semen analysis

SEMEN ANALYSIS:
What? When? How? Why?
Dr Sharon Mortimer, PhD
Director, Oozoa Biomedical Inc
Research Planning & Development Specialist,
Faculty of Medicine, UBC
Editor, “Reproduction, Fertility and Development”
BACKGROUND
What is semen, exactly?
A mixture of seminal plasma and cells
•
Seminal plasma contains:
–
Prostatic fluid (~30% of the volume)
– Epididymal plasma (~5% of the volume)
– Seminal vesicle fluid (the remainder of the ejaculate)
•
The cells are:
– Spermatozoa
–
Germ line cells
– Leukocytes of various types
– Bacteria
– Epithelial cells
– Occasional red cells
© Oozoa Biomedical Inc, April 2005
BACKGROUND
Formation of the sperm cell (1)
•
Formed in the seminiferous tubules, develop in close association with the
Sertoli cells
• Start as spermatogonia (self-renewing stem cell of the male germ cell line) – located on the basement membrane
•
The transformation from the round germ cell to the sperm cell occurs during passage to the centre of the seminiferous tubule
© Oozoa Biomedical Inc, April 2005
BACKGROUND
Formation of the sperm cell (2)
• Spermatogenesis is a cascade of cell divisions:
–
Mitosis: spermatogonia to primary spermatocytes
–
First meiotic division: secondary spermatocytes
–
Second meiotic division: haploid spermatids
• This process takes 70 ± 4 days in the human – so errors will take about 3 months to show up
© Oozoa Biomedical Inc, April 2005
BACKGROUND
Formation of the sperm cell (3)
• Spermiogenesis: differentiation of the round spermatid into a spermatozoon
•
This is the process in which sperm morphology is largely determined
© Oozoa Biomedical Inc, April 2005
BACKGROUND
Sperm transport and seminal plasma
• “Testicular sperm” need to undergo more maturation steps before they are ready to fertilize
• Transported from the testes to the epididymis, where they mature, and acquire the ability to swim
• Then moved to the vas deferens, for storage
• At ejaculation, the sperm are transported out of the vas and mix with accessory gland secretions:
– prostatic fluid (pH slightly acidic to neutral; contains citric acid and zinc)
– seminal vesicle fluid (pH strongly alkaline; contains fructose)
© Oozoa Biomedical Inc, April 2005
BACKGROUND
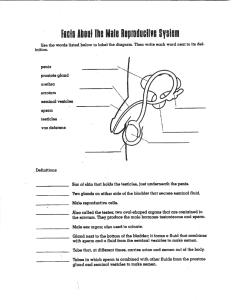
What the spermatozoon looks like (1)
• Not the homunculus (left)
•
More like the rabbit sperm
(right) – drawn by Antoni van
Leeuwenhoek in 1679
© Oozoa Biomedical Inc, April 2005
BACKGROUND
What the spermatozoon looks like (2)
Midpiece
Head
Tail
• The human sperm cell is about 70 µm long
•
The nucleus is in the head – contains the 23 chromosomes
• It is the head which binds to the egg at fertilization
• Midpiece: the energy for motility is generated
• Tail: motility – the beat is initiated just behind the midpiece, and then propagated along the tail
© Oozoa Biomedical Inc, April 2005
BACKGROUND
What the spermatozoon looks like (3)
outer dense fibres central pair dynein arms
B subunit microtubule doublet
A subunit
•
Tail cross-section
• The dynein arms from one doublet reach forward and touch the next doublet, ratchet forward, and then let go
• Then the next doublet’s arms reach forward, etc.
• This generates the tail wave, and hence sperm motility
© Oozoa Biomedical Inc, April 2005
BACKGROUND
Sperm function
•
The ejaculated sperm pass through the cervix, then the uterus, and enter the oviduct
•
The fertilizing sperm swims through the layers of cells around the egg (cumulus and corona), and reaches the zona pellucida
• The sperm then loses the front membranes of its head (the
“acrosome reaction”), binds to the zona, then forces its way through the zona to the egg membrane
• When the sperm head binds to the egg membrane, its tail stops beating, and the egg incorporates the whole sperm cell
• The egg unpacks the sperm, then the male and female pronuclei form.
