Dental Benefits From The General Dentist's Perspective
advertisement

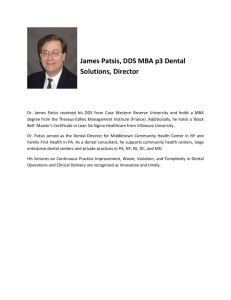
THERAPISTS & ADVOCACY Presented By Carter Brown, DMD, FAGD, FACD, FICD, FPFA Vice President, Academy of General Dentistry Why the Interest? What the Policy Makers See 82 million with limited care The Governmental Efforts & Safety Nets • Populations underutilizing available services • Up to a third of the population do not get care from the Private Market • Depends on a set of uncoordinated programs and policies: – Systems: FQHCs, VA, HIS – Policies: Medicaid, CHIP – Other: Volunteer Pro Bono Care, Free Clinics, Dental Schools, Corporate Medicaid practices, other community and public health programs • Limited capacity and overall has not addressed the underutilization in substantive way Policy Makers Are Looking at the Wrong Things They Don’t Understand, You Can Never Get 100% DENTAL VISITS IN THE LAST YEAR Source: National Healthcare Disparities Report 2005, Department of DHHS 1996 MEPS < FPL 100 < 200% 200 < 400% 400% + Total 2004 MEPS < FPL 100 < 200% 200 < 400% 400% + Total Visit 4,320,000 4,650,000 12,750,000 10,170,000 31,890,000 No visit 9,210,000 10,250,000 10,530,000 5,540,000 35,530,000 Total 13,530,000 14,900,000 23,280,000 15,710,000 67,420,000 4,410,000 5,700,000 11,860,000 13,620,000 35,590,000 7,910,000 9,120,000 10,990,000 6,140,000 34,160,000 12,320,000 14,820,000 22,850,000 19,760,000 69,750,000 Source: IADR March 2007, Medical Expenditure Panel Survey DHHS Responses: • OIG Report on EPSDT Dental Service Utilization (1996) – < 1-in-5 getting any dental services • HCFA/HRSA Oral Health Initiative (1990s) • Surgeon General’s Conference, Workshop and Report on Oral Health (1999–2000) • NGA Oral Health Policy Academies (2000–2001) Congressional Responses: • GAO Reports, Midlevel trials proposed • Legislation • Hearings (Deamonte Driver) WHO • Alaska ANTHC • Minnesota Legislature, University of Minnesota, Metropolitan State Normandale • Renewed CMS attention/new administration • Prominent foundation involvement: – PEW – Kellogg • HRSA / CA Health Foundation-funded Institute of Medicine (IOM) studies • Public Health Dentists, Small core group • ADEA, interest expressed in the model Access No set definition, clouds the debate • Access: AGD Making Dentistry Available – Patient Education and Responsibility – Affordability – Sufficient Medicaid/insurance coverage to make healthcare affordable for patient – Availability – Incentives/financial support to enable dentists to serve in underserved/rural areas History on Midlevels • In 1917, ‘Dental Dressers’ were established in some counties in England: – The first dental therapists – American hygienist with the addition of ‘filling those cavities without pulpal involvement’ and ‘the extraction of ‘temporary teeth in school clinics’ – Desperate shortage of school service dental officers – First World War – The Dental Act of 1956 there were enough dentists to work in the service and the dresser’s duties were reduced to that of a hygienist History on Midlevels • In 1920, New Zealand established a School Dental Service: – Called Dental Nurses – Were the first contact point for rural patients with an onward referral to a dentist if necessary History on Midlevels • Back to the UK: – In 1950, there was once again a desperate shortage of dentists in the school services – Following visits to New Zealand the Dentist Act of 1956 was changed to allow the training of Dental Auxiliaries – however, Dental Auxiliaries would be referred patients by the Dentist History on Midlevels • In 2002, British Association of Dental Therapists caused the Dental Act to be amended • Dental Therapists were allowed to work in general practice and along with that the SOP finally changed and ‘extended duties’ were added • In every country that has therapists, these associations become a political force and SOP continually expand Added Procedures in England • • • • • • • • • • • • • • Scaling and polishing Apply materials to teeth such as fluoride and fissure sealants Take dental radiographs Provide dental health education on a one to one basis or in a group situation Routine restorations in both deciduous and permanent teeth, on adults and children, from Class 1-V cavity preparations Can use all materials except pre cast or pinned placements Treats adults as well as children Extract deciduous teeth under local infiltration analgesia Pulp therapy treatment of deciduous teeth Placement of pre formed crowns on deciduous teeth Administration of Inferior Dental Nerve Block analgesia Emergency temporary replacement of crowns and fillings Take impressions Treat patients under conscious sedation provided the dentist remains in the surgery throughout the treatment Where Are They? • • • • • • Alaska Australia New Zealand Canada Great Britain Various other smaller projects Alaska DHAT Per the DHAT Website • DHAT: – 10 practicing DHATs trained in NZ – Since 2003, only one has stopped practice in AK – First training center in the US, partnership with UW • MEDEX – 9 graduates, 13 in training – Predict: 32 DHATs in AK by 2012 – PDHA -11 cert (22) – EFDHA -12 cert (23) – DHAH - 0 cert – Role models for younger Alaska DHAT • Alaska DHAT training program information: – First year: 40 weeks – Second year: 39 weeks – Total: 79 weeks (3,160 hours) • Curriculum breakdown, first year: – Biological Science: 30% – Social Science: 10% – Pre-Clinic: 40% (623 hours) – Clinic: 20% (316 hours) • Curriculum breakdown, second year: – Biological Science: 15% – Social Science: 7% – Pre-Clinic: 0% – Clinic: 78% (1,215 hours) • Curriculum breakdown, two years combined: – Biological Science: 22.5% – Social Science: 8.5% – Pre-Clinic: 20% (632 hours) – Clinic: 49% (1,548 hours) Alaska DHAT • After graduation, 400 hours preceptorship • Standards and procedures: –Standing orders –Renewal every two years Australia • Dental therapists have practiced in Victoria since 1975. • Since 2000, movement of dental therapists into new work settings such as private, community, and hospital practices. • Prior to 2000, dental therapists were limited to children attending school. • Now provide up to eighteen years and, upon the prescription of a dentist, from nineteen to twenty-five years. • In orthodontic practices, care prescribed by an orthodontist or dentist may now be provided by dental therapists to clients of all ages. This Year, a New Oversight Group in Australia: National Oral Health Alliance • Did not recommend enhanced Therapists, instead they recommended what the AGD has been saying for 5 years, namely: – Phasing in a dental residency (foundation) year over 5–10 years as policy, infrastructure, professional mentoring, and support develop (initially $20m pa for operations and $60m pa for infrastructure) – Introducing regional, rural, and remote incentives to improve the distribution of the workforce (initially $10m pa) New Zealand • Now, dental therapists train for three years at university or a polytechnic and are registered with the Dental Council of New Zealand • The majority of dental therapists are employed by District Health Boards in schools, though a small numbers work in private practice alongside a dentist • While dental therapists work independently, they will have a professional link to a dentist and refer your child to a dentist when more specialized care is required New Zealand • Treatments that can be carried out by a dental therapist include: – Advice on oral health and cleaning practices for children and adults – Cleaning the teeth – Diagnosis of decay (cavities) in baby (deciduous) or permanent (adult) teeth – this may include using x-rays – Restoration of decayed adult and baby teeth using fillings – Extraction of baby teeth – Preventive therapies to keep teeth healthy – for example using special sealants or topical fluoride – Referrals to other oral health practitioners for assessment and treatment – Keep records of dental treatment New Zealand • Therapists don’t stay long, not cost effective • High career satisfaction but much less satisfied with remuneration • Done in 10 years with dental therapy • Younger DTs were more interested in moving to private practice • A mean of 6.5 years in career Source: Ayers, K.M., et al. The working practices and career satisfaction of dental therapists in New Zealand. Comm Dent Heal 2007; 24:257-63. New Zealand • The dental health of young children continues to be among the worst in the developed world, figures reveal • Forty-four per cent of 5-year-olds have at least one decayed, missing or filled tooth, a school dental services report has found • The Government has spent $417 million on the problem since 2007 but the figures have shown little improvement • In 2000, 48 per cent of 5-year-olds had cavities, and the figure has not dropped below 43 per cent since • New Zealand rates are worse than the UK, US, and Australia Source: Gillis, Abby. NZ children's dental health still among worst. New Zealand Herald, March 2011. Canada • • • • • Large country Many rural, isolated populations Transportation challenges Dentists concentrated in population centers Access to dental care limited Canada • • • • • • • • • • Fillings on primary and permanent teeth Vital pulpotomies on primary teeth Stainless steel crowns on primary teeth Extractions of primary teeth (Prov & Fed) Extractions of permanent teeth (Fed) Sealants Cleanings Fluoride Radiographs Education Canada • Too many dental staff for the amount of dental work that needed to be done • Large provincial deficit, conservative government • Government scrapped the program in 1987, except for the northern program • Expanded dental hygiene schools Dental Team Concept • Prevention, prevention, prevention! • Expanded Auxiliaries within the practice can play key role in prevention • Establishment of Dental Home* • Dental benefits designs to support establishment of dental home from childhood** • Cost savings for patients & carriers! *Advisory Committee on Training in Primary Care Medicine & Dentistry’s (ACTPCMD) 8th Congressional Report (2010) recommends