(Insert Catchy Title )
advertisement
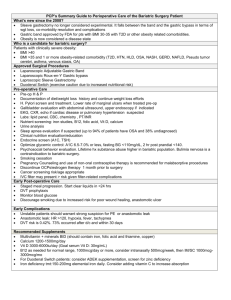
An Overview of Bariatric Surgery Kristin Dermody Angela Illing May 23, 2005 THE OBESITY EPIDEMIC A Quick Background of Obesity Derived from the Latin word obesus – “to devour” Definition: having a very high amount of body fat in relation to lean body mass Classifications using Body Mass Index (BMI) BMI Categories A BMI of: <18.5 18.5-24.9 25-29.9 30-34.9 35-39.9 40-49.9 50 and above Classifies one as: Underweight Normal weight Overweight Obesity Class I Obesity Class II Obesity Class III Super Obesity Obesity is a BIG problem… 1.7 billion worldwide are overweight or obese The US has a higher percentage of overweight and obese people than any country in the world And the numbers are growing… US Incidence of Obesity Approximately 2/3 of the United States population is overweight. Of those, almost 50% are obese. In total, approximately 5% of the US population is morbidly obese Alarmingly, the BMI subgroups growing the most quickly are 35 or higher and 40 or higher. Massachusetts: Not-so-’Phat’ Facts 55% of Mass adults overweight or obese* Of these obese adults** 18% non-Hispanic white 30% non-Hispanic black 22% Hispanic 24% of Mass high school students overweight or at risk of becoming overweight Obesity rate among Mass adults by 81% from 1990 to 2000* *CDC BRFSS, 2002; **CDC YRBSS, 2003 History of Obesity Obesity Trends* Among U.S. Adults BRFSS, 1985 (*BMI ? 30, or ~ 30 lbs overweight for 5’ 4” person) 1985 No Data <10% 10%–14% Source: Behavioral Risk Factor Surveillance System, CDC. Obesity Trends* Among U.S. Adults BRFSS, 1991, 1996, 2003 (*BMI 30, or about 30 lbs overweight for 5’4” person) 1991 1996 2003 No Data <10% 10%–14% 15%–19% Source: Behavioral Risk Factor Surveillance System, CDC. 20%–24% ? 25% Potential Consequences of Obesity Obesity is associated with a rise in many comorbid conditions, including: Type 2 Diabetes Hyperlipidemia Hypertension Obstructive Sleep Apnea Heart Disease Stroke Asthma Back and lower extremity weightbearing degenerative problems Cancer Depression AND MORE! CVD & Obesity Fact: Obesity contributes to these co-morbid conditions, however… Recent JAMA article by Gregg et al* suggests CVD risk factors across all BMI groups over past 40 years Suggest: Overweight not quite as bad as it once was, considering other factors: Risk r/t awareness, aggressive identification, pharmacological tx of high chol, HTN. Note: Obese persons still have risk factor levels vs..lean persons. Gregg EW, et al. Secular Trends in Cardiovascular Disease Risk Factors According to Body Mass Index in US Adults. JAMA, 2005:293:1863-1874 Impact of Obesity These comorbid conditions are together responsible for more than 2.5 million deaths per year worldwide*. This is in addition to billions of dollars in healthcare costs and lost productivity. *World Health Organization, World Health Report 2002 Obesity and Life Expectancy Recent NEJM article* – If current rates of obesity are left unchecked, the current generation of American children will be the first in two centuries to have a shorter life expectancy than their parents. The life-shortening impact of obesity (currently estimated at 1/3 to ¾ year) could rise to 2 to 5 years, or more, as obese children spend more years at risk for comorbid conditions. Olshansky SJ, et al. A Potential Decline in Life Expectancy in the United States in the 21 st Century. NEJM, 352(11):1138-1145, 2005 Obesity and Life Expectancy The morbidly obese are perhaps the worst off… Compared to a normal-weight person, a 25year-old morbidly obese man has a 22% reduction in expected remaining lifespan. This is an approximate loss of 12 YEARS! This number will also likely grow if the everexpanding numbers of currently obese children continue as obese adults… TREATING OBESITY Weight Loss Strategies Diet therapy Increased Physical Activity Pharmacotherapy (e.g., Orlistat, Meridia) Behavioral Therapy Hypnosis Any combination of the above Bariatric Surgery An effective treatment for combating obesity Bariatric