Sleep Apnea - BREATHE Heart Failure Nurses Association
advertisement

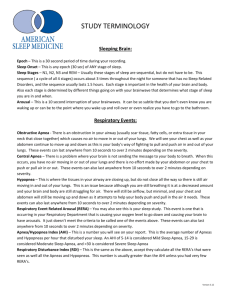
Sleep apnea in heart failure S. Javaheri , M.D Professor Emeritus of Medicine University of Cincinnati, College of Medicine Medical Director Sleepcare Diagnostics Cincinnati, Ohio Breathe Conference, Kings Island October 21st, 2011 javaheri@snorenomore.com Prevalence of Heart Failure in U.S. • 2% of population (6 million) • 6–10% of population >65 y old • Leading cause of hospitalization in people > 65 y The crystal ball Poor survival in heart failure in the era of beta blockers “Despite our many successes in the treatment of heart failure, our current drug regimens probably prolong survival only about 9 to 18 months relative to where we were in 1985” GS Francis, JACC, 2006 Current estimates of 5 y survival: 30 to 35% Sleep apnea and heart failure Identification and effective treatment of comorbidities which contribute to the progression of heart failure is of utmost importance. Sleep Medicine Physician Board Review OSA in heart failure occurs in subjects with compromised airway Sleep Medicine Physician Board Review SLEEP APNEA INCREASES LV TRANSMURAL PRESSURE Normal Hypertension 100 Ppl Ppl Ppl 140 0.0 LVTm 100 140 100 Pr UAO 0.0 100 - (0.0) = 100 100 -40 140 - (0.0) = 140 Sleep Medicine Physician Board Review 100 - (- 40) = 140 Prevalence of sleep apnea in Systolic Heart Failure 100 out of 114 consecutive patients 68% with AHI ≥ 5/h 49% with AHI ≥ 15/h Javaheri et al: Ann Intern Med 1995 Circulation 1998 Int J Cardiol 2006 Prevalence of sleep apnea in recent prospective studies of SHF Country (year) n % AHI≥15/hr % CSA % OSA * USA (06) 100 49 37 12 USA (08) 108 61 31 30 *Canada (07) 287 47 21 26 *UK (07) 55 53 38 15 Germany (07) 700 52 33 19 *Germany (09) 50 64 44 20 *Germany (10) 273 64 50 14 *Portugal (10) 103 46 n/a n/a China (07) 126 71 46 25 Germany (07) 203 71 28 43 Germany (07) 102 54 37 17 France (09) 316 81 25 56 % AHI≥10/hr Prevalence of sleep apnea in recent prospective studies of SHF 54% (897/1676) 34% (541/1573) 20% (308/1573) Prevalence of sleep apnea in Heart Failure with PEF • n = 244 consecutive patients (87 women) • Mean age 65 • Echocardiogram, Polygraphy, and R and L heart catheterization • Cause of DHF: - HTN (44%) - CAD (33%) - Hypertrophic/Restrictive (23%) Bitter T, 2009 EJHF Prevalence of Sleep Apnea in Heart Failure with PEF How frequently patients with HF are tested for SA? A retrospective cohort study used the 2004-2005 Medicare Standard Analytical Files (SAFs). SAFs contain a 5 % sample of randomly selected Medicare beneficiaries. The study population included newly diagnosed HF patients in the first quarter of 2004 without prior diagnosis of SA. Sleep Medicine Physician Board Review Under-diagnosis of sleep apnea in patients with heart failure Study Cohort N=30,719 SA tested N=572 (2%) SA Dx: N=553 (97%) tested, diagnosed, not treated N=295 Not SA tested N=30,147 (98%) No SA Dx N=19 (3%) tested, diagnosed, treated N=258 Javaheri et al. Am J Respir Crit Care Med 2011 Sleep Medicine Physician Board Review The mystery of the lack of subjective EDS in patients with SHF Most studies show no difference in subjective EDS in patients with systolic heart failure with