expansion of dental home to medicine as key to prevention and cost-savings **See the American Academy of Pediatric Dentistry’s (AAPD) Policy on Model Dental Benefits for Infants, Children, Adolescents, and Individuals with Special Health Care Needs (2008) Midlevel Providers • Examples: hygienists/dental assistants/expanded function dental assistants (EFDA) within the dental team model, Dental Health Aide Therapist (DHAT)*(AK), Registered Dental Hygienist in Alternative Practice (RDHAP) (CA), Dental Therapist/Advanced Dental Therapist (MN), independent practice of hygienists (CO, ME), Advanced Dental Hygiene Practitioner (ADHP)(Not yet implemented), limited access permits (OR), public health hygiene endorsements (OR, ME), collaborative practice dental hygienists(NM), Level III Hygienist (KS). • Concern: Independent practice w/o direct supervision of a dentist (a.k.a. “Alternative model of oral healthcare delivery”) Midlevel Providers In the Affordable Care Act: • SEC. 5304. ALTERNATIVE DENTAL HEALTH CARE PROVIDERS DEMONSTRATION PROJECT • Subpart X of part D of title III of the Public Health Service Act (42 U.S.C. 256f et seq.) is amended by adding at the end the following: – “SEC. 340G–1. DEMONSTRATION PROGRAM – “(a) IN GENERAL.—”(1) AUTHORIZATION.—The Secretary is authorized to award grants to 15 eligible entities to enable such entities to establish a demonstration program to establish training programs to train, or to employ, alternative dental health care providers in order to increase access to dental health care services in rural and other underserved communities. Midlevel Providers In the Affordable Care Act: • “(2) DEFINITION.—The term ‘alternative dental health care providers’ includes community dental health coordinators, advance practice dental hygienists, independent dental hygienists, supervised dental hygienists, primary care physicians, dental therapists, dental health aides, and any other health professional that the Secretary determines appropriate. Alternative Models • Advanced Dental Hygiene Practitioner (ADHP) • Community Dental Health Coordinator (CDHC) • Dental Therapist (DHAT and numerous variations) ADHP • Created by ADHA • Completion of hygiene program + 2 years of Master’s study • Diagnose and treat, including restorations and extractions • General or No Supervision • Pilot Study in CO indicated hygienists failed to practice in underserved areas • Not implemented in any state New Data, Implications of New Legislature • Possible funding for the ALTERNATIVE DENTAL HEALTHCARE PROVIDERS DEMONSTRATION PROJECT • Expansion of National Health Service Corps to specifically include dental therapists • Create demonstration programs for training and employment of alternative dental health care providers, including within the Departments of Defense and Veteran Affairs, Federal Bureau of Prisons and Indian Health Service • Amend Medicaid reimbursement criteria to include services provided by alternative dental providers. CDHC • • • • Created by ADA 18 Months of training Community, public health, and private practice settings Provides education/case worker services under general supervision • Limited treatment with door open for modification of SOP • New Mexico to implement Dental Therapists • • • • • • • Favored by Pew and W.K. Kellogg Modeled after New Zealand, Great Britain, Canada Two years or so of education Diagnosis, restorations & extractions General supervision Implemented in AK (native) & MN Benchmark for Proponents - Minnesota Minnesota Model • Dental Therapist (DT): – Both indirect and general supervision – Only 26 to 28 months of training – 16 licensed so far • Advanced Dental Therapist (ADT): – 2,000 hours – Prerequisite DT license – General Supervision • Practice Settings: – Both DT and ADT are limited to primarily practicing (about 50%) in settings that serve low-income, uninsured, and underserved patients or in a dental health professional shortage area. Other States • W. K. Kellogg targeting 5 states for dental therapist pilot programs: KS, NM, OH, VT, and WA • Washington: – Eastern Washington Univ. – ADHP Masters Program – HB 1310 (Advanced Dental Therapist) Bill withdrawn (2011) • Kansas: – HB 2280 (Registered Dental Practitioner) defeated (2011) – Does now have new Level III Hygienist States with Mid-Level Provider Legislation Legend: Pending Enacted Failed Nash Review of 1,100 Reports • Released by W.K. Kellogg Foundation, April 2010 • Claims that dental therapists can provide “technically competent, safe and effective” care • Fails to measure true patient health outcomes • More of position paper than a clinical research report (as noted by title, A Review of the Global Literature on Dental Therapists: In the Context of the Movement to Add Dental Therapists to the Oral Health Workforce in the United States) ADA Systematic Review • Sought to find the science to back up claims • 7,700 articles reviewed • Only 18 possibly useable, of which 12 were high bias, 5 were medium bias, and only 1 was low bias • Found no improvement in the oral health