Chapter One PowerPoint
advertisement

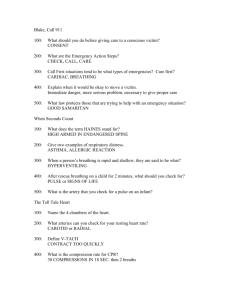
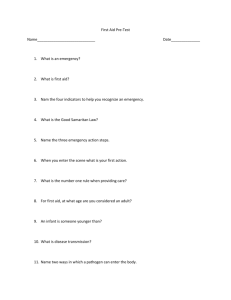
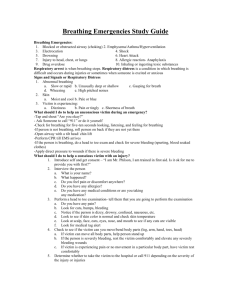
Chapter One Before Giving Care and Checking an Ill or Injured Person The EMS System Network of community resources and medical personnel that provides emergency care to victims of injury or sudden illness The Lay Responder Someone who recognizes an emergency and decides to help First aid – is immediate care given to a victim of injury or sudden illness until more advanced care can come In other words – this is you doing what you have learned The EMS Dispatcher The dispatcher is the person who receives the call from the citizen responder This person determines what help is needed Some are trained to give the caller instructions until EMS comes In other words, the person who answers when you call 9-1-1 First Responder This is the first person to arrive on the scene who is trained to provide a higher level of care They are often close to the scene and have the appropriate equipment and supplies to give care The Emergency Medical Technician The EMT is capable of providing more advanced care and life support techniques EMT Basic Level – all ambulance personnel have this basic training EMT Paramedics – at this level they can give medication, IV fluids, and provide advanced airway care. They are the highest level of care outside of the hospital Hospital & Rehabilitation Hospital – once the victim arrives at the hospital, the personnel there takes over Rehabilitation – the goal of rehab is to return the victim to his/her previous state of health Your Role in the EMS System Recognize that an emergency exists Decide to act Activate the EMS system Give care until help arrives Step 1: Recognizing an Emergency Unusual Noises Unusual Sights Unusual Odors Unusual Appearance and Behavior Step 2: Deciding to Act Barriers to Action Definition - Things that would stop you from helping a victim. 1. 2. 3. 4. 5. 6. 7. Panic of fear of doing something wrong Being unsure of the person’s condition and what to do Assuming someone else will take action The type of injury or illness Fear of catching a disease Fear of being sued Being unsure when to call 9-1-1 The Good Samaritan Law Usually protects citizens who act the same way that a “reasonable and prudent person” would if that person were in the same situation. Good Samaritan laws were developed to encourage people to help others in emergency situations. Examples of being “reasonable and prudent” include Moving a person only if the person’s life were in danger. Asking a conscious person for permission, also called consent, before giving care. Checking the person for life-threatening conditions before giving further care. Calling 9-1-1. Continuing to give care until a trained responder takes over. Disease Transmission Infectious diseases – spread from one person to another when germs enter the body and cause illness. Bacteria – can live outside the body and do not need other organisms for life. Treated with antibiotics. Viruses – depend on other organisms to live. They have few medications for treatment. Disease Transmission Direct contact – germs from another person’s body fluids pass directly into your body through breaks in the skin or mucus membranes. Indirect contact – germs pass through shared objects like spoons, doorknobs and pencils which have been exposed to infected droplets. Disease Transmission In order to get a disease the following conditions must be present – 1. 2. 3. 4. The victim must be infected with a disease The rescuer must be exposed to the infected victim’s body substance The rescuer must come in contact with the substance through an entry site There must be a sufficient amount of the infected body substance to cause infection Preventing Disease Transmission Standard Precautions - practices used to prevent spread of diseases 1. 2. 3. 4. 5. 6. 7. 8. 9. Avoid contact Use breathing barriers Use disposable gloves Cover any of your own open wounds before putting on personal protective equipment (PPE) Do not eat, drink or touch your face when giving care or before washing your hands after care has been given Avoid touching your personal items while giving care Do not touch objects that may have come in contact with body fluids Wash your hands thoroughly after care Tell EMS personnel or your doctor if you come in contact with a victim’s body fluids Cleaning Up Blood Spills Clean up the spill immediately or as soon as possible after it occurs. Use disposable gloves and other PPE when cleaning. Wipe up the spill with paper towels. After the area has been wiped up, flood the area with a disinfectant – 1 ½ cups bleach to 1 gallon of water. Dispose and label “biohazard” Step 3: Activate the EMS System Step 4: Give Care Until Help Arrives Consent – getting permission to give care You must tell the victim – Your name Your training What you think is wrong What you plan to do Expressed consent – when a conscious person who understands your questions and what you plan to do gives you permission to give care If the victim is an infant or a child, get permission from the parent or guardian Denied Consent Do not touch or give care to a conscious person who refuses care. If the person refuses care or withdraws consent at any time, step back and call 9-1-1. Implied Consent Definition – assumption that if the person could respond, he or she would agree to care. Consent is implied when – If an adult is unconscious If an adult is conscious but too seriously injured or ill to respond If an infant or child has a life threatening condition and the parent or guardian is not present Giving Care Until Help Arrives In general, you should give the appropriate care to an ill or injured person until: o o o o You see an obvious sign of life, such as breathing Another trained responder takes over You are too exhausted to continue The scene becomes unsafe Taking Action Emergency Action Steps Check the scene and the person Call 9-1-1 Care for the person Check Is the scene safe? Chemicals, traffic, fire, smoke, extreme weather Avoid confined areas with no ventilation If you can’t get near the victim, call 9-1-1 Check Is there immediate danger involved? Do not move seriously injured victims unless there is immediate danger or you have to move the person to give proper care such as CPR. Make sure bystanders do not move the victims. Check What happened? Look for clues to what caused the emergency. Nearby objects, broken glass, spilled bottle Check How many people were involved? Look carefully for more than one person. If one person is bleeding or screaming you may not notice an unconscious person. In an emergency with more than one victim you may have to prioritize care. Is anyone else available to help? Check What is wrong? Try to find out what is wrong. Look for signals of life threatening emergencies. Unconscious, no breathing, no pulse, severe bleeding Use all senses to try to notice if anything is abnormal Call Often times the most important thing you can do is call 9-1-1. When to call Unconscious or altered level of consciousness Breathing problems Persistent chest pain Persistent abdominal pain or pressure Severe external bleeding Severe burns Suspected poisoning Vomiting blood or passing blood Seizures Stroke Injuries to the head, neck, or back Suspected broken bone or an open fracture Also call for these situations Fire or explosion Downed electrical wires Swiftly moving or rapidly rising water Presence of poisonous gas Serious car accident Injured or ill person who cannot be moved easily Call First or Care First? You should always CALL FIRST for – An unconscious adult or adolescent (12 y/o) A witnessed sudden collapse of a child or infant An unconscious infant or child known to be at high risk for heart problems These are all possible cardiac emergencies therefore time is crucial Call First or Care First? You should CARE FIRST for – An unwitnessed collapse of an unconscious person younger than 12 years old Any victim of a drowning Conscious person who is choking These situations are more likely to be breathing emergencies Call Provide information requested by the dispatcher Location Description of person’s condition Do not hang up first Whenever possible have a bystander make the call for you Care 1. 2. 3. 4. 5. 6. Do no further harm Monitor the person’s breathing and consciousness Help the person rest in the most comfortable position Keep the person from getting chilled or overheated Reassure the person Give any specific care needed Give Care Until Help Arrives If you are trained in first aid, you can give help that can save a life in the first few minutes Get bystanders to help by – Calling 9-1-1 Clearing the scene Directing EMS personnel when they arrive Helping provide care Providing information about the victim Comforting and reassuring victims Should you just take them to the hospital yourself? Never transport a person – When the trip might cause greater damage to the person When the person may develop a life threatening condition If you are unsure of the injury or illness If you take the person to the hospital – Take someone with you and the victim Pay attention to any changes in the victim while en route Why would you move a victim? Only move the ill or injured person if – You are faced with immediate danger You have to get to another person who may have a more serious problem You have to move the person to give them proper care Emergency Moves Walking Assist Two Person Seat Carry Pack Strap Carry Blanket Drag Emergency Moves Clothes Drag Reaching Assist Foot Drag Throwing Assist Conscious Ill or Injured Person no immediate life threatening conditions Two Basic Steps – Step One Interview the victim and bystanders What happened? 2. Do you feel pain or discomfort anywhere? 3. Do you have any allergies? 4. Do you have any medical conditions or are you taking any medication? Write down the information and give it to EMS personnel when they arrive. 