or without sleep apnea. However, when tested objectively, by MSLT or Osler test, heart failure patients with sleep apnea are sleeper than those without sleep apnea. No difference in subjective EDS among the 3 groups(n=100) 90 No SA CSA OSA 80 70 60 50 p=0.8 40 30 Javaheri et al: 1998, 2006 20 10 0 Patients (n) EDS (%) *vs. Group I Group II †vs. Clinical impact of lack of subjective EDS in SHF 1.Under diagnosis of sleep apnea in systolic heart failure 2. Inadequate long-term CPAP adherence could diminish its effectiveness in maximizing LVEF and survival both for OSA and CSA Sleep Medicine Physician Board Review Sleep Apnea in Heart Failure: Then what should the primary care physicians and the cardiologists look for to suspect presence of sleep apnea in their patients with systolic heart failure? The phenotype depends differs in OSA and CSA Hallmarks of OSA in SHF 90 Group I *† 80 Group II p=0.02 p=0.1 70 Group III p=0.1 60 50 p=0.1 p<0.001 40 *† p=0.8 30 20 10 0 Patients (n) Age (y) Ht (in) BMI (kg/m2) Snoring (%) *vs. Group I Group II †vs. Sleep Medicine Physician Board Review EDS (%) Apnea (%) Hallmarks of CSA in SHF Sleep Medicine Physician Board Review Treatment of OSA in CHF • • • • • • • • Promote sleep hygiene Avoid ETOH, benzodiazepines, opioids, and Viagra Weight loss Positive airway pressure devices: CPAP, bilevel, Provent Mandibular advancement devices Upper airway procedures Hypoglossal N stimulation Nocturnal use of supplemental oxygen Sleep Medicine Physician Board Review Provent Effects of PAP therapy on LVEF in RCT OSA/SHF Kaneko Open Mansfield Open Egea DB Smith DB Khayat Open Khayat Open n 12 19 20 23 11 13 AHI, n/h 40 25 44 36 30 34 LVEF, % 25 35 29 30 29 26 Change in LVEF, % 9* 5* 2.2* 0.0 0.5 8.5* Duration 4w 3m 3m 6w 3m 3m PAP titration CPAP yes CPAP yes CPAP yes Auto no CPAP yes Bilevel yes 6.2 5.6 NR 3.5 3.6 4.5 Compliance OSA as Cause of Mortality in SHF • 218 patients with LVEF<45% • 45 with CSA (21%) • 113 control group, AHI < 15, mean = 7/h • 41 untreated OSA, AHI ≥15/hr, mean = 33/h Wang et al; JAAC, 2007 Wang H et al. J Am Coll Cardiol. 2007; 49: 1632 Worsening Survival of Patients With Heart Failure and OSA AHI<15, mean = 7/h (n=113;14 deaths) 100 Survival (%) 95 90 85 H.R. = 2.81 80 75 AHI ≥ 15/hr, mean = 33/h (n=41; 9 deaths) p = 0.029† 70 0 20 40 60 80 Time (months) M-NSA=mild to no sleep apnea OSA=obstructive sleep apnea † After adjusting for left ventricular ejection fraction, NYHA functional class, age Wang H et al. J Am Coll Cardiol. 2007; 49: 1632 Under-diagnosis of sleep apnea in patients with heart failure Study Cohort N=30,719 SA tested N=572 (2%) SA Dx: N=553 (97%) tested, diagnosed, not treated N=295 Not SA tested N=30,147 (98%) No SA Dx N=19 (3%) tested, diagnosed, treated N=258 Javaheri et al. Am J Respir Crit Care Med 2011 Sleep Medicine Physician Board Review Kaplan-Meier Survival Curves, Adjusted by Age, Gender, and Charlson Comorbidity Index, 2004-2005 Percent of Cohort Alive 100% Tested, Diagnosed, Treated, N=258 90% Not Tested, Not Treated, N=30,065 80% 70% Hazard ratio = .33 (95% CI = .21-.51), P <.0001 60% Baseline 1 2 3 4 5 6 Quarters after HF Onset Javaheri et al. Am J Respir Crit Care Med 2011 Sleep Medicine Physician Board Review 7 8 Cumulative