adenoidectomy-20and-20tonsillectomy-140323074835
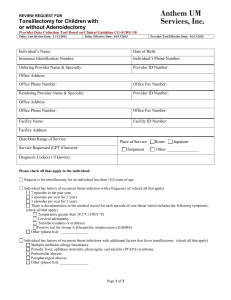
advertisement

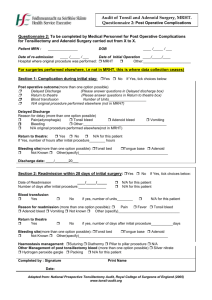
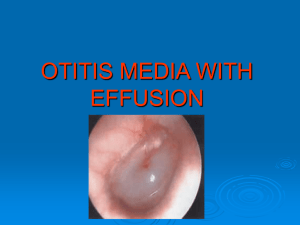
ADENOIDECTOMY AND TONSILLECTOMY Dr Joel G Mathew ADENOIDECTOMY ADENOIDECTOMY - INDICATIONS • Adenoid hypertrophy causing: • Otitis media with effusion (SOM) • Upper airway obstruction and obstructive sleep apnoea • Recurrent acute otitis media • Recurrent rhinosinusitis (Abolishing infective episodes) ADENOIDECTOMY - CONTRAINDICATIONS • Acute upper respiratory infections • Acute epidemic of Poliomyelitis>Paralytic polio (Exposed nerves) • Bleeding disorders and Anaemia • Cleft Palate • Overt cleft palate SUBMUCOUS CLEFT PALATE (COVERT) • Abnormal nasal speech, • Bifid uvula • Thin strip of mucosa in the middle of roof of mouth • Notch at the back of hard palate. ADENOIDECTOMY - PROCEDURE • Anaesthesia – General Anaesthesia • If combined, Adenoidectomy before Tonsillectomy POSITION – ROSE’S POSITION Supine with head extended by placing a pillow or sandbag beneath the shoulders. Advantage – Larynx lies at a higher level than oral cavity – no risk of aspiration. Excellent exposure Both hands of surgeon are free. Hyperextension is avoided Makes cervical vertebral bodies prominent-Damage to ligaments or cartilages of vertebral spine or bodies -> Grisel’s syndrome GRISEL’S SYNDROME • Non traumatic subluxation of atlanto axial joint • Results from any condition that results in hyperaemia and pathological relaxation of the transverse ligament of the atlanto-axial joint. • Due to infection in the periodontoid vascular plexus that drains the region->paraspinal ligament laxity. • Presents with persistent neck pain and torticollis 1-2 weeks following surgery. • More common in Down’s syndrome patients • X-ray and CT of Cervical spine confirms diagnosis. • Treatment: Cervical immobilisation , analgesics and antibiotics. Arthrodesis in intractable cases TECHNIQUE OF ADENOIDECTOMY • The surgeon stands behind the patient. • Boyle-Davis mouth gag is inserted, opened and held in place by Draffin’s bipod stand • Palate is palpated to exclude a submucous cleft palate. • The soft palate is retracted by a suction catheter introduced through the nose, and pulled out of the oral cavity. • The adenoid is palpated with a finger. • St Clair Thomson adenoid curette with guard is introduced into the nasopharynx above the upper end of adenoid tissue, “held like a dagger” • With a downward and forward sweeping movement, adenoids are shaved off. • A smaller sized curette is used to curette the adenoids around the choana and the Eustachian cushions • Nasopharynx is packed with gauze packs for a few minutes for haemostasis. OTHER TECHNIQUES OF ADENOIDECTOMY • Suction coagulator/diathermy • Endoscopic transnasal or transpalatal adenoidectomy with microdebrider • Coblator plasma field device POSTOPERATIVE CARE • The patient is kept in lateral position • Kept nil orally until fully recovered from GA (4-6 hours). • Monitor vitals • Watch for bleeding: Earliest sign-”Frequent swallowing” • Oral antibiotics and analgesics COMPLICATIONS • Haemorrhage ( < 0.7%) – Managed by postnasal packing. • Surgical trauma: • Teeth • Soft palate • Uvula • Eustachian cushions-stenosis, secretory otitis media • Cervical spine-atlantoaxial dislocation • Velopharyngeal insufficiency • Hypernasal speech, swallowing difficulty and rarely nasal regurgitation • Adenoid remnant (Upto 29%) • Pulmonary complications-Aspiration, “Coroner’s clot” • Infection of Nasopharynx. TONSILLECTOMY TONSILLECTOMY-INDICATIONS Absolute Indications: Obstructive symptoms and Obstructive sleep apnoea Malignancy or suspected malignancy Recurrent peritonsillar abscess Tonsillitis causing febrile seizures in children Relative Indications: Recurrent tonsillitis: >= 7 episodes in 1 year >=4 episodes per year for 2 consecutive years >= 3 episodes per year for 3 consecutive years Halitosis due to chronic tonsillitis Tonsilloliths Tonsillar cysts Dental and orofacial abnormalities Dipheria carriers Rheumatic fever and Acute glomerulonephritis TONSILLECTOMY AS PART OF ANOTHER PROCEDURE • Excision of elongated styloid process (Eagle syndrome) – Nagging throat pain and a palpatory finding in the tonsillar fossa. Confirmed by palpation and injection of anaesthetic. • Glossopharyngeal neuralgia • UPPP (Uvulopalatopharyngoplasty)or LAUP (Laser-assisted uvulopalatoplasty) or CAUP (Coblation assisted uvulopalatoplasty) CONTRAINDICATIONS • Bleeding disorders • Cleft palate or submucous cleft palate • Velopharyngeal insufficiency • Acute infection • Uncontrolled systemic disease • Anaemia • Extremes of age PROCEDURE • Anaesthesia: General anaesthesia • Position-Rose’s position-supine with head extended by placing a pillow or sandbag under the shoulder • Operative techniques • DISSECTION AND SNARING -> Classical • Diathermy • Coblation tonsillectomy • Ultrasonic dissection • Laser tonsillectomy • Capsulotomy techniques • Guillotine method (Ancient) DISSECTION AND SNARE METHOD • Boyle Davis mouth gag is inserted, opened and held in position with Draffin’s bipod stand • Upper pole of tonsil is held with tonsil holding forceps and pulled medially • Mucosa is incised with blunt scissors, knife, forceps or diathermy at the point where it reflects from tonsil to anterior pillar. Incision is continued inferiorly towards base of tongue. • The tonsil is separated from its bed by blunt dissection, upto the lower pole • The plane of dissection is the loose areolar tissue separating tonsil from its bed. • Once lower pole is reached, a tonsillar snare is passed over the tonsil holding forceps, placed over the tonsil, threaded down to the lower pole, tightened to crush the pedicle, and the tonsil is removed • Gauze packs are kept in the tonsillar fossa • Bleeding points are looked for, and bleeding arrested with non absorbable sutures POSTOPERATIVE CARE • Patient is nursed in the lateral position • Kept nil orally until fully recovered from GA (4-6 hours). • Monitor vitals • Watch for bleeding: Earliest sign-”Frequent swallowing” • Ice cold fluids and ice cream given on the first day • Oral antibiotics and analgesics COMPLICATIONS OF TONSILLECTOMY • HEMORRHAGE • Primary • During the surgery • Controlled by pressure packing, ligation, cauterisation • Reactionary • Within 24 hours of surgery • CAUSES OF REACTIONARY HEMORRHAGE (VIVA): 1. 2. 3. 4. 5. Formation of a blood clot or Dislodgement of blood clot from lumen Vasodilation of blood vessel Postoperative rise in blood pressure Increased venous pressure by coughing or retching Slipping of ligature • Management of Reactionary haemorrhage: • Blood is cross matched • Tonsillar fossa is inspected and clot removed • Pressure with a swab soaked in 1:1000 Adrenaline • Administration of hemostatic agents (Ethamsylate, Tranexamic acid) • May require taking to the operation theatre and ligation under General Anaesthesia. • Most dangerous form of haemorrhage because: • It may be missed (Patient may still be under the effect of GA) • It may cause fatal aspiration • Large hemorrhages may require ligation or electrocoagulation under GA. Two GAs at a short interval is dangerous. • Secondary haemorrhage (>24 hours – 2 weeks) • Cause: Infection of the granulating tonsillar bed • Treated with Antibiotics • OTHER COMPLICATIONS OF TONSILLECTOMY: • Injury to: • Temporo-mandibular joint • Lips and commisures of mouth • Tongue, uvula, soft palate • Very rarely Glossopharyngeal nerve, pharyngeal venous plexus, carotid sheath • Grisel syndrome (Non traumatic atlanto axial dislocation) • Aspiration of blood-> Pneumonia, collapse of lung, or lung abscess • Hematoma and oedema of uvula • Referred earache • Velopharyngeal insufficiency • Tonsillar remnants