SCHIZOPRENIA
advertisement
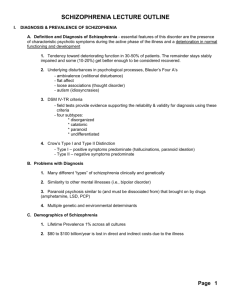
SCHIZOPHRENIA What is Schizophrenia? Schizophrenia is a medical illness that causes strange thinking, abnormal feelings, and unusual behavior. It is uncommon in children and hard to recognize in its early stages. Adult behavior often differs from that of teens and children. Symptoms of Diagnosis In children, Schizophrenia is preceded by developmental disturbances. (speech problems, lacking needed motor skills…) Diagnostic criteria is the same for both children and adults, only symptoms must appear prior to 12 years of age. May see or hear things that do not exist May be paranoid or have bizarre beliefs Other Symptoms Problems paying attention Impaired memory Inappropriate expressions (laughing something is not funny such as some one being hurt) Poor social skills Depressed mood Diagnosis Problems Often misdiagnosed in children Mistaken for autism, personality disorders, bipolar disorder and dissociative disorders Abused children may hear voice of abuser or see visions of abuser Bottom Line: Schizophrenia is hard to diagnose in children! Early Warning Signs Trouble discerning dreams from reality Seeing things and hearing voices that are not real Extreme moodiness Concept that people are “out to get them” Confusing television with reality Severe problems making friends DSM IV Characteristic Symptoms: Two or more of the following present for a significant portion of time during a 1 month period (less if successfully treated): Delusions Hallucinations Disorganized speech Grossly disorganized or catatonic behavior Negative symptoms (affective flattening) Social/Occupational dysfunction Duration: Continuous signs of disturbance persist for at least 6 months. This 6 month period must include 1 month of symptoms. Type: Paranoid type Disorganized type Catatonic type Undifferentiated type Residual type Epidemiology Less than 1% for children under 19 years of age Never diagnosed under the age of 5 and rarely before age 15 Boys are at 2:1 advantage of an early onset compared to girls Boys first psychotic break between 15-24 Girls first psychotic break between 20-29 Levels out for older adolescents and adults Children: No SES ties or racial/ethnic ties Adults: Over diagnosed in African Americans World wide Schizophrenia is very evenly spread Comorbidity Substance abuse disorder Common substances are alcohol, stimulants such as cannabis, cocaine and amphetamines 33.7% of people with Schizophrenia disorder or schizophreniform met criteria for alcohol abuse 47% met criteria for any substance abuse 43% in 125 male patients consumed cannabis 20% for cocaine, 3% heroin, and nicotine between 70-90% 80% out of 62 adolescents with schizophrenia had comorbidity with substance use in New Zealand 69% of children with Schizophrenia met criteria for another psychiatric disorder Comorbidity Obsessive-Compulsive disorder Depression 7.8% with schizophrenia had OCD 26% out of 50 patients met criteria for OCD 25% prevalence rate with Schizophrenia Suicide 10% of patients commit suicide Suicide attempts are 5 times higher than suicide rate Comorbidity Other comorbid disorders Social phobia Generalized anxiety Avoidant personality disorder Eating disorder Conduct disorder Etiology Strong evidence of genetic component to development of Schizophrenia. The stronger the genetic compatibility between individuals, the higher the concordance rates. Cont… Concordance Rates Non twin siblings: 9% One biological parent 13% Dizygotic twins 17% Both parents 46% Monozygotic twins 48% (Also children of Schizophrenic mothers are at greater risk regardless of who raises them) Etiology cont… Evidence of prenatal and biological factors that lead to Schizophrenia. Disruptions in brain development during prenatal period Complications during pregnancy Studies suggest that brain abnormalities are evident in children/adolescents with Schizophrenia Decrease in grey matter in frontal and temporal regions Developmental Pathways Delayed developmental milestones such as walking or talking Poor academic work High levels of impulsivity High levels of social withdrawl When Schizophrenia appears in childhood it is often a life long disorder. Developmental Pathways First psychotic break in childhood often is followed by multiple other breaks throughout life. After the disorder develops, more noticeable complications arise: Social isolation Economic impairment Academic deficits Developmental Pathways Long term prognosis is generally related to age of onset. (Earlier onset=poorer prognosis) Childhood onset usually continues throughout adulthood. Full recovery is rare. Best hope is remission from active symptoms through intensive therapeutic interventions and psychopharmacology. Treatment Medication: “atypical” antipsychotics Olanzapine Clozapine Used to reduce symptoms such hallucinations and delusions New medicines help reduce chance of tardive dyskinesia Treatment Side effects of medication: Weight gain Blood disorder (agranulocytosis) Nausea Urinary retention Impotence Hyper salivation Dyskinesia Depression Treatment Typically a combination of medication (clozapine) and individual therapy, family therapy along with specialized programs is necessary. Medications can have many side effects. www.nimh.com Case Study Reported is a case of an early onset of Schizophrenia with a translocation between chromosomes 1 and 7. An 11 year old male was admitted to NIMH with symptoms including: disorganized speech, rambling, a 2 year history of agitation, beliefs that ghosts were talking to him and could control his mind and that “rough hands” were pursuing him at night. His parents’ first concern came during day care at age 4 when it was reported to them their son was socially isolated and continually holding his genitals. At age 5 he began special programs for education. At age 9 an evaluation at a university hospital shows low intelligence and a language disorder. The patient has hypotonia with gross and fine motor delays. He continued to have abnormal thoughts and an inability to focus. His symptoms from ages 9-11 showed symptoms of paranoid delusions, grandiosity, mind control, auditory hallucinations, visual hallucinations, and tactile hallucinations. As for the patient’s developmental history, the mother had pregnancy complications with insulin-dependant diabetes preceded by two trimesters of hypoglycemia that resulted in loss of consciousness and 6 hospitalizations. She also had a greater that 50 pound weight gain. The patient walked by 14 months but did not have normal babbling and did not speak until age 3. He had a good temperament that did not include separation anxiety and no temper tantrums. At age 11 the NIH completed a physical that concluded the boy’s body was at a disproportion, having abnormally long limbs compared to his torso, a triangular face and small mouth. The patient displayed inappropriate laughing and an inability to make eye contact. The patient met all criteria for the DSM-III-R for schizophrenia and was admitted to the NIMH at age 11 ½ years. Patient responded well to clozapine. To further iterate, the patient had 3 other relatives whose DNA contained the 1 and 7 chromosome translocation, none of which were diagnosed with schizophrenia. They did have symptoms of drug/alcohol abuse and language delay. Another study showed an autistic boy with 7 and 21 translocation of chromosomes that also had a 1 chromosome in the same location of the patient discussed. The patient did show some early signs of autism but not enough to be diagnosed. The relationship between autism and early childhood schizophrenia is still not clear, but studies have shown that 40% prepubertal schizophrenics did have autistic symptoms. At the time of this study it is hard to state the role of genetics in this patient’s schizophrenia. Certainly more research needs to be conducted, but this is very good start.