event-free survival in CPAP-treated and untreated patients Cumulative Event Free Survival (%) 100 80 N=65 AHI: 45 /hr LVEF: 36 % 60 40 Treated N=23 Untreated 20 HR 2.03 (1.07-3.68) P=0.03 AHI: 38 /hr LVEF: 35 % 0 0 Kasai T, et al. Chest, 2008 12 24 36 Months Sleep Medicine Physician Board Review 48 60 Cumulative event-free survival by compliance status Cumulative Event Free Survival (%) 100 N=32 AHI: 46 /hr LVEF: 37 % 80 60 N=33 (6.0 hr/night) 40 AHI: 44 /hr LVEF: 35 % (3.5 hr/night) 20 HR 4.02 (1.33-12.2) P=0.014 0 0 Kasai T, et al. Chest, 2008 12 24 36 Months Sleep Medicine Physician Board Review 48 60 OSA Patients Die During Sleep Gami et al, NEJM, 2006 Sleep Medicine Physician Board Review If I can choose…… Dr, are you telling me that if I use my CPAP I will die during daytime while awake! I know you mean good, but I prefer to die during sleep Sleep Medicine Physician Board Review Author year n Age year LVEF % Mortality Statistical significance Hanly (96) 16 64 23 ↑ Yes Lanfranchi (99) 62 57 23 ↑ Yes Sin (00) 66 59 22 ↑ Yes Bradley (03) 258 63 25 ↑ Yes Leite (03) 84 42 34 ↑ Yes Corra (06) 133 58 23 ↑ Yes Javaheri (07) 88 62 25 ↑ Yes Brack (07) 60 58 29 ↑ Yes La Rovere (07) 380 52 25 ↑ Yes Andreas (98) 36 55 20 ↑ No Roebuck (04) 78 53 20 → No Jilek (11) 176 65 34 ↑ Yes CSA is an independent predictor of mortality in SHF • • • • N = 114 eligible N = 100 Enrolled N = 12 with OSA Excluded N = 88 32 with AHI <5/hr ( mean = 2 ) 56 with AHI ≥5/hr ( mean = 34 ; CAI = 23) • Median F/U : 51 months Javaheri et al , J Am Coll Cardiol (May, 2007) Sleep Medicine Physician Board Review CSA is a Predictor of Mortality in SHF 100 90 AHI < 5/h (n=32) 80 AHI ≥5/h (n=56) Survival % 70 60 50 40 30 20 Hazard ratio=2.14 10 P=0.02 0 0 10 20 30 40 50 60 70 80 90 100 110 120 130 140 150 160 170 Months Sleep Medicine Physician Board Review Javaheri S et al. J Am Coll Cardiol 2007 The predictors of poor survival in SHF Three variables, AHI , RVEF and DBP independently correlated with survival : AHI (HR=2.14, P=0.02) RVEF (HR=0.97, P=0.003) DBP (HR=0.96, P=0.02) Javaheri, JACC, 2007 Sleep Medicine Physician Board Review poor Heart-Transplantation-Free Survival Transplantation-free Survival (%) 100 80 CPAP group 60 Control group 40 20 P=0.54 0 0 12 24 36 48 60 Time from Enrollment (mo) Bradley TD et al., N Engl J Med 2005 Sleep Medicine Physician Board Review Treatment of sleep apnea with CPAP in SHF In regard to therapy with CPAP, how does CSA differ from OSA? Sleep Medicine Physician Board Review CSA in SHF Prevalence of CPAP-responders and nonresponders Patients n 21 Responders Non-responders 43% AHI(36 to 4/h) 57% AHI(62 to 62) Javaheri, Circulation, 2000 Sleep Medicine Physician Board Review Baseline Polysomnogram: HCSB CPAP Reasons why CPAP increased mortality 1. CPAP- nonresponders (43 % up to 57%) 2. Adverse hemodynamic consequences of CPAP: CPAP increases intrathoracic P and decreases venous return to R ventricle Javaheri , JCSM, 2006 Sleep Medicine Physician Board Review The predictors of poor survival in SHF Three variables, AHI , RVEF and DBP independently correlated with survival : AHI RVEF DBP poor HR=2.14, P=0.02 HR=0.97, P=0.003 HR=0.96, P=0.02 Sleep Medicine Physician Board Review Javaheri, JACC, 2007 