Surgery 1991: NIH establishes guidelines for the surgical therapy of morbid obesity Recommends BMI criteria BMI > 40 BMI > 35 + significant comorbidities This therapy now referred to as Bariatric Surgery Types of Bariatric Surgery Purely Restrictive Restrictive > Malabsorptive Short-limb/Roux-en-Y gastric bypass (BWH) Long-limb/distal Roux-en-Y gastric bypass Malabsorptive > Restrictive Gastric Balloons (not approved for use in USA) Vertical-banded gastroplasty Gastric adjustable banding (BWH) Biliopancreatic diversion (BPD) BPD with duodenal switch Very long limb Roux-en-Y gastric bypass Purely Malabsorptive Jejunoilieal bypass Jejunocolonic bypass A Brief History of Bariatric Surgery First developed: Pts with short bowel syndrome weight loss First weight loss surgeries (ca. 1950s) Intestinal bypass Low-risk surgically BUT many patients developed serious and often fatal complications Biliopancreatic diversion Effective BUT with high risk and many complications Evolution of the Roux-en-Y Gastric partitioning (Roux-en-Y GBP) Based on observations of weight loss in pts receiving subtotal gastric resections for other conditions 1967 – First performed Continues to be studied and refined Roux-en-Y Open* 2 hour procedure 3 days in-house 4 weeks – Return to work 60-70% EBW loss @ 2 yrs 0.5-1.0% Risk of Death Dumping Syndrome Laparoscopic* 2-4 hour procedure 3 days in-house 2-3 weeks – Return to work 60-70% EBW loss @ 2yrs 0.5-1.0% Risk of Death Dumping Syndrome * Data based on averages. Evolution of Gastric Banding 1970s 1980s Alternative to Roux-en-Y in Europe & Scandinavia Adjustable silicone band developed 1990s Laproscopic techniques for placement developed Gastric Banding Adjustable Lap Band 1 hr procedure 1 day in-house 1 wk – Return to work 40-45% EBW loss @ 2 yrs <0.1% Risk of Death Self-sabotage easier Who Gets Bariatric Surgery? Gender Age 19% Males 72.6% Females (8% gender not reported) Mean age 39 years Range 16-64 years BMI Mean BMI 46.9 Range 32.3-68.8 Buchwald H, et al. Bariatric Surgery: A Systematic Review and Meta-analysis. JAMA, 14:1724-37, 2004 Medical Nutrition Therapy and The Post-op Bariatric Patient Post-Surgical Nutrition Balanced/healthy diet Liquids to pureed to soft to solid* High nutrient density, quality Modified in lactose, fat, sugar Adequate fluid Portion Control Meal Periods/Eating time MVI/MIN Ca (>1200mg/d) + D (10-20mg) Folate (800-1000mcg) +B12 Iron (45-100mg elemental – premenstrual) Vitamin C (75-100mg) Thiamin Self-monitoring Eating triggers/behaviors Exercise * Time line may vary among institutions Post-Op Roux-En-Y Diet Stage One (1 day) Water and clear liquids Non-caloric, noncarbonated, noncaffeinated liquids Fluid goal: 28-32oz/d Stage Two (14 days) High protein, low sugar beverages Fluid goal: 56oz Protein goal: 60-70g/d Chewable MVI + Ca Post-Op Roux-En-Y Diet Stage Three (4 weeks) 5 – 2oz servings diced protein Fluid goal: 56oz Protein goal: 60-70g Chewable MVI + Ca Stage Four (4 months) 3 meals, 2 snacks 850kcal/d Fluid goal: 56oz Protein goal: 60-70g Chewable MVI + Ca Stage Five (ongoing) Regular Meals 1200-1500kcal Fluid & Protein goals: same as above Post-op Lap Band Diet Stage One (1 day) Water & Clear Liquids Non-carbonated, non-caffeinated, non-caloric liquids Fluid goal: 28-32oz/d Stage Two (14 days) 5-8oz servings of High Protein, low sugar Beverage Fluid goal: 56oz Protein goal: 50-60g Chewable MVI + Ca Post-op Lap Band Diet Stage Three (14 days) Pureed Foods, Semi solids 2 small meals, 3 snacks Fluid goal: 56oz Protein goal: 50-60g Chewable MVI + Ca Stage Four (ongoing) Regular meals: 3 meals,2 snacks (1000-1200) Fluid goal: 56oz Protein goal: 50-60g Chewable MVI + Ca Post-Surgical Nutrition & Exercise RD seen frequently 1m 3m 6m 1yr Exercise No heavy lifting or exercise 6-8wks post-op Walking daily OK, encouraged After cleared, strength training important to help skin stretch back Helps with weight loss in the long run When Surgery and Follow-Up Go Well… Efficacy of Bariatric Surgery for Weight Loss Mean percentage excess weight loss: 61.2% - All