Cerebrovascular Accident “Brain Attack”

Cerebrovascular Accident (CVA) aka “Brain Attack”
Chris Puglia, MSN, RN, CEN
Objectives
• Define cerebrovascular accident and associated terminology
• Discuss related pathophysiology and presentation of various types of stroke
• Discuss etiology, risk factors, diagnostics, management, and outcomes of stroke
• Review case studies and nursing diagnoses, interventions, and goals
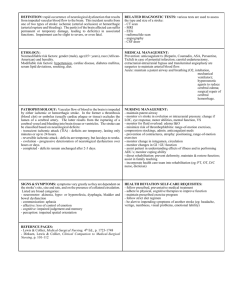
Definition
• Cerebral Vascular Accident (CVA), Stroke or
“brain attack” is an acute CNS injury that results in neurologic S/S brought on by a reduction or absence of perfusion to a territory of the brain. The disruption in flow is from either an occlusion (ischemic) or rupture
(hemorrhagic) of the blood vessel.
Incidence & Prevalence
• Third leading cause of death in the USA
– 795,000+ people/year
– 175,000 die within one year (25%)
• Leading cause of long-term disabilities
– 5.5 million survivors (USA)
– 15 to 30 % live with permanent disability
Definitions
• Cerebrovascular Accident
– Ischemic Stroke
• Thrombotic
• Embolic
• Lacunar infarct
• TIA
– Hemorrhagic Stroke
• ICH
• SAH
Thrombotic Stroke
• Occlusion of large cerebral vessel (blood clot)
• Older population
• Sleeping/resting
• Rapid event, but slow progression (usually reach max deficit in 3 days)
Embolic Stroke
• Embolus becomes lodged in vessel and causes occlusion
• Bifurcations are most common site
• Sudden onset with immediate deficits
– Embolysis
– Hemorrhagic
Transformation
Lacunar Strokes - 20% of all stokes
• Minor deficits
– Paralysis and sensory loss
• Lacune
• Small, deep penetrating arteries
• High incidence:
– Chronic hypertension
– Elderly
– DIC
Transient Ischemic Attack
• Warning sign for stroke
• Brief localized ischemia
• Common manifestations:
– Contralateral numbness/ weakness of hand, forearm, corner of mouth
– Aphasia
– Visual disturbancesblurring
• Deficits last less than 24 hours (usually less than
1 or 2 hrs)
• Can occur due to:
– Inflammatory artery disorders
– Sickle cell anemia
– Atherosclerotic changes
Hemorrhagic Stroke Definitions
• Intracerebral hemorrhage
• Intracranial hemorrhage
• Parenchymal hemorrhage
• Intraparenchymal hematoma
• Contusion
• Subarachnoid hemorrhage
Hemorrhagic Stroke
• Rupture of vessel
• Sudden
• Fatal
• Causes:
– HTN
– Trauma
• Varied manifestations
Hemorrhagic Stroke
– Intracerebral
Hemorrhage (ICH)
– Subarachnoid
Hemorrhage (SAH)
Pathophysiology
Hemorrhagic Stroke
• Changes in vasculature
• Tear or rupture
• Hemorrhage
• Decreased perfusion
• Clotting
• Edema
• Increased intracranial pressure
• Cortical irritation
Physiology
Normal Cerebral Blood Flow
• Oxygen
• Glucose
• 20% of Cardiac Output / Oxygen
• Arterial supply to the brain:
– Internal carotid (anteriorly)
– Vertebral arteries (posteriorly)
• Venous drainage
– 2 sets of veins - venous plexuses
• Dural sinuses to internal jugular veins
• Sagittal sinus to vertebral veins
– No valves, depend on gravity and venous pressure gradient for flow
NON-MODIFIABLE
Age
2/3 over 65
Gender
M=F
Female>fatality
Race
AA > hispanics, NA
Asians > hem
Heredity
Family history
Previous TIA/CVA
Risk Factors
MODIFIABLE
• Hypertension
• Diabetes mellitus
• Heart disease
• A-fib
• Asymptomatic carotid stenosis
• Hyperlipidemia
• Obesity
• Oral contraceptive use
• Heavy alcohol use
• Physical inactivity
• Sickle cell disease
• Smoking
• Procedure precautions
Etiology
Ischemic Stroke
Embolism
• Atrial fib
