Examination of the Renal Patient
advertisement

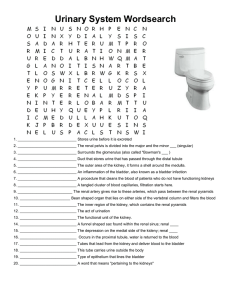
Examination of the Renal Patient P E T ER L AT HA M F Y2 Plan 30 minutes Treat it as a mock final What to expect before finals History Examination Investigations Management Common Questions What are the ‘classic’ Renal Cases? • PCKD • CRF • Renal Transplant In the hospital all the time for dialysis Most will have some sort of sign Still the chance to get something more exotic BUT the theme will always be around Renal Failure History No presenting compliant to work with!! ‘This man is on dialysis. Please find our more.’ ‘This lady is known to the Renal Physicians. Please find out more.’ Classic Chronic Disease history History Introduction Timeline PC – lethargy, HTN, Blood Test, Kidney problems as a child, family history of kidney disease From diagnosis – how have they progressed – when started dialysis, what types etc Bring it back to the present Screen for complications Stay focussed – keep it renal Roles of the Kidney All symptoms arise from the different roles of the kidney, failing 1. Calcium Homeostasis Can’t convert to active form of Vitamin D (calcitriol) and can’t reabsorb Calcium Renal Patients can suffer from hypocalcaemia and hypercalcaemia depending on whether the are secondary or tertiary Hyperparathyroidism Hypo – cramps, tingling peripherally Hyper – Bone pain, constipation, kidney stones 2. Blood pressure and Fluid Homeostasis Excretion of water is key If not – it accumulates Peripheral Oedema – ‘ankles swelling’ Pulmonary Oedema – orthopnea ‘how are you lying flat?’ 3. Acid Base balance Kidney key role in the longterm control of pH Excretes H+ and reabsorbs HCO3 Acidosis key symptoms – N&V 4. Electrolyte Balance Key role in retaining sodium and excreting potassium Hyperkalaemia – lethargy, muscle paralysis, chest pain Hyponatraemia – muscle cramps, anorexia, N&V 5. Erythropoietin Produces EPO Anaemia is common throughout patients with CKD Symptoms – lethargy, pallor, cold peripheries, chest pain, dizziness PmHx Open question (could ask them for a cause?) ASK SPECIFICALLY FOR Diabetes HTN Childhood infections Drugs, Operations, Allergies Drugs – NSAIDs Ops – Transplant Sx Smoking Smoking Smoking Smoking Alcohol Work with dyes Fx PCOS Artheriopaths ICE Do ICE early but not too early Tricky because they will clearly have a good Idea what is going on!! All about wording ‘First had symptoms – did you have any Idea what was going on?’ ‘What concerns you the most about your current condition’ ‘Has the care you have received met your expectations?’ Examination Examiner – ‘What is exam would you like to do?’ Essentially a GI/General Exam Talk to them, be confident, take control ‘What I would like to do……’ End of Bed Well or unwell Breathing comfortably at rest (compensating for acidosis) Colour – pallor (anaemia) Can you see a fistula? Hands Pallor, perfusion Gouty Tophi Lindsay’s nails Pulse Fistula???? Offer Blood pressure Face Pallor in Conjunctiva, Xanthelasma Offer Fundoscopy – Hypertension retinopathy, End-organ damage Assess JVP Abdomen Inspect and comments (Transplant scars in flanks) Palpate – as per GI exam, ballot kidneys Percuss – liver, spleen and bladder Auscultate – renal bruits, and offer lung bases Ankles for oedema Fistula No different to anything other examination Inspect – signs of infection, wound breakdown, aneurysms Palpitate (careful!), again signs of inflammation, should feel vibration Auscultate – bruits to confirm function Offer Cardiovascular Exam Neuroexam (PCKD) Investigations Bedside Tests Blood pressure in both arms, lying and standing ECG – hyperkalaemia!!! Urine dip – Protein! Albumin Creatinine ratio (or protein creatinine ratio) WEIGHT Bloods FBC – Anaemia U&E – urea and creatinine Bone – Calcium and phosphate LFTs – ALP raised due to renal bone disease Parathyroid Hormone VBG or ABG - acidosis Imaging AxR – suspecting renal calculi USS – non-invasive, size, shape, Structural abnormalities CT – stones BUT always mention use of contrast MRA – preferable if suspecting Renal Vascular Disease Special Tests –Renal Biopsy (rarely done due to complications) Management - Conservative Lots of MDT players Renal Physicians Renal Specialist Nurse Dieticians GP – most should be managed in primary care Immunisations Psychological support Patient education – diet, symptoms of decompensation Management - Medical Best Medical care Control Hypertension Reduce Cardiovascular risk – statins, antiplatets Bone disease – calcium and vitamin D supplements Anaemia – EPO injections Stringent Diabetic Control Avoid all nephrotoxins especially NSAIDs Surgical Transplant and immunosuppression Questions Try to think about these in your thinking time Definition Epidemiology Pathophysiology Risk Factors/Causes Indications for treatment Acute on Chronic Presentations – Hyperkalaemia, Pulmonary Oedema, Acute Kidney Injury Any Questions???