© Oozoa Biomedical Inc, April 2005
WHAT IS A SEMEN ANALYSIS?
•
An evaluation of spermatogenesis and spermiogenesis.
• Traditional descriptive analysis:
• interpretation based on population distributions of characteristics,
• therefore prone to misinterpretation at the individual level.
• Modern approach is to interpret with regard to:
• diagnosis of specific lesions; and
• indicators of dysfunctional and/or functional potential.
• Requires understanding of the relevance of sperm patho-physiology.
• In any case, the results must be accurate and reliable.
© Oozoa Biomedical Inc, April 2005
WHY PERFORM SEMEN ANALYSIS?
•
Diagnosis of sterility
• Diagnosis of infertility
• Prognosis for fertility
• Identify treatment options:
• surgical treatment
• medical treatment
• assisted conception treatment
Therefore = a screening test to help direct management.
© Oozoa Biomedical Inc, April 2005
What is the “standard” approach to semen evaluation?
International minimum standards are, by consensus, the
World Health Organization’s Lab Manual.
•
Focus is on standardization with expanded section on quality control.
•
Methods amenable for use in any
(“third world”) country.
•
Basic infertility work-up.
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sample Collection
For a meaningful result, semen samples must always be collected under standardized conditions:
– the container has to be sterile and known NOT to be spermotoxic (i.e. provided by the lab)
– the man must have had 3 – 5 days of abstinence
– the man must have washed his hands before collection
(particularly if microbiological analysis is requested)
– the man must NOT have used lubricants (except for
Pre~Seed or His~Seed, the only “sperm-friendly” ones)
– the sample must be kept at 37°C until analysis, which begins ideally within 30 min, but absolutely within 60 min, of ejaculation
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sample Handling
• The semen sample should be mixed gently during the liquefaction period to promote liquefaction
•
The sample should NEVER be vortexed (the only exception is for the fixed prep for concentration assessment)
•
The sample should NEVER be “needled” – if it is too viscous to work with, a known volume of sperm buffer (not PBS) should be added and the sample mixed gently. The added volume must be included in the sperm concentration calculation
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Macroscopic Evaluation
•
There are several macroscopic evaluations which give useful diagnostic information about the sample:
– Appearance
– Odour
–
Liquefaction
–
Volume
– Viscosity
– pH
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Macroscopic Evaluation - Appearance
•
Swirl the sample, still in the collection jar, gently
•
Hold the jar up to look through its bottom
•
Note the following:
–
Colour (normal = white to grayish-yellow) – if there is blood present, it may range from pink to brown
–
Opacity / translucence (normal = tends to opaque)
– Whether mucus streaks or cell clumps are present
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Macroscopic Evaluation - Odour
•
Different people have different abilities to smell semen, so this cannot be standardized
•
However, when the lid is taken off the collection jar, it should be noted if there is a strong smell of urine or of putrefaction
•
Samples collected after a prolonged abstinence period
(i.e. several weeks) are likely to have a stronger odour
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Macroscopic Evaluation – Liquefaction & Viscosity
• Liquefaction is the breakdown of the gel portion of the seminal plasma – the enzymes for this are in the prostatic fluid
–
A sample with incomplete liquefaction has a gelatinous material in a liquid base – this can be seen when the sample is swirled for the appearance assessment
• Viscosity is related to the fluid nature of the whole sample
– This is rated subjectively according to the length of the thread of semen produced when the sample is allowed to run back out of the volumetric pipette used to measure the ejaculate volume
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Macroscopic Evaluation - Volume
•
The volume of the sample should be measured to allow an accurate determination of the sperm number
•
This is most easily assessed using a warmed disposable volumetric pipette (which is sterile and known NOT to be spermotoxic)
•
After the sample is measured, allow it to run back into the collection jar, noting its viscosity (a normal sample will have some viscosity – i.e. not watery, but it will flow easily)
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Macroscopic Evaluation - pH
• pH is important because sperm die at pH < 6.9
•
The pH of liquefied semen is normally determined using test strips (we use EM Science ColorpHast type, pH 6.5–10.0)
•
We usually measure pH after volume and viscosity – by touching the “emptied” volumetric pipette to the test strip
•
The normal pH range is 7.2–8.4
•
Inflammatory disorders of the accessory glands can take the pH outside of this range
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
The wet preparation – set-up
•
Place 10µl of thoroughly mixed, liquefied semen on a microscope slide and cover with a 22x22mm No 1½ coverslip
• There are several important points to keep in mind:
–
The quality of sperm motility is affected by temperature – the lower the temperature, the poorer the motility, and then cold shock starts to occur at around 15°C.