• Sinoatrial D/O
• Recent MI
• Endocarditis
• Cardiac tumors
• Valvular D/O
• Patent foramen ovale
• Carotid/basilar artery stenosis
• Atherosclerotic lesions
• Vasculitis
Prothrombotic states
• Hemostatic regulatory protein abnormalities
• Antiphospholipid antibodies
• Hep cofactor II
Etiology
Hemorrhagic Stroke
• Chronic HTN**
• Cerebral Amyloid Angiopathy*
• Anticoagulation*
• AVM
• Ruptured aneurysm (usually subarachnoid)
• Tumor
• Sympathomimetics
• Infection
• Trauma
• Transformation of ischemic stroke
• Physical exertion, Pregnancy
• Post-operative
Aneurysm
• Localized dilation of arterial lumen
• Degenerative vascular disease
• Bifurcations of circle of Willis
– 85% anterior
– 15% posterior
Aneurysm
Subarachnoid Hemorrhage
SAH
Mortality 70%
97% HA
Nuchal rigidity
Fever
Photophobia
Lethargy
Nausea
Vomiting
Aneurysm/SAH
• Complications
– HCP (hydrocephalus)
– Vasospasm
• Triple H Therapy
– HTN
– Hemodilution
– Hypervolemia
• Surgical treatment
– Clip
– Coil
• Surgical Coil
– INR
Nursing Management
• Assessment
• Monitoring
– BP
– TCDs
– CBC
• Preventing complications
– Bowel program
– DVT prophylaxis
– Siezure prophylaxis
– Psychological support
– Discharge planning
Arteriovenous Malformations
• AVM
– Tangled mass of arteries and veins
– Seizure or ICH
• Endovascular
• Neurosurgery
• Radiosurgery
Treatment
AVM
Presentation
• Sudden onset
• Focal neurological deficit
• Progresses over minutes to hours
• HA, N/V, <<LOC, HTN
• Depends on location
Stroke Symptoms include:
• SUDDEN numbness or weakness of face, arm or leg
• SUDDEN confusion, trouble speaking or understanding.
• SUDDEN trouble with vision
• SUDDEN trouble walking, dizziness, loss of balance or coordination
• SUDDEN severe HA
Manifestations by Vessel
• Vertebral Artery
– Pain in face, nose, or eye
– Numbness and weakness of face (involved side)
– Gait disturbances
– Dysphagia
– Dysarthria (motor speech)
Manifestations by Vessel
• Internal Carotid Artery
– Contralateral paralysis (arm, leg, face)
– Contralateral sensory deficits
– Aphasia (dominant hemisphere involvement)
– Apraxia (motor task),
– Agnosia (obj. recognition),
– Unilateral neglect (non-dominant hemisphere involvement)
– Homonymous hemianopia
Manifestations & Complications by Body System
• Neurological
– Hyperthermia
– Neglect syndrome
– Seizures
– Agnosias (familiar obj)
– Communication deficits
• Aphasia (expressive, receptive, global)
• Agraphia
– Visual deficits
• Homonymous hemianopia
• Diplopia
• Decreased acuity
• Decreased blink reflex
Manifestations & Complications by Body System
Neurological (cont.)
Cognitive changes
Memory loss
Short attention span
Poor judgment
Disorientation
Poor problemsolving ability
– Behavioral changes
• Emotional lability
• Loss of inhibitions
• Fear
• Hostility
Manifestations & Complications by Body System
• Musculoskeletal
– Hemiplegia or hemiparesis
– Contractures
– Bony ankylosis
– Disuse atrophy
– Dysarthria - word formation
– Dysphagia – swallow
– Apraxia – complex movements
– Flaccidity/spasticity
• GU
– Incontinence
– Frequency
– Urgency
– Urinary retention
– Renal calculi
Manifestations & Complications by Body System
• Integument
– Pressure ulcers
• Respiratory
– Respiratory center damage
– Airway obstruction
– Decreased cough ability
• GI
– Dysphagia
– Constipation
– Stool impaction
Initial Stroke Assessment/Interventions
• Neurological assessment
• Call “Stroke Alert” Code
• Ensure patient airway
• VS
• IV access (What size?)