Reasons why CPAP increased mortality 1. CPAP- nonresponders 2. Adverse hemodynamic consequences of CPAP: CPAP increases intrathoracic P and decreases venous return to R ventricle Javaheri , JCSM, 2006 Sleep Medicine Physician Board Review Reasons why CPAP increased mortality If my statements are correct, then: 1. CPAP responders should have a better survival than the control group, and 2. CPAP non-responders should have a poorer survival than the control group Sleep Medicine Physician Board Review Heart-Transplantation-Free Survival 100 Transplantation-free Survival (%) CPAP group, n=128 80 60 Control group 40 20 P=0.54 0 0 12 24 36 48 Time from Enrollment (mo) Bradley TD et al., N Engl J Med 2005 Sleep Medicine Physician Board Review 60 Transplant-free survival in SHF patients according to effect of CPAP on CSA (Artz, Circ, 2007) CPAP responders* (AHI at 3 months < 15/hr, n = 57) Transplant-free survival (%) 100 80 60 Control CPAP non-responders (AHI at 3 months 15/hr, n = 43) 40 20 * vs. control: HR=0.36, p=0.040 0 0 6 12 18 24 30 36 42 48 54 60 Time from enrollment (months) Sleep Medicine Physician Board Review Transplant-free survival (%) Transplant-free survival according to effect of CPAP on CSA CPAP responders* (AHI at 3 months < 15/hr, n = 57) 100 80 Control 60 CPAP non-responders (AHI at 3 months 15/hr, n = 43) 40 Control 20 *versus control: HR=0.36, 0 0 6 12 18 24 p=0.040 30 36 42 48 54 60 Time from enrollment (months) Sleep Medicine Physician Board Review CSA in SHF Prevalence of CPAP-responders and non-responders Potential Therapeutic Role of PSSV Devices Patients Javaheri (1st night) (Circulation,2000) Artz (at 3 m) (Circulation,2007) n Responders Non-responders 21 43% AHI (36 to 4/h) 57% AHI (62 to 62) (lowPCO2) 100 57% AHI (34 to 6.5) 43% AHI (47 to 35) Sleep Medicine Physician Board Review Regarding CPAP in CSA/SHF 2 important concerns: 1. CPAP non-responders 2. Poor adherence with CPAP in responders Sleep Medicine Physician Board Review ASV devices • VPAP Adapt ASV Enhanced • BiPAP AutoSV Advanced Sleep Medicine Physician Board Review General operation of ASV devices Hyperpnea Hypopnea Patients Airflow Device Inspiratory pressure support Expiratory pressure Inspiratory support decreasing during hyperpnea and increasing during hypopnea Operation of BiPap auto SV Advanced EP increased from 4 to7 cm H2O during obstructive disordered breathing events AHI comparative data across various nights (N=37) Javaheri et al, Sleep 2011, In Press 100 90 80 70 60 53.1 50 40 34.5 30 20 10.4 10 6.1 0 vs. Dx_PSG vs. autoSV Advanced Dx_PSG ----- CPAP <0.001 autoSV <0.001 autoSV Advanced <0.001 <0.001 <0.001 0.0354 ----- Effects of PAP treatment on survival in patients with SHF and severe sleep apnea Jilek et al. EJHF, 2011 100 PAP treated; AHI=49/h Survival, % 80 16 events, 18% 60 untreated ; AHI=42 44 events, 52% 40 adjusted HR 0.3 (95%CI: 0.2 – 0.6, p=0.001) 20 0 20 40 60 80 months Sleep Medicine Physician Board Review 100 Thanks for your attention Ref: S. Javaheri, Heart Failure in: Principles and Practice of Sleep Medicine, 2010 A patient with HCSB on VPAP Adapt Enhanced Sleep Medicine Physician Board Review • Cardiovascular changes in NREM & REM sleep NREM Sleep: – Sympathetic and Parasympathetic