Patients 47.5% - Gastric Banding 61.6% - Gastric Bypass 68.2% - Gastroplasty 70.1% - BPD or duodenal switch *Buchwald H, et al. Bariatric Surgery: A Systematic Review and Meta-analysis. JAMA, 14:1724-37, 2004 Roux-en-Y: Metabolic Sequelae Human body regulates nutrient intake over time by secreting hormones Over 40 hormones play a role in regulation of feeding. Roux-en-Y: Metabolic Sequelae Two types: Satiety hormones Short-term Help regulate meal size; daily intake Secretion decreases meal size; reduces time to stop Includes (among others) cholecystokinin, amylin, glucagonlike-peptide 1 (GLP-1), enterostatin, and bombesin Adiposity hormones Long-term Related to energy stores Secretion delays onset of beginning of meal Includes insulin, leptin Roux-en-Y: Metabolic Sequelae Also of note is ghrelin, the endogenous ligand for the growth hormone secretagogue receptor Mostly secreted in the fundus of the stomach (part bypassed in RYGB) Contrary to satiety hormones, ghrelin is orexigenic – i.e., increases appetite (fasting increases levels) Roux-en-Y: Metabolic Sequelae Plasma ghrelin normally increases after non-surgical weight loss This supports long-term weight homeostasis Proportional to lean body mass Initial report showed circulating plasma ghrelin greatly decreased in pts s/p RYGB Past theory: exclusion of the fundus of the stomach responsible for lower ghrelin levels (and therefore greater weight loss) Roux-en-Y: Metabolic Sequelae Studies since then have shown no change or increase in ghrelin after bypass Additionally, found that post-pyloric nutrient stimulation vs.. stomach distention responsible for changes in ghrelin levels Does not support idea that bypassing stomach fundus responsible for changes, if any, in ghrelin levels Overall, still not well understood Strader AD, et al. Gastrointestinal Hormones and Food Intake. Gastroenterology, 128:175-91, 2005 Roux-en-Y: Metabolic Sequelae Further investigation is needed, but thought that one reason certain types (i.e., RYGB) of bariatric surgery are successful at reducing food intake and causing weight loss may be related to enhanced secretion of satiety signals (ghrelin or others). Effect on Comorbid Conditions Diabetes Hyperlipidemia 70% - Improved HTN 76.8% - Completely resolved 86.0% - Resolved or improved 61.7% - Resolved 85.7% - Resolved or improved Obstructive Sleep Apnea 83.6% - Resolved 85.7% - Resolved or improved Buchwald H, et al. Bariatric Surgery: A Systematic Review and Metaanalysis. JAMA, 14:1724-37, 2004 Metabolic Changes and Diabetes Many metabolic changes contribute to improvement and/or resolution of DM s/p bariatric surgery: Recovery of acute insulin response Decreases of inflammatory indicators (C-reactive protein and interleukin 6) Improvement in insulin sensitivity correlated w/increases in plasma adiponectin Changes in the enteroglucagon response to glucose Reduction in ghrelin levels (s/p RYGB, but not banding) Improvement in beta cell function (s/p banding, but not RYGP) Effect on Quality of Life Studies show overall QOL greatly improved Relief from comorbidities Improved appearance Perception of improved: Well-being Social function Body self-image Self confidence Ability to interact with others Increased time spent in recreational and physical activities Enhanced productivity Increased economic opportunities Often new employment More lucrative employment PROBLEMS AND COMPLICATIONS of Bariatric Surgery Possible Complications of Bariatric Surgery General Complications Pulmonary embolism Incisional hernia Gallstone formation Major wound infection and seroma Abdominal fluid collection Subphrenic abscess Peritonitis Procedure-Specific Complications (RYGB) Anastomotic or staple-line leak Acute gastric distention Staple-line disruption Stomal stenosis Stomal ulceration Small-bowel obstruction Occlusion of Roux limb Intermediate Complications Wound Infection Intra-abdominal bleed Gastric remnant necrosis Ischemic Roux-limb Internal hernia Long-Term GI Complications Nausea Constipation Abdominal pain Marginal ulcers Incisional