Perform a primary assessment Obtain consent if the victim is conscious. 3. Summon EMS, if needed 4. Perform secondary assessment, if no life-threatening conditions are found. 5. Provide care for the conditions found. 6. Report, advise, and release Size up the Scene: Determine if the scene is safe for LGs, other rescuers, victim(s) and bystanders • Use your senses to check hazards (gas leak or fire, look for things explosion) Determine what caused the injury or illness Determine the number of injured or ill victims Determine what additional help may be needed Put on the appropriate PPE Moving a victim victim on land move only: You are faced w immediate danger You need to get to other victims who have more serious injuries or illnesses It is necessary to provide appropriate care (stairs) Moves Non-emergency moves Walking assist: one or two responders conscious person who simply needs assistance Two-person seat carry: requires a second responder. Conscious person no serious injury Moves Emergency moves: Clothes drag: conscious or unconscious person suspected of having a head, neck, or spinal injury Pack-strap carry: Ankle drag: conscious and unconscious (foot drag) to move a person who is too large to carry or move in any other way. Perform an initial assessment: to identify any Life-threatening conditions Checking the victim for responsiveness A person who speaks is CONSCIOUS Breathing and pulse Scanning for severe bleeding Continue sudden illness on land Perform Secondary assessment To identify additional conditions Only do it if you know that there are no life-threatening conditions To gather additional info about injuries or conditions that may need care Not life-threatening but could be if not cared for Summon EMS if any of the following conditions are found: Unconsciousness or altered level of consciousness (LOC) “confusion or drowsiness” Breathing problems (difficulty or no breathing) Persistent abdominal pain or pressure Any victim recovered from underwater who may have inhaled water Chest pain, discomfort, or pressure lasting more than a few minutes or goes away and comes back No pulse Severe external bleeding Vomiting blood or passing blood Severe (critical) burns Suspected poisoning Seizures in the water Seizures that last more than 5 minutes or cause injury Suspected or obvious injuries to head, neck or spine Stroke Painful, swollen, deformed areas (broken bones) or open fracture Victim's physical condition is unclear or is worsening (allergic reaction) Open the Airway and check for breathing and Pulse No more than 10 seconds Perform concurrently If able to speak, airway is functioning Opening Airway To check breathing and give ventilations, you must manually tilt the head or thrust the jaw to move the tongue away from the back of the throat Head-tilt/chin lift: used when the rescuer is positioned at the victim’s side Jaw-thrust maneuver (with head extension): used when the rescuer is positioned above the victim’s head Jaw-thrust maneuver (without head extension) used when the victim is suspected of having an injury to the head, neck or spine Child, tilt the head slightly past the neutral position not as far as adult Infant, tilt head to neutral position Checking for Breathing Position your ear over the mouth and nose so that you can hear and feel air as it escapes while you look for the chest to rise and fall. Agonal gasps, isolated or infrequent gasping (this is NOT breathing) assume he/she is not breathing Checking for a pulse If you do not find a pulse with your fingertips in the arteries near the skin, within 10 seconds do not waste time. Adult and child: feel for carotid pulse “place two fingers in the middle of the victim’s throat and then slide them into the groove of the neck closest to you.” Infant: feel for brachial pulse on the inside of the upper arm between elbow and shoulder Give 2 ventilations Victims of cardiac arrest (witnessed sudden collapse), IMMEDIATELY begin CPR chest compressions. Other situations drowning or another respiratory event, giving ventilations before beginning CPR is important because victims of hypoxia (deprived of oxygen) likely to experience respiratory emergencies. Adults: unconscious and not breathing as a result of drowning, hypoxia or another respiratory problem, give the victim 2 ventilations before compressions. If unconscious and no pulse begin compressions Child or infant: unconscious and not breathing give 2 ventilations. Only skip if you witness a sudden collapse Scan for severe Bleeding Do a quick visual scan of the victim for severe bleeding. Head to toe scan Additional LGs should assist by controlling the bleeding Recovery Position Leave the victim in a face-up position and maintain an open airway if he/she unconscious but breathing (especially suspected spinal) High arm endangered spine (H.A.IN.E.S):keep the airway open and clear even if a spinal injury. You are alone and have to leave victim to call for help, you cannot maintain an open and clear airway because of the fluids or vomit. Perform secondary assessment Victim does NOT have any life-threatening conditions, to identify any additional problems Provide Care for the Conditions Found Always treat life-threatening situations FIRST. Care should be continued until EMS personnel take over Report, Advise, and Release Once care is given, be sure to complete incident report forms, advise the victim on next steps and release the victim to appropriate parties. One Age does NOT fit all Purpose of the skills in this manual Anyone approx. 12 years of age or older is an ADULT Anyone age 1 year to about 12 years is a child An infant is anyone younger than 1 year AED anyone 1 to 8 years of age less than 55 pounds is an child Call first or care first If alone: Call first for : (cardiac emergencies) Any adult or child about 12 years of age or older who is unconscious A child or an infant who you witnessed suddenly collapse An unconscious child or infant known to have heart problems. Care First (proved 2 minutes of care) for: (breathing emergencies) An unconscious child (younger than 12 years of age) who you did not see collapse Any victim of a nonfatal drowning Adult Child 1. Tap the victims shoulder and shout, “Are you okay.” Infant Tap on foot 2. If no, response (Unconscious) summons EMS 3. Check for signs of life (movement and NORMAL breathing) a. If victim face down, roll victim onto back, while supporting head. b. Tilt head back and lift the chin to open airway. Look for movement and look, listen and feel for normal breathing for NO more than 10 seconds. Head tilt not as dramatic Very little to no head tilt 4. If no movement or breathing, give two rescue breaths with resuscitation mask. Each breath should last about 1 second and make the chest clearly rise. 5. If chest clearly rises, check for pulse, CAROTID ARTERY, for no more than 10 seconds. a. One hand on the victim’s forehead, take other hand and place two fingers on the front of the neck. Then, slide the fingers down into the groove at the side of neck. 6. Quickly scan the victim for severe bleeding. 7. Care for conditions found. a. If there is movement, breathing, and pulse, place victim in H.A.IN.E.S. recovery position (if spinal is suspected) continue to monitor ABCs (airway, breathing, circulation) One hand on infant’s forehead, use other hand to find the brachial pulse on the inside of the upper arm, between the infant’s elbow and shoulder