of the community by adding therapists • Quality of data was poor and refutes the foundations claims of hundreds of articles California Study • SB694 – A bill to study use of midlevel providers in CA • No dentist shortage in CA • Bill died in appropriations • The sponsor has called for a special session of the legislature to discuss the bill – will take place in Dec. ‘12 Jackson Brown Articles • The Economic Aspects of Unsupervised Private Hygiene Practice and Its Impact on Access to Care (2005) • www.ada.org/sections/professionalResources/pdfs/report_hygiene.pdf • “Unsupervised private dental hygiene practice has not had a notable effect on access to care in Colorado” • “They are located in areas served also by dental offices with traditional dental hygienists” • “The economic viability of the unsupervised hygienist business model is questionable because their prophylaxis fees, on average, are not different from traditional dental practices, which have the advantage of providing a full range of practice services” Study of Alternate Dental Providers, Five State Comparison • Five states, three models, three payment systems • Only in a couple of scenarios would using therapist be minimally economically sustainable – they would have to be heavily subsidized • “The current public payor and indigent reimbursement levels is not economically feasible for providers with salaries at 50% of the Dentists” • “The limitations to greater access to dental care is that existing fee schedules do not cover the cost of treating the patients” • The addition of additional providers does nothing to address this issue AAPD Answers Kellogg • In addition to AGD and the ADA, the AAPD also responded to the Nash/Kellogg Report • Key points of AAPD: – Report fails to account for variations between 54 countries – Based on opinions, not data – Fails to address economic viability – Technical competence ≠ long-term patient outcomes The Perth Meeting • The Presidents of the American Dental Association, the British Dental Association, the Australian Dental Association, the Canadian Dental Association, and the New Zealand Dental Association had a discussion on the success or failure of the therapist programs • In ALL of the countries utilizing therapists, there was no improvement in Access and NO cost savings ADEA and Public Health • They claim that this workforce issue is being driven by: – Access to care – Oral health disparities – Some believe that the DT could be an answer to these problems Dental Extenders at CHC’s • WSDA introduces legislation to introduce AFDAs (Advanced Function Dental Auxiliaries) for community health centers approved by the Dental Quality Assurance Commission (DQAC) • Essentially, public health EFDA with added surgical privileges under direct supervision Prevention-Focused Care • A fully trained dentist and a full oral health team (dental team concept), CDA, EFDA, RDH • The dentist utilizes the team to increase efficiency in order to treat more patients but without decreasing the level of care • Just adding more hole fillers doesn’t increase the level of overall oral health Prevention-Focused Care From: Vibeke Bælum Date: October 23, 2012 Subject: Re: Dental therapists in Denmark No, fortunately, we don't have dental therapists here, just dentists and dental hygienists. We don't need more professionals that are licensed to drill and fill. The high speed drill was never instrumental for oral disease control. Best regards, Vibeke Prevention-Focused Care • “Oral Health Inequities will only be reduced through the implementation of effective and appropriate oral health promotion policy.” – The State of Oral Health in Europe, Dr. Rena Patel, September 2012 • 40 years ago, Denmark embarked upon oral health improvement, and by the end of the 1990’s, they have 99% of the children with consistent preventative services and a high national level of Oral Health Literacy Number of Dentists – NOT the Issue • 1:2,000 • Health Resources and Services Administration (HRSA) standard is 1:5,000 or lower in many locations • Advancements in technology and increases in the education and number of auxiliaries within the dental team show that capacity is the key, not ratios! 2,263 2,246 2,500 134,492 136,717 2,256 2,260 2,274 2,248 2,249 2,274 2,261 2,273 2,257 2,239 2,267 160,000 2,254 Number of Active Private Practicing General Practitioners, 1996–2009 2,000 1,500 80,000 1,000 60,000 Population to GP Ratio 133,688 132,118 130,054 130,335 129,096 126,546 126,097 124,151 123,625 123,197 100,000 119,493 Number of GPs 120,000 120,250 140,000 40,000 500 20,000 Number of GPs 2009 2008 2007 2006 2005 2004 2003 2002 2001 2000 1999 1998 1997 0 1996 0 Population/GP Source: Distribution of Dentists in the United States by Region and State, various years, 1996 to 2009; and U.S. Census Bureau. CAPACITY, Survey March 2011 CAPACITY, Survey March 2011 • Of the 589 members who were seeing fewer patients than two years ago, 47.5 percent indicated that they are seeing between 11 and 25 percent fewer patients; 36.3 