So great care must be taken to ensure that the slides and coverslips, as well as the pipette tips are kept at 37°C
–
The assessment must start as soon as the flow stops – if this is
>1 minute, then a new wet prep must be made
–
Microscope: phase contrast optics and a heated stage
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
The wet preparation – assessments
•
The characteristics assessed are:
–
Motility (to be discussed later)
–
Sperm aggregation (random clumping) – “some” is normal, but large clumps (each with hundreds of sperm) is abnormal
–
Spermagglutination (between specific sites) – could suggest the presence of antisperm antibodies.
–
Round cells: should be <1 per 40× field (~ 1 million/ml). If more abundant, a leukocyte test should be run
–
Epithelial cells: usually present in small numbers
–
Erythrocytes: should not be present
–
Debris: particles smaller than sperm head, may be plentiful
–
Bacteria and protozoa: presence indicates infection
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Motility assessment - Background
• This is the first assessment made on the wet prep
• If >10–15% of the sperm are clumped, just assess the freeswimming sperm (and note this on the report form)
• A repeat assessment should be made on a second wet prep
• Don’t estimate, count (> 4 fields and 200 sperm per prep)
• Use a 40× objective, and phase contrast optics
• Make a random selection of the fields that are assessed
•
Assess fields that are away from the coverslip edge
•
Count only those sperm that were in the field at one moment in time (you have to be quick!)
• There must be agreement to within 10% between duplicates
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Motility assessment - types
• % motile = the proportion of sperm with tail movement
•
Progression rating = the grade of progression shown by the majority of the sperm: this can be from 0 (all immotile) to 4
(all with rapid progression); or from a (rapid progression) to
d (all immotile)
• Differential motility count = proportion of sperm in each of
4 motility classes (rapid progressive; slow progressive; nonprogressive; immotile)
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Motility assessment – differential motility
•
Differential motility classification is based on the distance swum over time:
–
Rapid progressive: > 25 µm/s
–
Slow progressive: 5 – 25 µm/s
–
Non-progressive: < 5 µm/s
–
Immotile: no flagellar movement
• The sperm head is about 5 µm long, so the rapid sperm have a net gain of 5 head lengths / second
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Motility assessment – monitor
• Alternatively, we use a video monitor with a grid for the differential motility assessments
– so we do them off the screen.
• Each square is the equivalent of
25 × 25 µm (a stage micro-meter is used to set this up)
• This approach is very useful for training and for QC/QA
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Motility assessment – lab sources of error
• Have the definitions been implemented correctly?
•
Are staff trained to classify progression?
•
Internal quality control?
• How is velocity/progression assessed?
• Effect of temperature :% motile = minimal
% progressive = slight
% rapid = very large
• Representative sample aliquots?
• Adequate number of sperm counted?
•
Repeatability of duplicate counts?
• Calculations performed correctly?
• Precision of results?
• External quality assurance / proficiency testing?
• Uncertainty of results?
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Motility assessment – interpretation
• The WHO’s Reference values for motility are:
–
50% or more with progressive motility; or
–
25% or more with rapid progressive motility
•
Assuming that all of the collection and laboratory factors have been controlled, a poor motility result may have negative implications for fertility.
