Nursing Care Plan: Elderly Patient with Mobility Issues & UTI
advertisement

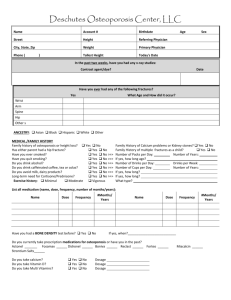
NSG3MCC Assessment Task 3 Nursing Care Plan Template Members in Group: Nicole Stafford 16445856, Baljit Pannu, Bonnie-Kate Wood 16133476, Denis Baniqued, Leah Dridan 16080544, Melissa Salemme 15802975 Clients Gender: Female Clients Age: 87 Medical Diagnosis: decreased mobility, UTI Past Medical History:osteoartritis(severe), osteoporosis, proxysmol AF, vestibular dysfunction, PUD Current Medications: Clexane 20mg S/C daily 0800 Aspirin 100mg daily 0800 Alendronate 70mg weekly 0700 Sotalol 80mg BD 0800 & 2000 Sertraline 50mg daily 0800 Coloxyl & Senna 2 tablets BD 0800 & 2000 Paracetamol 1g QID 0800/1200/1800/2200 Assessment Planning /Implementation Evaluation Nursing Diagnosis Expected Outcome –patient goal Nursing Interventions Rationale Outcome Assessment Chronic pain related to physical disability, secondary to osteoporosis. Patient will report decreased levels of pain and increased tolerance in performing activities within one week. Assess patient’s physical symptoms of pain using a pain assessment tool. To assess the patient for pain and to provide successful pain management (Bruckenthal, 2008). The patient verbalises reduced pain assessment ratings. Prior to the patient performing an activity, carry Pain limits mobility and is often exacerbated by Patient verbalises reduced pain on mobilisation. The patient may be experiencing some weakness due to a decrease in bone density secondary to osteoporosis. The expected outcome will be that the patient will be more educated on how to manage osteoporosis as well as show an improvement in their bone density and out a pain assessment and treat the pain accordingly. movement (Ackley & Ladwig, 2008) Assess the patient’s cognitive functioning using a Mini Mental State Examination. To use appropriate pain assessment tool and to assess the extent of which the patient will be able to comply with the pain treatment regime (Scherder, Herr, Pickering, Gibson, Benedetti, & Lautenbacher, 2009). Patient suffers from depression and occasionally has short term memory issues, medications are prepared for her in a Webster pack to improve medication compliance. Educate patient on importance of taking medications and the relationship of the medications with her disease process. To empower patients and improve their knowledge with regard to their medications, which optimises the likelihood of patients to take their medications (Nurit, Bar Cohen, & Zelker Revital, 2009). Verbalises importance of medication and repeats back understand of education session. Assess the patient’s bone density by ordering a bone density scan in order to accurately assess the deterioration of the bones. Bone density scans are usually used to analyse the extent of the density of the bones in order to be able to plan out treatment (Blake & Continuous bone density scans in order to determine an improvement in bone density and strength. strength before being discharged from the hospital. Fogelman, 2007). These scans are also used to measure any improvement in bone density once interventions have been put in place (Blake & Fogelman, 2007). Refer the patient to a dietician who will organise an appropriate diet for an individual with osteoporosis. A diet high in calcium will help to prevent osteoporosis as well as slow down the progression of the disease in effected individuals and therefore increase their strength (Stransky & Rysava, 2009). Monitor the patient’s diet and make sure that they are well educated on the foods that are beneficial to bone strength. Administer calcium and vitamin D supplements. Administering calcium Make sure that the patient is and vitamin D taking their supplements. supplements in the treatment of osteoporosis will help to absorb the calcium in their diet as well as prevent the occurrence of an osteoporotic fracture (Stransky & Rysava, 2009). Refer the patient to a physiotherapist in order to do simple strengthening exercises. Simple exercises such as walking or simple stretches can help to strengthen bones as well as prevent or slow down progression of osteoporosis (Keramat et. al, 2008). Allow the patient to demonstrate various simple exercises to promote bone strength. Educate the patient on osteoporosis by providing them with various brochures and information sessions in the community. Education is important for the patient to self care for their osteoporosis in the community setting (Nielsen et. al, 2010). It may be beneficial for the patient to join a community group who educate on osteoporosis, as it has been proven to be more successful in slowing down the progression of the condition through consolidating their education into practice and therefore producing stronger bones (Nielsen et. al, 2010). Group sessions also increase the likelihood that the patient will adhere to their Let the patient tell you about osteoporosis and the treatments to prevent further progression and improve bone density. treatment plan (Nielsen et. al, 2010). Baljit diagnosis ??? Denis Diagnosis ??? Self-care deficit and inability to perform activities of daily living related to disease progression, weakness and joint deformity. Achieve independence of self-care and maintain optimal role function. Monitor patient’s ability to perform independent selfcare. Knowing what the patient is capable of enables us to plan appropriate interventions (Brown & Edwards, 2008). Monitor patient’s needs for adaptive advices for personal hygiene, dressing, grooming, toileting and eating. Advices can compensate for contractures