percent are seeing 10 percent or less fewer patients; and 10.9 percent indicated that they are seeing between 26 and 50 percent less patients • Of the 328 members who were seeing more patients than two years ago, 45 percent indicated that they are seeing between 11 and 25 percent more patients; 27.7 percent are seeing 10 percent or less more patients; and 13.4 percent indicated that they are seeing between 26 and 50 percent less patients • The Dental Economics Advisory Group states that, with the new dental schools coming on line and the anticipated workforce and technology enhancements, the supply of dentists is not likely to be a problem • “Capacity Utilization” problem: In Economics this means, “Don’t create more until you use what you already have” • PEW's “shortage of dentists” based their assumption on the numbers who are willing to treat low-market or non-market patients • PEW refuses to understand that, “regardless of how many DHATs they produce, they still can't address the dental needs of the underserved dealing with social and cultural issues, transportation and health literacy.” Dr. Ron Tankersley, ADA Past President • The Foundations and others don't seem to want to work on the major aspects of the issue • In a report to the National Oral Health Conference, a state with 62% dentist involvement in Medicaid in a 5-year CDC assessment done by DOH using ASTDD standards on 5,732 children in 73 schools in 2008 showed: In the Untreated Caries Summary: • The children in the Medicaid group showed “NO DIFFERENCE” than any other category • Their data was the same as insured patients In the Treatment Urgency Summary: • The children in the Medicaid group showed “NO DIFFERENCE” than any other category • Their data was the same as insured patients • Some claim that Medicaid reimbursements don’t affect participation, but a statewide school nurse survey showed the opposite trend • Increases in Medicaid rates had a direct correlation to the numbers of dentists • However, Parent Involvement and Transportation were the biggest barriers, not dentists’ involvement Fiscal Pressure on Medicaid Programs Breakdown of Total Medicaid Spending, 2010 • “CMS sees Medicaid costs outpace projections.” • “Medicaid spending will increase 7.9% per year over the next 10 years. That compares to a growth rate of 4.8% in the general economy.” 1.8% • “We must act quickly to keep state Medicaid programs fiscally sound.” Source: CMS and HHS • “20 states cut Medicaid payment rates last year. At least 16 governors have proposed rate reductions this year.” 98.2% Source: Kaiser Family Foundation Oral Health Services All Other • Oral health is affected by more factors than access to dental care • Because so many factors at the individual, environmental, and delivery system levels affect oral health, interpreting the findings from international studies is difficult Source: Community Dentistry and Oral Epidemiology, 2006 • “Direct public expenditures constitute only 6% of total spending for dental care in the US, just three-eighths of the proportion in Australia, and almost all of it is limited to the care of children • New Zealand’s program in the schools has been in place a long time and, thus, it may be surprising to learn that Baltimore adolescents had (among all countries in ICS I and ICS II) the lowest number of DMF teeth and the second- or third-lowest number of decayed teeth” Source: Chen MS, Andersen RM, Barmes DE, Leclercq MH, Lyttle CS. Comparing oral health systems: a second international collaborative study. • “Financial barriers to access are significant in explaining how much desired dental care is actually received in the US” Source: Mueller CD, Schur CL, Paramore LC. Access to Dental Care in the United States. • Workforce is but a very small part of oral health improvement • “The New Zealand oral health therapist program is touted as the model for this country’s foray into a mid-level provider. In 2004, the DHBNZ (Ministry of Health) declared the School Dental Service to be “in strategic crisis” and that inequities continue to exist, notably with low income, minorities, and rural populations. They further concluded that facilities were run down, not suited to modern practice and non-compliant with health and safety standards.” Source: Dr. Crall, AAPD presentation. • The AAPD suggests the burden of proof from studying such models is to first show they actually work, versus trying to implement nationwide programs based on “what harm can they do? / something is better than nothing” • “Something” that drains away resources and provides less comprehensive care for children could in fact be worse than doing nothing” Source: Dr. Crall, AAPD presentation. New Strategy • The goal is Improved Oral Health – Access is only a small part of Oral Health – Workforce is only a small part of Access • The REAL BARRIERS are Oral Health Literacy, Economic, Transportation, Cultural, and Social Issues • Don’t fight over what will not help Oral Health anyway Get Involved US Representative Jeff Duncan THANK YOU!