• However, this should be confirmed by a repeat semen analysis, and the result should be interpreted with the rest of the semen analysis results
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm concentration- background
•
Sperm count = total number of sperm in the ejaculate
• Sperm concentration = number of sperm per ml
(not “density”, which is an expression of mass / unit volume)
• Most accurate method is volumetric dilution and haemocytometry
• Must use a positive displacement pipettor
•
We make a 1 + 19 dilution with a fixative solution (allows the assessments to be batched - usually counted within two days)
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm concentration - method
•
Fix the haemocytometer coverslip over the chambers – ensure interference fringes can be seen
•
Vortex the fixed sample, load ~10
µl in both chambers
• Leave in a humid chamber for
10-15 minutes
• Count using a 20× objective and phase contrast optics
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm concentration - haemocytometer
First large square counted
The number of squares assessed depends on the number of sperm counted in the first large square:
–
If < 10 counted, the whole grid is assessed
–
If 10-40 counted, 10 squares are assessed
– If > 40 counted, 5 squares are assessed
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm concentration - calculations
•
If the counts of the two chambers are not within 5% of their average (i.e. the difference > 1/20 of their sum): discard, remix the sample, and set it up again
• If the two counts are in agreement, then the sum of the two counts is divided by the correction factor:
–
If 2 × 25 squares counted, divide their sum by 10
– If 2 × 10 squares counter, divide their sum by 4
–
If 2 × 5 squares counted, divide their sum by 2
• This gives the sperm concentration in millions per ml
• Sperm count = concentration × total volume
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm concentration – lab sources of error
•
Sample aliquot representative of ejaculate?
– semen homogeneous (mixed)?
– accurate sample aliquot (N.B. viscosity)?
– duplicate aliquot?
•
Accurate dilution : – volumes of sample aliquot and diluent?
– storage (airtight) / sperm bind to vial?
•
Secondary sampling : – mixing of diluted aliquot?
– duplicate aliquots?
•
Preparation of counting chambers : – good chamber design/manufacture?
– chamber loaded correctly &/or cover glass placed correctly?
– adequate minimum number of cells?
– repeatability of duplicate counts?
•
Calculations correct?
•
Precision of results?
•
Uncertainty of measurement known?
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm concentration – interpretation
•
The WHO Reference values for:
–
Sperm concentration is > 20 × 10 6 sperm/ml
– Sperm count is > 40 × 10 6 sperm per ejaculate
• A persistently low sperm concentration is associated with impaired fertility
•
If a man has a sperm concentration < 5 × 10 6 sperm/ml, the
WHO recommends assessment for numerical and structural abnormalities of sex chromosomes
• Azoospermia can indicate a failure of spermatogenesis or blockage(s) in the male tract
© Oozoa Biomedical Inc, April 2005
FALLING SPERM COUNTS
SECULAR TREND IN SPERM COUNTS
150
100
50
0
1930 1940 1950 1960 1970 1980 1990
Carlsen et al.: Br. Med. J., 305:609-613, 1992
© Oozoa Biomedical Inc, April 2005
Falling sperm counts: Apocalypse now?
ANDROLOGY SPECIAL INTEREST
GROUP OF ESHRE (1997)
Pre-Congress “Controversies” Course
“Yes”
=
“No”
=
Richard Sharpe
David Mortimer
The motion was lost – not because of any lack of evidence for adverse effects on male reproductive potential, but because the data on sperm counts was established as too unreliable for valid meta-analyses.
© Oozoa Biomedical Inc, April 2005
Variation in Sperm Counting
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm morphology – background
•
Morphology is even more important than motility and concentration
•
Because of the small size of the human sperm head, must use an air-dried smear which has been stained
•
The Papanicolaou method is best
•
Prepared samples are assessed using a 100× oil-immersion objective under bright field optics
•
The WHO recommends that 200 spermatozoa are counted per sample (and says that 2 × 200 is better)
•
Fields for counting must be selected at random
•
When counting, remember about the normal distribution
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm morphology – morphology types
Variations of normal head shape Asymmetric insertion
Non-inserted tail
Distended midpiece
Thin midpiece
Small / large head Tapering heads
Cytoplasmic droplet
Coiled tail
Duplicate tail
Conjoined form
Pyriform heads Vacuolated head
Constricted Reduced acrosome
Amorphous forms
Dense staining
Short tail
Hairpin tail
Terminal droplet
Bent tail
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm morphology – assessment
• Even “good” samples will have <20% normal forms
• But we know that these sperm from these samples can fertilize eggs – so is the morphology any help at all?