and weakness, so that the patient can perform as many self-care activities as possible, promoting independence (Ward & Loring, 2005). Establish a routine for selfcare activities with rest periods. Establishing a routine fosters maximum independence for the patient and rest periods allow minimal fatigue (Brown & Edwards, 2008). Modifications to home such as removing rugs, providing rails and elevated toilet seat. Modifications may be necessary to allow the patient to be as independent as possible without the risk of possible injury (DVA, 2011) Teach family to encourage independence and to intervene only when the patient is unable to perform the task Teaching the family to only intervene when absolutely necessary is to allow the patient to understand they can do it and gives them independence in activites (Ward & Loring, 2005). Potential constipation during hospital stay due to decreased mobility and analgesic medications. Patient will maintain regular to substantial bowel motions during her hospital stay. Observe and monitor usual defecation patterns, including amount, frequency and stool consistency. Compare this to regular bowel motions of patient prior to hospital stay and during hospital stay. This allows a baseline that enables nursing and medical staff to compare if patient becomes distended and impacted (Gulanick & Myers, 2007). Monitor the chart to recognise any changes in bowel actions. Encourage mobility and ADL’s. Ensure these are undertaken post pain medication administration for patient comfort. Mobilising and being active increases peristalsis of the bowels enabling bowel motions and decreasing the chances of constipation (Gulanick & Myers, 2007). The patient is more likely to be apprehensive of mobilising when there is strong pain involved on movement. Despite pain medications contributing to decreased elimination, the patient is best to mobilise out of bed when medications are administered, than nil movement after (Gulanick & Myers, 2007). Reassess mobility levels daily and determine which method of mobilising is most comfortable for the patient.(Gulanick & Myers, 2007). If patient is in too much pain for weight bearing, encourage movements on the bed, including twisting and changing positions while in bed, lifting her left leg up and down slowly, pulling her left knee to her hip and slowly straightening her leg. Other exercises can include lifting her upper torso slightly whilst flexing her abdominal muscles. Encourage fluid intake, 6-8 glasses per day Adequate fluid intake is Use a fluid balance chart to necessary to prevent hard monitor fluid intake and and dry stools that are difficult to pass (Eoff & Lembo, 2008). output. Encourage oral intake, a diet high in fibre. When fibre reaches the colon, it absorbs water formin a gel and adding bulk to faeces, enabling full stools that are easy to pass (Eoff & Lembo, 2008). Use a food chart to monitor nutritional intake. Educate the patient on how and why the constipations have occurred, as well as interventions they can initiate to prevent it Education will allow the patient to understand constipation better, hence enabling them to self initiate and manage their own care (Eoff & Lembo, 2008). Assess the patients understanding of constipation and have them talk the steps into preventing constipation. Provide laxatives, suppositories, and enemas ordered or when required. These soften stool, lubricate intestinal mucosa and help peristalsis (Gulanick & Myers, 2007). Assess patients bowel chart and ask patient about their bowel motions, any discomfort or pain that is present. From this information, determine if medication will be needed. (Eoff & Lembo, 2008). Bibliography Ackley, B. J., & Ladwig, G. B. (2008). Nursing diagnosis handbook: an evidenced-based guide to planning care. St Louis: Mosby Elsevier. Blake, G.M., Fodelman, I. (2007). The role of DXA bone density scans in the diagnosis and treatment of osteoporosis. Postgraduate Medical Journal. 83(982), 509-517 Brown, D. (2008). Lewis’ Medical-Surgical Nursing: Problems related to movement and co-ordination (2nd ed) Chapter 28, 1812-1814. Elsevier Australia. Bruckenthal, P. (2008). Assessment of Pain in the Elderly Adult. Clinics in Geriatric Medicine, 24(2), 213-236. Department Of Veteran Affairs (DVA), 2011. Homecare and Support: Community Aged Care. Retrieved September 15th 2011 from www.dva.gov.au Eoff J.C., & Lembo, A.J. (2008). Optimal treatment of chronic constipation in managed care: Review and roundtable discussion. Journal of managed care pharmacy 14 (9), S5-S9. Gulanick, M., & Myers, J. (2007). Nursing care plans: Nursing diagnosis and intervention. (6th ed.). St. Louis, Missouri: Mosby Elsevier. Keramat, A., Patwardhan, B., Larijani, B., Chopra, A., Mithal, A., Chakravarty, D. (2008). The assessment of osteoporosis risk factors in Iranian women compared with Indian women. BMC Musculoskeletal Disorders. 9(28) Nielsen, D., Ryg, J., Nielsen, W., Knold, B., Nissen, N., Brixen, K. (2010). Patient education in groups increases knowledge of osteoporosis and adherence to treatment: A two-year randomized controlled trial. Patient Education and Counselling. 81(2), 155-160 Scherder, E., Herr, K., Pickering, G., Gibson, S., Benedetti, F., & Lautenbacher, S. (2009). Pain in dementia. Pain, 145(3), 276-278. Stansky, M., Rysava, L. (2009). Nutrition as Prevention and Treatment of Osteoporosis. Physiological Research. 58(1), s7-s11 Ward. M, Loring. K (2005). Patient Education Interventions in osteoarthritis and rheumatoid arthritis: a meta-analytic comparison with Non-Steroidal AntiInflammatory Treatment. 9 (4), 292-301