Activity – HR & BP – Ventilation – – Phasic REM sleep HR and BP • NREM sleep is peaceful for CV system • Phasic REM sleep is not peaceful for CV system Differences of ESS Score between HF patients (University of Toronto) and the GP (Madison Sleep Cohort) according to the AHI † Subjective Sleepiness (ESS Score) 11 † GP 10 † 9 8 † † HF 7 6 († p<0.05, †† p<0.01) 5 4 AHI < 5 AHI 5-15 Arzt M et al. Arch Int Med 2006 Sleep Medicine Physician Board Review AHI 15 Long-term CPAP adherence in OSA one year use of CPAP in nonsleepy OSA patients in the Spanish trial Adherence: 4.7 ± 2 hrs Barbe et al, Am J Respir Crit Care, 2010 Sleep Medicine Physician Board Review Kaplan-Meier Survival Curves, Adjusted by Age, Gender, and Charlson Comorbidity Index, 2004-2005 100% Percent of Cohort Alive Tested, Diagnosed and Treated N=258 Tested, Diagnosed and Not treated N=295 90% Hazard ratio =.49 (95% CI= .29-.84), P=0.009 80% Baseline 1 2 3 4 5 Quarters after HF Javaheri et al. Am J Respir Crit Care Med 2011 Sleep Medicine Physician Board Review 6 7 8 Future direction 2 RCT, one with VPAP Adapt Enhanced one with BiPap AutoSV Advanced are in progress in systolic heart failure Sleep Medicine Physician Board Review Prevalence of sleep apnea in Systolic Heart Failure 100 out of 114 consecutive patients 10% on beta blockers Javaheri et al : Ann Intern Med Circulation Int J Cardiol AHI ≥ 15/h 1995 1998 2006 49% Sleep Medicine Physician Board Review Prevalence of sleep apnea in 6 recent prospective PSG studies of SHF %AHI≥15/hr 70 %CSA %OSA 60 50 40 30 20 10 0 USA (06) Canada (07) UK (07) Germany (09) Germany (10) Prevalence of sleep apnea in 6 recent prospective PSG studies of SHF Country (year) n AHI≥15/hr USA (06) 100 Canada (07) CSA OSA 49 37 12 287 135 60 75 UK (07) 55 29 21 8 Germany (09) 50 32 22 10 Germany (10) 273 175 137 38 Portugal (10) 103 46 n/a n/a Total 868 466 277 143 Prevalence of sleep apnea in 6 recent prospective studies of SHF Prevalence of sleep apnea in 12 recent prospective studies of 2,423 consecutive patients with SHF Country (year) n *USA (06) AHI≥10/hr (n) AHI≥15/hr (n) CSA (n) OSA (n) 100 49 37 12 USA (08) 108 66 33 32 *Canada (07) 287 135 60 75 China (07) 126 58 32 *UK (07) 55 29 21 8 Germany (07) 700 364 231 133 Germany (07) 203 144 57 87 Germany (07) 102 55 38 17 France (09) 316 256 79 177 *Germany (09) 50 32 22 10 *Germany (10) 273 175 137 38 *Portugal (10) 103 46 n/a n/a Total 2,423 896 773 621 89 544 Prevalence of sleep apnea in recent prospective studies of SHF Country (year) n % AHI≥10/hr % CSA % OSA % β blockers China (07) 126 71 46 25 80 Germany (07) 203 71 28 43 90 Germany (07) 102 54 37 17 80 France (09) 316 81 25 56 82 Total 747 73 31 42 84 Prevalence of sleep apnea in recent prospective studies of SHF Country (year) n % AHI≥15/hr % CSA % OSA % β blockers * USA (06) 100 49 37 12 10 USA (08) 108 61 31 30 82 *Canada (07) 287 47 21 26 80 *UK (07) 55 53 38 15 78 Germany (07) 700 52 33 19 85 *Germany (09) 50 64 44 20 100 *Germany (10) 273 64 50 14 88 *Portugal (10) 103 46 n/a n/a 90 Total 1676 54 34 20 81 Prevalence of sleep apnea in SHF (blue=EEG/red=no EEG) Prevalence of sleep apnea in 2 recent polygraphy studies of SHF (n=808) AHI≥15/hr CSA OSA Prevalence of Sleep Apnea in Recent Prospective