1. Conscious Ill or Injured Person no immediate life threatening conditions Two Basic Steps – Step Two Do a Head to Toe Check of the Victim 1. 2. 3. 4. 5. 6. Do not move areas of the body that hurt. Look for cuts, bruises, bumps, and depressions. Watch for changes in consciousness and breathing. Notice how the skin looks and feels. Look over the body. Look for a medical ID tag. Checking an Ill or Injured Infant or Child – What You May Do Differently Start your check at the victim’s feet instead of their head. Check the victim while he or she is seated in his or her parent’s or guardian’s lap. Shock A condition in which the circulatory system fails to circulate oxygen rich blood to all parts of the body. When vital organs do not get oxygen rich blood they do not work properly. Vital organs – brain, heart, lungs Shock Three conditions must be present for adequate blood flow – The heart must be working well. An adequate amount of oxygen-rich blood must be circulating in the body. Blood vessels must be intact and able to adjust blood flow. Signs & Symptoms of Shock 1. 2. 3. 4. 5. 6. Restlessness or irritability Altered level of consciousness Nausea or vomiting Pale, ashen or grayish, cool, moist skin Rapid breathing or pulse Excessive thirst Care for Shock 1. 2. 3. 4. 5. 6. 7. CALL 9-1-1 Have the person lie down Control any external bleeding Maintain normal body temperature Do not give the person anything to eat or drink Reassure the person Continue to monitor the person’s breathing Checking an Unconscious Person If you think someone is unconscious – Tap their shoulder and ask if they are ok Infant – tap shoulder or flick the bottom of their foot If they do not respond CALL 9-1-1 Check to see if the person – Has an open airway and is breathing Is bleeding severely Signs of Life Consciousness, normal breathing and circulation and skin characteristics are referred to as signs of life. Checking an Unconscious Person As easy to remember as ABC! Airway – open the airway Breathing – check for movement or breathing Circulation – check for severe bleeding Checking the Airway & Breathing Head Tilt/Chin Lift Technique used to open a victim’s airway Moves the tongue away from the back of the throat, allowing air to enter Checking the Airway & Breathing Look, listen, and feel for breathing for no more than 10 seconds. Agonal breath is irregular, gasping or shallow. Someone with agonal breathing should be treated like a non-breathing victim. If the victim is not breathing Adult – begin CPR immediately Child or Infant – give 2 rescue breaths Child – pinch nose, complete seal over mouth and give 2 rescue breaths each lasting 1 second Infant – complete seal over mouth and nose and give 2 rescue breaths each lasting 1 second Special Situations Air in the Stomach Avoid forcing air into the person’s stomach by keeping the person’s head tilted back. Air in the stomach can cause the victim to vomit. Choking Harder to breathe Special Situations Vomiting H.A.IN.E.S. Clear it out Continue care Special Situations Mouth to Nose Breathing Close the mouth by pushing on the chin If possible, open the victim’s mouth between rescue breaths to let the air out Special Situations Mouth to Stoma Breathing Expose the person’s neck down to the breastbone Keep the airway in neutral position If the tube is blocked, remove the inner tube If partial breather, rescuer must seal the mouth and nose Special Situations Head, Neck, and Spinal Injuries If a child is in a car seat, do not remove the child from the seat Minimize movement when opening the airway Tilt the head and left the chin just enough to open the airway Special Situations Drowning Victim For an adult, give 2 rescue breaths as you would for a child or infant once you determine the victim is not breathing Give 2 minutes of care before calling 9-1-1 for an unconscious person who has been submerged Do not go in the water to rescue someone unless you are trained to do so What to do next Vomit, fluids blocking the airway, or if you must leave the victim, place the person in the H.A.IN.E.S. recovery position. Incident Stress Definition - a condition caused by acute stress which overwhelms a person to the point that they are unable to cope with the stress. If not appropriately managed, this stress can lead to PTSD. Signals of Incident Stress 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Anxiousness and unable to sleep Nightmares Restlessness Confusion Low attention span, poor concentration Denial, guilt, anger, depression Nausea Increased or decreased eating Change in interactions with others Uncharacteristic, excessive humor or silence Unusual behavior Difficulty performing day to day tasks (job, school) Guidelines for Coping with Incident Stress 1. 2. 3. 4. 5. 6. Seek help Use relaxation techniques Eat a balanced diet Avoid alcohol and drugs Get enough sleep Participate in some type of physical activity