hernias Vomiting Diarrhea Gallstones Gastritis Intestinal Obstructions Incidence of Complications Operative mortality (< 30 days): 0.1% for Purely Restrictive Procedures 0.5% for Gastric Bypass 1.1% for BPD or Duodenal Switch Long-Term Nutrition Complications Malnutrition Vitamin and mineral deficiencies Weight loss failure Dehydration Anemia Dumping Syndrome Hair loss Dry skin Risk of Vitamin and Mineral Deficiencies Post-op Calcium and Vitamin D Iron Absorption decreased d/t decreased contact of food with gastric acid; reduced conversion of iron from ferrous to ferric form (MVI) Vitamin B12 Reduced absorption d/t bypassed duodenum, proximal jejunum (R-en-Y) Life-long supplements mandatory Absorption decreased d/t decreased contact with intrinsic factor 60% of patients require long term supplementation of B12 Thiamine Connection to Wernicke’s syndrome Cases not well documented Post-Surgical Eating Avoidance Disorder (PSEAD) De novo synthesis of eating disorders postGBP Do not fit criteria for AN, BN, or BED No history pre-operatively Classify now as EDNOS Characteristics consistent enough to suggest new eating disorder Post-Surgical Eating Avoidance Disorder (PSEAD) Proposed Criteria: Previous h/o morbid obesity followed by bariatric surgery over the last 2 years Higher speed of weight loss than the average Use of purgative strategies or excessive reduction of food intake, related or not related to binge eating episodes Post-Surgical Eating Avoidance Disorder (PSEAD) Proposed Criteria: Reaction of extreme anxiety +/or negative attitude when nutritional correction introduced Intense fear of going back to pre-op wt Does not accept attempts to interrupt the wt loss Denies doing something exaggerated that account for loss Perceives a positive return with wt loss in spite of evidence to the contrary Post-Surgical Eating Avoidance Disorder (PSEAD) Proposed Criteria: Body image dissatisfaction or distortion Follow-up nutritional tests (such as laboratory tests) alterations that are significant and/or not in line with the surgical technique, maintained for more than 2 months after initial interventions Exclude AN and BN, according to DSM IV Exclude Simple Phobias (I.e., Food or Choking Phobia) according to DSM IV Exclude organic causes as the most probable factor for excessive weight loss Segal et al. Post-Surgical Refusal to Eat: Anorexia Nervosa, Bulimia Nervosa or a New Eating Disorder? A Case Series. Obes Surg, 14:353-359, 2004 Post-Surgical Eating Avoidance Disorder (PSEAD) A proposed ED classification Not yet part of the DSM IV ED: Contraindication for GBP? Pt with h/o of AN or BN likely not a good surgical candidate Pt at high risk for malnutrition after surgery Some with h/o ED receive surgery Important to screen carefully before AND monitor closely post-op to prevent relapse of disorder, malnutrition. Long Term Impact & Future Directions Long-Term Changes: Weight Regain One study of 342 gastric bypass pts showed excellent long-term weight maintenance: % weight loss at: 1 year (89%) 2 years (87%) 5 years (70%) 10 years (75%) However, potential for pouch stretch, selfsabotage, etc. leading to weight regain over time. Surgery relatively new, will have to wait and reanalyze data in a few years. “Long-term changes in energy expenditure and body composition after massive weight loss induced by gastric bypass surgery” Das SK, et al. Am J Clin Nutr. 2003;78:22-30. Study: EE & Body Composition Objective: To determine changes in energy expenditure and body composition with weight loss after gastric bypass surgery; to identify pre-surgery indicators of weight loss. Study: EE & Body Composition Design & Methods: Included 30 obese men and women Average age 39.0 + 9.6 y Average BMI (kg/m2) 50.1 + 9.3 Tested longitudinally under weight-stable conditions before surgery and after weight loss and stabilization (14 + 2 mo) Measured total energy expenditure (TEE), resting energy expenditure (REE), body composition, and fasting leptin Study: EE & Body Composition Results: Weight loss 53.2 + 22.2 kg body weight Significant