•
Yes it is – but there are a few things to think about:
–
The result will indicate a probability, not an absolute
–
You have to count 2000 sperm to discriminate reliably between, say, 3% and 5% (“Strict Criteria” cut-off 4%)
–
The dynamic range of 4 – 15% is not very large, and means that it is difficult to make a meaningful assessment
• So we use an extra “index” for morphology assessment
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm morphology – assessment schemes
vs
• Tygerberg scheme defines normal sperm and counts the number that meet these criteria.
• WHO’92 looks for, and counts, defects that might affect sperm function in each region of a sperm – normal sperm are those that have no recognizable defects.
• Expert direct comparison study between the schemes* revealed little difference.
• Issues with counting error and uncertainty of measurement, especially if only 100 sperm counted.
• Need additional information, e.g. Acrosome Index or Teratozoospermia Index (TZI) when dynamic range of % normal forms is very limited.
* Mortimer & Menkveld (2001) J. Androl. 22:192-205.
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm morphology – TZI
• The Teratozoospermic Index is an expression of the average number of abnormalities per abnormal sperm
•
Each sperm cell is assessed for an abnormality in the head, neck/midpiece, or tail, and for a cytoplasmic droplet
• If it does not have any of these abnormalities, it is “normal”
• If it does have an abnormality, it is “abnormal”, and we score each abnormality. So, if a cell has an abnormal head and tail, it is counted as 1 cell, and 2 abnormalities
• Then, (total # abnormalities) / (total # sperm) = TZI
•
A TZI > 1.80 has been associated with poor sperm fertilizing ability in vivo and in vitro
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Semen biochemistry
• Acid phosphatase: marker for prostatic function
• Citric acid: can indicate prostatic function – low levels may indicate dysfunction or a prostatic duct obstruction
•
Zinc: marker for prostatic function – colorimetric assay
(WHO)
•
Fructose: marker for seminal vesicle function, and is a substrate for sperm metabolism – spectrophotometric assay
(WHO)
•
-Glucosidase: secreted exclusively by the epididymis and so is a marker for epididymal function – spectrophotometric assay (WHO)
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Sperm Vitality
• Used in samples with low total motility (<50%)
• Distinguishes between samples with live, but immotile sperm
(e.g Kartagener syndrome), and those with lots of dead sperm (could result from: sperm senescence; exposure to detergents or lubricants; or spermotoxic antibodies)
•
Also provides a check on the accuracy of motility assessments: % live should be slightly higher than % motile
• Usually performed using a vital stain, such as eosin Y, with a counterstain (nigrosin) – although could use a fluorescent
DNA stain, such as H33258.
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Leukocyte tests
• Cytochemical stain for peroxidase activity – benzidinecyanosine is the easiest to use (and it is available in a kit).
Only stains those cells with peroxidase activity so does not detect activated polymorphs or lymphocytes
•
Immunocytochemistry: double antibody assay (primary antibody is a mouse MAb to CD45), reaction is with alkaline phosphatase:anti-alkaline phosphatase complex (available in a kit)
• The tests are run on whole semen
• The normal range is < 1 × 10 6 / ml
• Values above this are considered to be clinically significant
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Retrograde ejaculation
•
In some men, the semen passes back into the bladder at ejaculation - this is confirmed by examination of a sample of postejaculatory urine
•
The man must take sodium bicarbonate the day before, and the day of, his appointment – to alkalinize his urine
•
Before collection, he should pass urine and then wait until he feels there is some urine in his bladder before masturbating
• He then collects a urine sample for analysis
•
Assess volume and pH of the urine
•
Centrifuge (600g for 10 min), resuspend pellets to a total of 20ml with sperm buffer + protein
•
Re-spin, resuspend pellets and combine – add buffer to a final volume of 1ml
•
Perform a standard semen analysis with this suspension
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
Post-vasectomy analysis
To determine the sperm concentration when few/none expected:
– centrifuge as much of the sample as possible (1000 g for 15 min) in a disposable conical centrifuge tube – note the exact volume used
–
Remove most of the supernatant - note volume removed
– Make at least 5 wet preps (10µl of resuspended pellet under a 22
× 22mm coverslip)
–
Search through at least 5 wet preps
–
If anything that looks like a sperm is seen – the report is “not clear”
–
Final decision is the responsibility of the Pathologist
© Oozoa Biomedical Inc, April 2005
SEMEN ANALYSIS
What tests should always be done?