Studies of SHF n Country (y) US (06) US(08) Canada (07) China (07) UK (07) 126 55 700 Germany (07) 203 102 % AHI ≥ 15/hr 49 61 47 100 108 287 Germany (07) Germany (07) % AHI ≥ 10/hr % β blocke 10 82 80 80 71 53 52 78 85 71 90 54 80 Prevalence of Sleep Apnea in SHF The World Series n = 431 n = 1250 AHI ≥10 AHI ≥15 Prevalence of CSA in Systolic Heart Failure 100 out of 114 consecutive patients 49% with AHI ≥ 15/h 37% CSA Javaheri et al: Ann Intern Med 1995 Circulation 1998 Int J Cardiol 2006 Prevalence of Sleep Apnea in Recent Prospective Studies of SHF n Country (y) US (06) US(08) Canada (07) China (07) UK (07) 126 55 700 Germany (07) 203 102 % % AHI ≥ 15/hr CSA % β blocke 37 31 21 10 82 80 46 80 38 78 33 85 71 28 90 54 37 80 49 61 47 100 108 287 Germany (07) Germany (07) % AHI ≥ 10/hr 71 53 52 Prevalence of CSA in SHF The World Series 40 35% 31% 35 30 25 % n = 431 n = 1250 20 15 10 5 0 AHI ≥10 AHI ≥15 Prevalence of CSA in Systolic Heart Failure 100 out of 114 consecutive patients 49% with AHI ≥ 15/h 12% OSA Javaheri et al: Ann Intern Med 1995 Circulation 1998 Int J Cardiol 2006 Prevalence of OSA in SHF Recent Studies n Country (y) US (06) % AHI ≥ 10/hr % AHI ≥ 15/hr 49 100 Canada (07) 287 55 UK (07) % OSA 12 26 47 53 52 Germany (07) 700 15 19 43 Germany (07) 203 71 Germany (07)102 54 17 China (07) 71 25 126 % β blocke 10 80 78 85 90 80 80 Prevalence of OSA in SHF The World Series 35 30 32 n = 431 25 % 20 20 n = 1250 15 10 5 0 AHI ≥ 10 AHI ≥ 15 World wide prevalence of sleep apnea in systolic heart failure Author, Country (y) n AHI > 15/hr % B blockers % Javaheri, USA (06) 100 49 10 MacDonald, USA (08) 108 61 82 Wang, Canada (07) 287 47 80 Vazir, UK (07) 55 53 78 Oldenburg, Germany (07) 700 52 85 Worldwide prevalence of sleep apnea in 1250 consecutive patients with SHF 60 52 50 40 % 31 30 21 20 10 0 AHI ≥15 CSA OSA Sleep Medicine Physician Board Review Prevalence of Sleep Apnea in Heart Failure with PEF(n=244) AHI≥15/hr Prevalence of sleep apnea in 6 recent prospective PSG studies of SHF 54% (467/868) 36% (277/765) 19% (143/765) Prevalence of Sleep Apnea in Heart Failure with PEF • Patients with SA performed worse on exercise test and 6 minute walk • With increasing impairment of diastolic dysfunction the prevalence of SA, and CSA in particular increased • Patients with CSA had lower PCO₂, higher NT-proBNP, LVEDP, PCWP, and PAP Sleep Medicine Physician Board Review How frequently patients with HF are tested for SA? Among a population of 30,719 newly diagnosed HF patients, only 1,263 (4%) were clinically suspected to have SA. Of these, 553 (only 2% of the total cohort) were tested for SA. Javaheri et al, AJRCCM, 2011 Sleep Medicine Physician Board Review How frequently patients with HF are tested for SA? A retrospective cohort study used the 2004-2005 Medicare Standard Analytical Files (SAFs). SAFs contain a 5 % sample of randomly selected Medicare beneficiaries. The study population included newly diagnosed HF patients in the first quarter of 2004 without prior diagnosis of SA. Javaheri et al. Am J Respir Crit Care Med 2011. Sleep Medicine Physician Board Review Phenotype of heart failure patients with and without sleep apnea 90 NO SA CSA OSA *† 80 p=0.02 p=0.1 70 p=0.1 60 50 p<0.001 40 *† p=0.8 30 