• Maintain BP within parameters (check MAP)
• Position head midline
• HOB 30 (if no shock/injury)
• CT, blood work, data collection
• NIH Stroke Scale
• Anticipate thrombolytic therapy for ischemic stroke
NIH Stroke Scale Score
• Standardized method
– measures degree of stroke r/t impairment and change in a patient over time.
• Helps determine if degree of disability merits treatment with tPA .
– As of 2008 stroke patients scoring greater than 4 points can be treated with tPA.
• Standardized research tool to compare efficacy stroke treatments and rehabilitation interventions.
• Measures several aspects of brain function, including consciousness, vision, sensation, movement, speech, and language not measured by Glasgow coma scale.
NIH Stroke Scale
Handout
Current NIH Stroke Score guidelines for measuring stroke severity:
Points are given for each impairment.
0= no stroke
1-4= minor stroke
5-15= moderate stroke
15-20= moderate/severe stroke
21-42= severe stroke
A maximal score of 42 represents the most severe and devastating stroke.
Acute Stroke Times
Question
A patient is admitted to the hospital with a left hemiplegia. To determine the size and location and to ascertain whether a stroke is ischemic or hemorrhagic, the nurse anticipated that the health care provider will request a
A. CT scan.
B. lumbar puncture.
C. cerebral angiogram.
D. PET scan.
Diagnostics
Tests for the Emergent Evaluation of the Patient with Acute
Ischemic Stroke
• CT head (-)
• Electrocardiogram
• Chest x-ray
• Hematologic studies (complete blood count, platelet count, prothrombin time, partial thromboplastin time)
• Serum electrolytes
• Blood glucose
• Renal and hepatic chemical analyses
• National Institute of Health Scale (NIHSS) score
Ischemic Stroke
Diagnostics
Hemorrhagic Stoke
Medical Management
• BP
– MAP
– CPP
• Factor VII, Vit K, FFP
• ICP
– HOB
– Sedation
– Osmotherapy
– Hyperventilation
– Paralytics
• Fluid management
– euvolemia
• Seizure prophylaxis
– Keppra
– Dilantin
• Sedation
• Body temperature
• PT/OT/ST
• DVT prophylaxis
Ischemic
• Medical management
• tPA
• Endovascular
– Carotid endarectomy
– Merci clot removal
• Clot removal
Treatment
Hemorrhagic
• Medical management
• Decompression
– Craniotomy
– Craniectomy
PT/OT/ST
REHABILITATION
Medications
Anti-coagulants – A fib & TIA
• Antithrombotics
Calcium channel blockers – Nimotop (nimodipine)
Corticosteroids ???
Diuretics – Mannitol, Lasix (Furosemide)
Anticonvulsants – Dilantin (phenytoin) or Cerebyx
(Fosphenytoin Sodium Injection)
Thrombolytics - tPA (recombinant tissue plasminogen activator)
Medications
• Thrombolytics Recombinant Alteplase (rtPA)
Activase, Tissue plasminogen activator
– Treatment must be initiated promptly after CT to R/O bleed
• Systemic within 3 hours of onset of symptoms
• Intra-arterial within 6 hours of symptoms
– Some exclusions:
• Seizure at onset
• Subarachnoid hemorrhage
• Trauma within 3 months
• History of prior intracranial hemorrhage
• AV malformation or aneurysm
• Surgery 14 days, pregnancy,
• Cardiac cath. 7 days
Neurosurgical Management
• Craniotomy
– Craniotomy Procedure
• Craniectomy
Neurosurgical Management
• EVD placement
• ICP monitor placement
Recommendations for Surgical
Treatment of ICH
• Nonsurgical candidates
– Small hemorrhage
– Minimal deficit
– GCS </= 4 (unless brain stem compression)
– Loss of brainstem fxn
– Severe coagulopathy
– Basal ganglion or thalamic
• Surgical candidates
– >3cm
• Neuro deficit
• Brain stem compression
• HCP
– Aneurysm, AVM, cavernous hemangioma
– Young with mod/large lobar hemorrhage and clinical deterioration
Question
• A carotid endarectomy is being considered as treatment for a patient who has had several TIAs.