Always:
•
Semen volume
• Sperm concentration
• Differential motility
•
Morphology
If there is an indication:
•
White cells
• Vitality
© Oozoa Biomedical Inc, April 2005
ABNORMAL SEMEN ANALYSIS
Treatments to correct abnormalities
• There is some evidence accumulating that there are some treatments which can improve semen analysis results, including:
– antioxidants
– carnitine
– reducing scrotal temperature
• However, there is still no good evidence that these changes in semen analysis results are related to improved fertility
• Therefore, two abnormal semen analyses will often lead to a couple being recommended fertility treatments
© Oozoa Biomedical Inc, April 2005
FERTILITY WORK-UP
• Fertility is a “couple” problem, and so both partners are assessed
• For the woman, the investigations may include hormone assessments (such as a day 3 FSH), a hysterosalpingogram, and/or a laparoscopy
• Both partners also undergo physical examinations
• For these functional assessments, the investigation is based on finding where the problem(s) lie – i.e. predicting failure
•
The treatment chosen is the one most likely to circumvent the problem(s) – i.e. increasing the likelihood of success
© Oozoa Biomedical Inc, April 2005
FERTILITY vs STERILITY not pregnant probably pregnant pregnant not pregnant possibly pregnant probably pregnant not pregnant not pregnant not pregnant
STERILE SUBFERTILE FERTILE
FEMALE PARTNER
© Oozoa Biomedical Inc, April 2005
FERTILITY TREATMENT OPTIONS
• If a partner is sterile (i.e. no gametes), then the couple would need donor gametes to achieve a pregnancy
•
If one or both partners are sub-fertile, then the treatment options are:
– no treatment, or ovulation induction
– intra-uterine insemination (+ ovulation induction)
–
in vitro fertilization (includes ICSI)
© Oozoa Biomedical Inc, April 2005
INTRA-UTERINE INSEMINATION (IUI)
• IUI is the least invasive of the ARTs - involves the selective washing of semen to isolate the motile spermatozoa (can’t put whole semen into the uterus)
• Up to 15 million motile spermatozoa are inseminated
• Advantages:
– relatively inexpensive – simple procedures
– minimal use of FSH
– can be used in consecutive cycles
– can usually start treatment virtually immediately
•
Disadvantages:
– lower success rate per cycle than other ARTs
© Oozoa Biomedical Inc, April 2005
IN VITRO FERTILIZATION (IVF)
Overview
•
There are many types of IVF
• For virtually all types, the woman is treated with “fertility drugs” to stimulate the development of a group of eggs (the average is around 10 – but the range can be enormous)
• Just prior to ovulation, the oocytes are retrieved
• That afternoon, they are inseminated with prepared sperm
• Inseminated eggs checked the next day for fertilization
• The fertilized eggs are kept in culture for up to 5-6 days
• Embryo transfer / possibly cryopreservation
© Oozoa Biomedical Inc, April 2005
IN VITRO FERTILIZATION (IVF)
Fertilization and embryo development
© Oozoa Biomedical Inc, April 2005
IN VITRO FERTILIZATION (IVF)
Intracytoplasmic sperm injection (ICSI)
• ICSI and its variants - the highest-level ART
•
One sperm is injected directly into an egg
•
Only mature eggs injected
•
After the insemination, the rest of the lab procedures are the same as for “standard”
IVF
© Oozoa Biomedical Inc, April 2005
IN VITRO FERTILIZATION (IVF)
Risks and rewards
•
IVF gives the highest chance of pregnancy per cycle – although this is still controlled by the woman’s age
• Traditionally there was a high risk of multiple pregnancy with IVF – as several embryos were transferred at once
•
The new culture systems give embryos with a much higher chance of implanting – so fewer are transferred
• The advent of ICSI has allowed men with very poor fertility prognoses (including azoospermia) to become biological fathers
•
This can bring the requirement for genetic counselling prior to treatment (Y-chromosome deletions, etc.)