20 10 0 Patients (n) *vs. Group I Group II †vs. Age (y) Ht BMI Snoring (in) (kg/m2) (%) Sleep Medicine Physician Board Review EDS (%) PAP devices decreases LV afterload Normal Hypertension 100 Ppl 100 Pr LVTm Ppl 100 - (0.0) = 100 Ppl -40 140 - (0.0) = 140 100 100 140 0.0 CPAP 100 140 Ppl 0.0 UAO 100 +10 100 - (-40) = 140 100 - (+10) = 90 OSA , HF and CPAP 1.CPAP titration in OSA with heart failure is the same as OSA without HF 2. Generally, OSA is eliminated with overnight CPAP titration 3.Occasionally central apneas may occur during titration with CPAP 4.In most patients, OSA is controlled with low pressure What is critical is long-term adherence Sleep Medicine Physician Board Review CPAP adherence in OSA What is a major determinant of long-term adherence to CPAP in OSA patients ? Sleep Medicine Physician Board Review Optimize Therapy of Heart Failure ACEI; ß-Blockers; Diuretics; Digoxin; CRT SRBD Eliminated Follow-up Clinically Cardiac Transplantation Nocturnal Nasal Oxygen Medications Theophylline Persistent SRBD Consider Treatment Phrenic Nerve Stimulation Acetazolamide Positive Airway Pressure Devices CPAP Bilevel ASV Changes in AHI with low flow nasal O2 in CSA patients with heart failure and systolic dysfunction 80 70 p<0.0001 Room Air Oxygen Apnea-Hypopnea Index (n/hr) MeansSD 60 p=0.01 p<0.05 p<0.001 50 p<0.01 p=0.02 40 30 20 10 0 N=9 Hanly N=7 Walsh N=11 Staniforth N=7 Franklin N=22 Andreas N=29 Javaheri RCT : Theophylline Improves CSA Baseline Placebo Theo Variable 15 15 15 N 15/0 15/0 15/0 Gender, M/F 66 66 66 Age, y 175 175 175 Ht, cm 89 88 88 Wt, kg ND ND 11 Theo, ug/ml Javaheri et al., NEJM, 1996 Values are means; ND=not detectable RCT:Theophylline improves CSA in HF Variable Baseline Placebo Theo 37 18* AHI, n/h 47 26 6* CAI, n/h 26 2 2 OAI, n/h 2 2 1 MAI, n/h 2 17 8* DBArI, n/h 24 Javaheri et al., NEJM, 1996, 335, 562-7 Values are means; * p < 0.05 RCT: Disordered breathing events of 12 SHF patients with CSA treated with single dose of acetazolamide before bedtime Variable Baseline AHI, n/h 55 CAI, n/h 44 OAI, n/h 1 DBArI, n/h 25 Placebo 57 49 1 20 Actz 34*† 23*† 2 13 p < 0.05 versus baseline † = p < 0.05 versus placebo Javaheri, Am J Respir Crit Care Med, 2006 p 0.002 0.004 0.6 0.06 Long-term CPAP adherence in SHF is inadequate (Arzt, Circulation, 2007) AHI (n/hr) CPAP-CSA suppressed n=57 6 CPAP-CSA unsuppressed n=43 35 P (cm H2O) 9 9 CPAP use at 3 m (hr) CPAP use at 12 m (hr) 4.6 4.2 3.6 3.6 Bi-level Pressure cm/H₂O 20 Fixed inspiratory pressure 15 Fixed inspiratory support = IPAP - EPAP 10 Fixed expiratory pressure 5 0 VPAP Adapt SV Enhanced Pressure cm/H₂O 25 18 Variable inspiratory pressure support Max inspiratory P = 25 Default min pressure support 3 Default max pressure support 5 7 4 Fixed expiratory pressure (Manually adjusted) 0 BiPAP Auto SV Advanced Pressure cm/H₂O 25 Max inspiratory P = 25 18 11 4 0 Min expiratory P = 4 with automatic adjustment Variable inspiratory pressure support Min inspiratory support = 0 Max pressure support = 25 – instantaneous EPAP Features of ASV devices EP to eliminate obstructive events. – Back up rate to abort any impending apnea – Variable inspiratory support which with hypopneas and with hyperpneas – Sleep Medicine Physician Board Review