Inflammation/Fever
advertisement

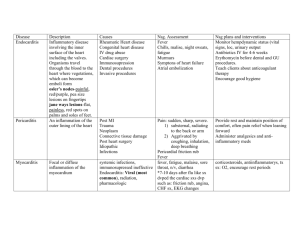
Review of Inflammation and Fever 1 Inflammation A non-specific response to injury or necrosis that occurs in a vascularized tissue. Signs: Redness, heat ,swelling, pain, and loss of function (Rubor, calor, tumor, dolor) -- itis refers to an inflammatory condition 2 Stages of Inflammation • Vascular stage • Cellular stage • Tissue repair 3 4 5 Response at site of injury: blood vessels briefly constrict, then dilate Edema: due to increased pressure in vessels blood vessels become permeable plasma forced into tissues = transudate Exudates - small proteins and cells 6 7 Functions of transudates and exudates: • dilute toxins from dead cells • pain – limits use; prevents additional injury • carry blood cells and proteins to site (antibodies and complement) • carry toxins and wastes from site (mostly through lymphatic system) 8 Cellular Stage • Marked by movement of white blood cells (leukocytes) to the area of injury. • When fluid is lost from blood, blood becomes more viscous. See change in blood flow patterns which allows white cells to move to the edges of the blood stream – margination. 9 Release of chemical mediators and cytokines cause the leukocytes to increase production of adhesion molecules. Leukocytes –neutrophils, macrophages – phagocytic cells, leave the capillaries and enter tissues by transmigration or emigration. 10 11 • Biochemicals released by leukocytes and tissue cells serve as signals to coordinate all body defenses. • “calling molecules” • Movement of leukocytes – chemotaxis • Neutrophils then macrophages • Steps of phagocytosis: – Adeherence plus opsoniztion – Engulfment – Intracellular killing • die - form pus 12 13 Platelets – stop bleeding in injured vessels histamines Plasma protein systems – Complement – MAC, vasodilation, opsonization Clotting Kinins – signal endothelial cells to shrink bradykinins contributes to pain Immunoglobulins 14 • Other mediators: –Prostaglandins –Platelet-activating factor –Cytokines –Nitric oxide 15 Systemic manifestations of inflammation • Release of cytokines in Acute-phase response: – Affects hypothalamus and may cause fever – Affects bone marrow, ↑ neutrophil production – Affects the CNS causing lethargy – Affects liver to produce more fibinogen and Creactive protein, which increases the ESR • Lymphadenitis 16 Excessive inflammation • Prolonged pain • Swelling impairs function • Therapies: – Temperature • Cold - 10 on 10 off (or alternate heat and cold) – Elevation and pressure – Drug therapy • Antihistamines, nonsteroidal anti-inflammatory agents, corticosteroids 17 Chronic Inflammation • May last for weeks, months or years – Recurrent acute inflammation or low-grade responses • Characteristics: – Infiltration by macrophages and lymphocytes – Proliferation of fibroblasts instead of exudates – Cause may be foreign matter, viruses, bacteria, fungi or larger parasites 18 Excessive inflammation • Pain is intense or prolonged and swelling impairs function of organ • Cold – 10 minutes only • Drugs – steroids • Elevation – decreases blood flow 19 Resolution or Tissue Repair • Inflammatory phase • Proliferative phase • Remodeling phase 20 Resolution and repair: resolution – restoration of normal tissue structure and function. repair – replacement of destroyed tissue with scar tissue. Débridement, suturing Vessel dilation and permeability are reversed Leukocyte migration ends Exudate is drained away – lymphatics 21 Repair – scar formation Processes fill the wound cover the wound shrink the wound 22 Impairment of inflammation Excess bleeding Circulation at site of injury Bone marrow health Immune response function Nutritional status: protein, methionine, zinc, vitamin C, copper 23 Fever (pyrexia) • Called “hallmark of infection” • Many infections are called fevers: – Typhoid fever, rheumatic fever, etc. 24 Normal thermoregulation Body temperature is maintained within ± 1oF Varies over the course of the day Cells constantly produce heat by metabolism Mechanisms to lose heat: dilation of surface blood vessels sweating Body temperature is set and controlled by the hypothalamus 25 With infection (or some toxins) : some bacteria release biochemicals into blood stream – exogenous pyrogens (esp. lipopolysaccharides of Gram-negative bacteria) – these signal white blood cells (monocytes/macrophages) to produce their own biochemicals – endogenous pyrogens (interleukins or interferons) – induce synthesis of prostaglandins – cause hypothalmus to raise its set point. 26 • Many non-infectious disorders can also produce fever • NON-SPECIFIC • Patterns of fever: – Intermittent fever – Remittent fever – Sustained or continuous fever – Recurrent or relapsing fever • Heart rate increases with fever 27 • Hypothalamus : – releases TSH to increase production of T3 & T4 – releases ACTH which increases release of glucocorticoids – Causes increase of release of epinephrine – Decreases production of ADH 28 Prostaglandins inhibited by non-steroidal antiinflammatory drugs (aspirin, tylenol, motrin etc.) (although overdose of aspirin raises body temp.) 29 Benefits of fever Increased temperature kills microorganisms and adversely affects their growth and reproduction Decrease serum levels of iron, copper and zinc – needed for bacterial reproduction 30 Causes lysosomal breakdown and autodestruction of cells, preventing viral replication in infected cells Increased leukocyte motility Facilitates the immune response – activation of T cells Enhances phagocytosis Production of interferon increased 31 But fever is bad when: too high – impairs neurological and/ respiratory functions increased work load of heart in patients with heart disease or stroke damage to hypothalamus can cause temp. to become dangerously high Can cause complications in pregnancy Fever over 106oF requires emergency care 32 • Infants under 3 months of age have difficulty regulating temperature • Young children can develop very high fevers • Body temperature is lowered in the elderly, so fevers are not as high 33