reduction in REE (-2.4 + 1.0 MJ/d; P < 0.001) and TEE (-3.6 + 2.5 MJ/d; P < 0.001). Changes in REE predicted by changes in fat-free mass and fat mass Average physical activity level (TEE/REE) was 1.61 at both baseline and follow-up (P = 0.98) Weight loss predicted by baseline fat mass and BMI but not by any energy expenditure variable or leptin. Measured REE at follow-up was not significantly different from predicted REE. Study: EE & Body Composition Conclusions: TEE and REE decreased by 25% on average after massive weight loss and weight stabilization after gastric bypass Decreases in REE largely or completely predicted by decreases in body FFM and fat mass Fasting leptin at baseline found not to be a predictor of energy efficiency/changes, as some previous studies had shown Study: EE & Body Composition Conclusions: Suggested further studies to examine other explanations for variability in weight loss between patients after gastric bypass surgery ? Psychological, behavioral factors Suggested permanent reduction in energy intake critical for long-term weight management Other Future Weight Loss Strategies Gastric stimulation – idea of placing a pacemaker-like device in stomach to control contractions; release of hunger/satiety hormones Hormone therapy - “exendin-4” Hormone produced in Gila monster salivary gland Similar to GLP-1 in humans Reduces gastric emptying Lowers fasting plasma glucose Reduces food intake May prove effective therapy for DM, obesity OTHER CONCERNS Nutrition Support in the Critically Ill GBP Patient Enteral feeding possible, if warranted: Tube surgically placed in excluded stomach (RYGBP) Nasoenteric tube placed endoscopically through pouch If neither option possible (e.g. if pt has anastomotic leak) TPN. Bariatric Surgery in Special Populations Adolescents Elderly (over 60) Adolescents Few medical centers currently performing bariatric surgery on this population Only extreme cases Highly controversial given incomplete growth period Specialized medical team only Elderly Advanced age common contraindication to surgery Research suggests age may not be as indicative of outcome as once believed Successful GBP cases in 60+* St.Peter, Shawn. Impact of Advanced Age on Weight Loss and Health Benefits After Laparoscopic Gastric Bypass. Arch Surg; 140:165-168;2005 Spouses of GBP Patients Study by Madan AK, et al (2005) showed gastric bypass patient’s spouses who are obese are more likely to have weight gain while the patients lose weight after surgery Suggest pre-operative counseling for spouses or even consider them for surgery as well Summary Bariatric surgery is a seemingly effective therapy for morbid obesity that is gaining in popularity and prevalence Bariatric surgery provides significant Loss of excess body weight Relief from comorbidities: DM, HTN, hyperlipidemia Improvement in QOL for patients However, these surgeries put pts at risk for Post-op complications & mortality Nutritional deficiencies & GI complications Psychosocial complications References Kim JJ, et al. Surgical Treatment for Extreme Obesity: Evolution of a Rapidly Growing Field. Nutr Clin Prac 18:109-23, 2003 Buchwald H, et al. Bariatric Surgery: A Systematic Review and Meta-analysis. JAMA, 14:1724-37, 2004 Olshansky SJ, et al. A Potential Decline in Life Expectancy in the United States in the 21st Century. NEJM, 352(11):1138-1145, 2005 Merkle EM, et al. Roux-en-Y Gastric Bypass for Clinically Severe Obesity: Normal Appearance and Spectrum of Complications at Imaging. Radiology, 234(3):674-83, 2005 Segal et al. Post-Surgical Refusal to Eat: Anorexia Nervosa, Bulimia Nervosa or a New Eating Disorder? A Case Series. Obes Surg, 14:353-359, 2004 Madan AK, et al. Weight changes in spouses of gastric bypass patients. Obes Surg, 15(2):191-4, 2005 References Strader AD, et al. Gastrointestinal Hormones and Food Intake. Gastroenterology, 128:175-91, 2005 Das SK, et al. Long-term changes in energy expenditure and body composition after massive weight loss induced by gastric bypass surgery. Am J Clin Nutr. 2003;78:22-30.