© Oozoa Biomedical Inc, April 2005
ART SUCCESS AND FEES
Pregnancy rates (women < 37 years old):
•
No treatment / fertile couple: around 15-20% per cycle
•
IUI + COH: 20% per cycle
•
IVF (includes ICSI): 50-60% per cycle (was about 10%)
Cost in BC (excluding drugs, which can be $2000–$4000):
•
IUI + COH: $300 – $400
•
IVF: $4500 – $4700
•
ICSI: $5750 – $6250
•
ICSI with aspirated sperm: $6250 – $6500 (+ urologist fees)
© Oozoa Biomedical Inc, April 2005
TREATMENT OPTIONS
Normal semen analysis
The recommended treatment will depend on the woman’s test results, and could be:
•
No treatment: if her results were normal, and she is young, and they have been trying for only a short time (< 1 year)
•
IUI: if the couple has already been trying for some years and the woman has normal results
•
IVF: if the woman is in her mid to late thirties, or if she has blocked tubes
© Oozoa Biomedical Inc, April 2005
TREATMENT OPTIONS
Low concentration (oligozoospermia)
The recommended treatment will depend on the woman’s test results, and could be:
•
IUI: if enough motile sperm can be recovered from the ejaculate (and if the woman’s results are normal)
•
IVF: if enough sperm can be recovered from the ejaculate, and if the woman is older, or has blocked tubes.
•
ICSI: only need to be able to isolate as many motile sperm as there are eggs, so used in cases of extreme oligozoospermia
•
ICSI with aspirated sperm: in the case of ejaculatory azoospermia (i.e. there are sperm in the testes but not in the ejaculate)
© Oozoa Biomedical Inc, April 2005
TREATMENT OPTIONS
Low motility (asthenozoospermia)
The recommended treatment will depend on the woman’s test results, and could be:
•
IUI: less likely, and depends on whether enough sperm with good progressive motility can be recovered, and if the woman’s results are normal
•
IVF: if enough motile sperm can be recovered from the ejaculate, with a final total motility of >90% with good progression (and if hyperactivation is seen)
•
ICSI: quite likely, as the sperm may not be able to generate enough power to break through the outer layer of the egg
(the zona pellucida)
© Oozoa Biomedical Inc, April 2005
TREATMENT OPTIONS
Poor morphology (teratozoospermia)
•
If the sperm morphology is very poor, then ICSI is the most likely option
• This is due to the high likelihood of failure of fertilization by IUI or IVF, related to functional failure in sperm-egg interactions, including:
–
Geometric interference in sperm-egg binding (head too round, or too long)
–
Interference in penetration of the zona (low energy, poor transmission of force due to midpiece or tail defects)
© Oozoa Biomedical Inc, April 2005
RESEARCH & NEW TECHNIQUES
Sperm kinematics
•
The way sperm swim affects their fertility
• To get through the cervix, they have to swim in a straight path
• To get through the outer layer of the egg, they have to generate a lot of power – this is seen as hyperactivated motility
© Oozoa Biomedical Inc, April 2005
RESEARCH & NEW TECHNIQUES
Sperm kinematics
•
The sperm tracks are analyzed and a number of kinematic parameters are derived, including:
–
Velocity (VCL, VSL and VAP)
–
Velocity ratios (expression of the path shape and regularity)
–
Amplitude of lateral head displacement
–
Beat/cross frequency
•
The proportion of sperm in a sample which meet particular kinematic criteria is used to predict (failure) of:
–
Mucus-penetrating ability
–
Hyperactivation (a marker of sperm function)
© Oozoa Biomedical Inc, April 2005
RESEARCH & NEW TECHNIQUES
CASA
• Computer-aided sperm analysis
•
Able to assess the kinematics of hundreds of sperm in a couple of minutes
