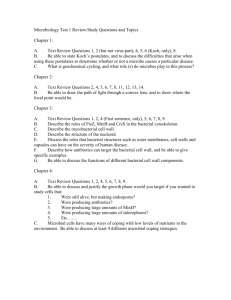
Intro To Antimicrobials
advertisement

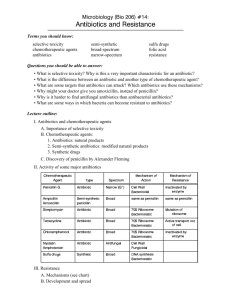
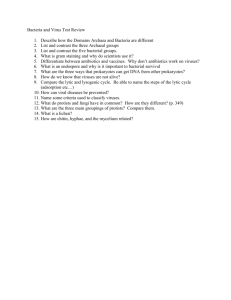
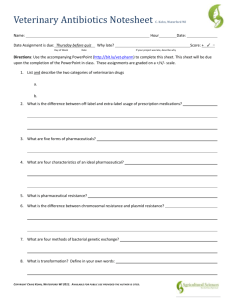
INTRODUCTION TO ANTIMICROBIAL CHEMOTHERAPEUTICS September 2013 Selective Toxicity The selective toxicity of antibiotics means that they must be highly effective against the pathogen microorganisms but have minimal or no toxicity to humans. In practice, this is expressed by a drug's therapeutic index (TI) - the ratio of the toxic dose (to the patient) to the therapeutic dose (to eliminate the infection). The larger the index, the safer is the drug (antibiotic) for human use. Selective Toxicity The selective toxicity of antibiotics is brought about by finding vulnerable targets for the drug in the target microorganism that do not exist in the animal (eucaryote) that is given the drug. Most antibiotics in clinical usage are directed against; bacterial cell wall synthesis, bacterial protein synthesis, or bacterial nucleic acid synthesis, which are unique in some ways to bacteria. Selective Toxicity For example, the beta lactam antibiotics (penicillin and its relatives) inhibit peptidoglycan synthesis in the cell wall. Humans have neither a cell wall nor peptidoglycan and so are unaffected by the action of the drug. Other antibiotics, including streptomycin and the tetracyclines, target bacterial protein synthesis because bacterial ribosomes (termed 70S ribosomes) are different from the ribosomes (80S) of humans and other eucaryotic organisms. Selective Toxicity Antibiotics such as the flouroqinolones (e.g. ciprofloxacin) inhibit procaryotic (not eucaryotic) DNA replication, and rifamycins inhibit bacterial (not eucaryotic) DNA transcription. From a patient point of view, the most important property of an antimicrobial agent is its selective toxicity, i.e., that the agent acts in some way that inhibits or kills bacterial pathogens but has little or no toxic effect on the patient. Antibiotics may have a cidal (killing) effect or a static (inhibitory) effect on a range of microbes. The range of bacteria or other microorganisms that is affected by a certain antibiotic is expressed as its spectrum of action. Antibiotics effective against procaryotes that kill or inhibit a wide range of Gram-positive and Gram-negative bacteria are said to be broad spectrum. If effective mainly against Gram-positive or Gramnegative bacteria, they are narrow spectrum. If effective against a single organism or disease, they are referred to as limited spectrum. • Effect of different dose schedules on shape of concentration-time curve. • The total AUC for the fractionated dose in curve B is determined by adding AUC0-8h, AUC8-16h and AUC1624h, which adds up to the same AUC0-24h in curve A. • The time that the drug concentration exceeds MIC in curve B is also determined by adding up T1>MIC, T2>MIC, and T3>MIC, which results in a fraction greater than that for curve A.