Chapter 20: The Cardiovascular System: Blood Vessels
advertisement

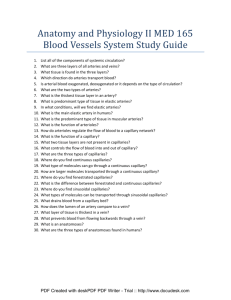
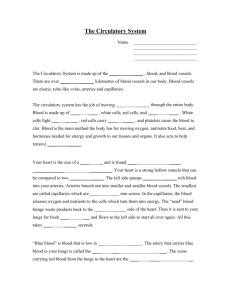
Chapter 21: The Cardiovascular System: Blood Vessels Heart arteries arterioles capillaries venules veins heart Blood Vessel Anatomy Arterial Blood System ______________ vessels- “air,” “to carry” Types: Elastic = conducting muscular = distributing Venous Blood System _________________ vessels Capillaries - ______________ vessels Arteries- 3 tunics figure 21.1 ____________________- lining of simple squamous epithelium = 1. ____________, closest to the lumen 2. Basement membrane 3. Internal elastic lamina ________________- middle coat, usually thickest, elastic & circular smooth muscle __________________- stretch without tearing Innervated by sym NS for constriction/dilation _____________________- outer, elastic & collagen Vaso vasorum “_______________________” Larger blood vessels require oxygen and nutrients, to do so they are served by these types of blood vessels Types of arteries ________________–largest diameter __________________ in tunica media Walls ___________ compared to diameter Help ______ blood while ventricles relax Walls stretch to store ______________ Conduct blood to more muscular arteries Aorta, brachoiocephalic, common coratid, subclavian, vertebral, pulmonary, common iliac Types of arteries (2) _____________________- distribute to various parts of the body Media- more smooth muscle, less elastic Capable of > vasoconstriction/dilation Examples: brachial artery, radial artery Arterioles Small artery 10-100 μm in diameter ________________________ Similar to arteries but usually just a ring of endothelial cells surrounded by scattered smooth muscle fibers ______________ – opposition to blood flow Mainly friction between blood an inner walls Arterioles can be dilated or constricted called resistance vessels _________________ can affect bp Capillaries = microcirculation Microscopic vessels, 4-10μm connect arterioles to venules Near almost every cell in the body # vary w/metabolic activity of the tissue _______________ – exchange of nutrients and waste between blood and tissue cells thru interstitial fluid Walls= single cell layer thick & b.m. ________________– emerges from arteriole & supplies 10-100 capillaries (capillary bed) Capillaries (2) __________________ – ring of smooth muscle at the junction of the arteriole with metarteriole Control flow to capillary bed __________________- bypasses the capillary bed Types of capillaries, fig. 21.4 _______________ – endothelial cells form continuous tube only interrupted by intercellular clefts (gaps) Skeletal & smooth muscle, CT, lungs __________ – “window,” have small pores Kidneys, villi, choroid plexuses, endocrine glands ____________ – wider than other cap, may have unusually large fenestrations Incomplete or absent basement membrane Liver, red bone marrow, spleen, some endocrine Venule ______________________ forming these small veins Walls very porous Many phagocytic WBC migrate from here Few scattered smooth muscle cells Larger venules more ____________ _______________________ Veins 3 layers, interna & media much thinner than artery (less smooth muscle & elastic) thickest layer - tunica externa = collagen & elastic fibers, lack external & internal elastic lamina __________ to handle volume & pressure Δ yet not capable to withstand pressure have abundant __________ (esp. in limbs) thin folds in the tunica interna form flaplike cusps projecting into the lumen towards the _________________________ Capillary exchange, fig 21.7 7% blood in systemic cap at any one time Diffusion _______________- plasma in vesicles are endocytosed by endothelial cells & exocytosed out other side Insulin, Ab from mother to fetus ________________- passive process, large # of ions, molecules particles move in same direction at rates > than w/diffusion Filtration & resorption Pressure driven movements ________– fluid & solutes interstitial fluid ___________– FROM interstitial fluid blood capillaries 2 pressures accountable for filtration: Blood hydrostatic pressure (BHP)- generated by pump action of heart Interstitial fluid osmotic pressure Main pressure accountable for reabsorption: Blood colloid osmotic pressure (BCOP) _____________________ (NFP) = balance of all of these pressures Pressure driven movements (2) __________________ – pressure due to water in plasma exerted against bv Interstitial fluid hydrostatic pressure pushes fluid back into capillaries Is close to zero Difference in ________________ across due to plasma proteins too large to pass pores or fenestrations BCOP force of these large proteins to pull IF into capillaries (remember- diffusion from to ) Edema __________________________________ Interstitial fluid 30% > than normal Causes of excess filtration: capillary blood pressure permeability of capillaries Chemicals, bacterial, thermal, mechanical Cause of inadequate reabsorption: concentration of plasma proteins Liver disease, burns, malnutrition, kidney disease Blood pressure Hydrostatic pressure exerted by blood on walls of blood vessel __________________________________ __________________________________ @ 110mmHg during systole drops to70mmHg during diastole Systolic- highest pressure in arteries during systole Diastolic- lowest arterial pressure during diastole Pressure falls progressively as distant from L.V. Mean arterial pressure MAP = average bp in arteries @1/3 between systolic & diastolic MAP = diastolic bp +1/3(systolic-dia) CO MAP blood volume MAP *Don’t forget, just as in the ventricles, blood flows from areas of high to low pressure Resistance = opposition to flow BF = DP/R BP = CO x TPR (TPR=total peripheral resistance= all the vascular R offered by systemic bv) Viscosity- thickness, viscosity resistance, flow vessel length- longer vessel, resistance vessel diameter (1/ r4)- lumen resistance Blood volume- volume pressure CO = SV x HR If CO, P as long as R is same Systemic Vascular Resistance (SVR) and venous return Arterioles control SVR bp & blood flow to particular areas by Δ diameter Controlled by brainstem ____________________: Besides heart 2 mechanisms to pump blood: _________________: valves open, muscle contraction pushes blood thru proximal valve and closes distal, muscle relax & close proximal _________________: pressure in thoracic pressure in abdominal volume from abdomen to Rt Atrium Regulation of Blood pressure CV center – input from higher brain regions & sensory receptors Figure 21.12 Neural Baroreceptors – Δ pressure Carotid sinus- for pressure in the brain Aortic- regulate systemic pressure Chemoreceptors – Δ O2, CO2, H + acidosis symp hormones, vasoconstriction Hormonal control Renal regulation, symp hormones, ANP, Angiotensin II Hormonal regulation of bp _______________________ (RAA)- blood volume falls or kidney blood flow, renin angiontensin II bp Vasoconstriction Stimulates release of aldosterone ______________- CO by HR and force, also cause vasoconstriction _______- released due to blood volume urine output, vasoconstriction __________________________- released by , bp by vasodilation Circulatory shock Failure to deliver O2 and nutrients to meet metabolic need Hypovolemic – low blood volume Cardiogenic – poor heart function Vascular – inappropriate vasodilation Obstructive- obstruction to blood flow See figure 21.16 – responses Activation of RAA ADH Sympathetic hormones Local vasodilators: K+, H+, lactic acid, NO Shock: signs and symptoms Systolic bp 90 Resting HR due to symp Pulse weak and rapid, CO & HR Skin is cool, pale, clammy Mental state altered urine production thirst pH due to acidosis Nausea - impaired blood flow to GI tract Disorders _________________- a group of diseases characterized by thickening of artery walls and loss of elasticity _____________- thin weakened section of the wall of artery or vein, bulges out Graft or replace _______- inflammation of vein, often in leg CVA= cerebrovascular accident- destruction of brain tissue (infarction) resulting of obstruction or rupture of bv supplying brain Atherosclerosis, LDL, and HDL Atherosclerosis - a stage of arteriosclerosis involving fatty deposits or plaques (atheromas) inside the arterial walls, thus narrowing the arteries Plaques develop from due to excessive LDL (containing much cholesterol) accumulate in the inner layer of the artery wall HDLs decrease amount of excessive cholesterol, transport it to liver for elimination Hypertension Silent killer- damage to bv, heart, brain, kidney before any noticable pain or symptoms Major risk factor for both#1 cause of death = heart disease, & #3 = stroke Lifestyle changes: lose weight, exercise, reduce salt intake, maintain proper electrolyte intake, don’t smoke, manage stress Drug treatment ACE (angiotensin converting enzyme) inhibitors beta blockers- inhibit renin Vasodilators Ca 2+ channel blockers- decrease heart rate Fetal circulation O2 & nutrients- diffusion from maternal blood (& eliminates its CO2 & wastes) exchange occurs ______________-inside uterus Normally, no direct mixing of maternal & fetal blood; all exchanges by diffusion thru capillaries Deoxy blood from fetus to placenta via 2 umbilical arteries -____________________ ___________________________________ Fetal circulation (2) Umbilical vein ascends to liver, forms 2 branches: some thru the branch that joins the hepatic portal vein most flows into ____________ IVC Deoxygenated blood IVC mingles w/blood from ductus venosus Deoxy blood from upper body SVC, this blood mixes in the right atrium Fetal circulation (3) Most blood does not pass to rt ventricle & lungs but thru _________opening between right & left atria, bypassing pulmonary circuit Blood reaches rt ventricle, but little reaches nonfunctioning lungs Instead, most blood sent thru another bypass _____________-vessel connecting pulmonary trunk & aorta (becomes ____________________)