• Means that these tests can be part of the infertility work-up
© Oozoa Biomedical Inc, April 2005
RESEARCH & NEW TECHNIQUES
ROS and sperm
© Oozoa Biomedical Inc, April 2005
RESEARCH & NEW TECHNIQUES
Sperm DNA Damage
Sperm Chromatin Structure Assay: SCSA™
© SCSA Diagnostics Inc, Brookings, SD, USA
Evenson et al. (1980) Science 240:1131-1133 © Oozoa Biomedical Inc, April 2005
RESEARCH & NEW TECHNIQUES
Structured management
•
Use the test results to predict where blocks to fertilization are occurring
•
A treatment plan to go around these blocks is created for each couple
•
It is designed to maximize the chance of achieving a successful pregnancy in the most practicable and economical way
• The treatment plan is implemented after consultation with the couple
© Oozoa Biomedical Inc, April 2005
The WHO and Structured Management
(2000)
© Oozoa Biomedical Inc, April 2005
STANDARDIZATION & QUALITY
CONTROL
Fundamental requirements of all laboratory tests :
• appropriate and robust methodology
• careful training
• operator experience
} accuracy & precision
• suitable assay control limits
• regular internal comparisons
• regular external comparisons
• cost effectiveness
= IQC
= EQA
College of Reproductive Biology Inaugural Meeting, Houston, May 1997
© Oozoa Biomedical Inc, April 2005
ISO 15189:2003
Medical laboratories – Particular requirements for quality and competence.
5.5.1
Appropriate procedures that meet the needs of the users of the laboratory’s services shall be used.
5.5.2
Only validated procedures shall be used.
5.5.3
All procedures must be documented and available: a) purpose b) principle c) performance specifications d) primary sample(s) e) sample container f) equipment & reagents g) calibration h) procedural steps i) QC procedures j) sources of interference k) calculation of results (includes
uncertainty of measurement) l) reference intervals m) reportable interval for patients n) alert &/or critical values o) interpretation by laboratory p) safety precautions q) potential sources of variability
5.5.4
Performance specifications must related to intended use.
5.5.5
Periodic review of biological reference intervals
© Oozoa Biomedical Inc, April 2005
QC IN SEMEN ANALYSIS
Mean ± SD% differences between 4 trained andrology scientists using WHO manual/visual semen analysis methods on 60 determinations. (Calgary Diagnostic Semen Lab, ca. 1990)
A
B
C
D
Concentration
-2.3 ± 7.4
-1.7 ± 4.9
+4.5 ± 7.3
-0.5 ± 7.0
Total motility
+0.3 ± 3.0
-0.8 ± 3.1
-1.0 ± 3.3
+1.6 ± 2.9
Prog motility
+0.4 ± 2.6
-0.8 ± 2.9
-0.6 ± 3.3
+1.0 ± 2.8
© Oozoa Biomedical Inc, April 2005
TRAINING IN SEMEN ANALYSIS
© Oozoa Biomedical Inc, April 2005
GOAL-ORIENTED TRAINING
•
Originally elaborated in Calgary during the mid/late 1980s as a means to facilitate the training of new staff.
• Subsequently applied in numerous locations where we were involved in training andrology lab staff: e.g. Sydney (Australia), London (UK), Stockholm (Sweden),
Boston (USA), Bangkok (Thailand).
•
Adopted by the ESHRE Andrology SIG Education Subcommittee as the basis for their Basic Semen Analysis
Courses (25 run by the end of 2003).
© Oozoa Biomedical Inc, April 2005
ESHRE Basic Semen Analysis Courses
© Oozoa Biomedical Inc, April 2005
CONCLUSION
•
Semen analysis is an important laboratory test and should be thought of in the same way as any other diagnostic assay
• It is used in determining treatment plans for infertility
•
The results can therefore have a huge impact on the level of intervention, with the associated emotional and financial costs to the couple
© Oozoa Biomedical Inc, April 2005