The nurse explains to the patient that this surgery
– A. is used to restore blood circulation to the brain following an obstruction of a cerebral artery.
– B. involves intracranial surgery to join a superficial extracranial artery to an intracranial artery.
– C. involves removing an atherosclerotic plaque in the carotid artery to prevent an impending stroke.
– D. is used to open a stenosis in a carotid artery with a balloon and stent to restore cerebral circulation.
Standing Orders
• Per facility policy
Nursing Concerns
• Medical management!
• Post-op care
• Mobilization
• Nutrition
• Constipation
• Skin
• Infection
• Patient/family teaching
• Follow-up
• Medications
• Resources available
Question
• An essential intervention in the emergency management of the patient with a stroke is
– A. intravenous fluid replacement.
– B. administration of osmotic diuretics to reduce cerebral edema.
– C. initiation of hypothermia to decrease oxygen needs of the brain.
– D. maintenance of respiratory function with a patent airway and oxygen administration.
Nursing Diagnosis
• Ineffective cerebral tissue perfusion
• Impaired mobility
• Self-care deficit
• Impaired verbal communication
• Impaired swallowing
Nursing Diagnoses/Interventions
• Ineffective Tissue Perfusion
– Goal is to maintain cerebral perfusion
• Monitor respiratory status
• Auscultate, monitor lung sounds
• Suction as needed – increases ICP (< 10 seconds)
• Place in side-lying position (secretions)
• O
2 as needed/prescribed
• Assess LOC, other neuro vital signs
• NIH Stroke Scale
• Glasgow Coma Scale – Eyes, Verbal, & Motor
Nursing Diagnoses/Interventions
• Ineffective Tissue Perfusion (cont)
• Monitor strength/reflexes
• Assess for HA, sluggish pupils, posturing
• Monitor cardiac status
• Monitor I&O’s
– Can get DI as result of pituitary gland damage
• Monitor seizure activity
Nursing Diagnoses/Interventions
• Impaired Physical Mobility
– Goal is to maintain and improve functioning
• Active ROM for unaffected extremities
• Passive ROM for affected extremities
• Q2 hr turns
• Assess for thrombophlebitis
• Confer with PT for movement and positioning techniques for each stage of rehab
Nursing Diagnoses/Interventions
• Impaired Physical Mobility
Flaccidity & spasticity
Meds used to treat spasticity:
Kemstro or Lioresal (baclofen)
Valium (diazepam)
Dantrium (dantrolene sodium)
Zanaflex (tizanidine hydrochloride)
New drugs being tried –
– Neurontin (Gabapentin) & Botox (botulinum toxin)
Nursing Diagnoses/Interventions
• Self-Care Deficit
– Goals are to promote functional ability, increase independence, improve self-esteem
• Encourage use of unaffected arm in ADLs
• Self-dressing (using unaffected side to dress affected side first)
• Sling or support for affected arm
• Confer with OT for techniques to promote return to independence
Nursing Diagnoses/Interventions
• Impaired Verbal Communication
– Goal is to increase communication
• Speak in normal tones unless there is a documented hearing impairment
• Allow adequate time for responses
• Face center person when speaking, speak simply and enunciate words
• If you don’t understand what the patient is saying, let them know, and have them try again
Nursing Diagnoses/Interventions
• Impaired Verbal Communication (cont)
• Try alternate method of communication if needed
– Writing, computerized boards, etc
• Allow patient anger and frustration at loss of previous functioning
• Allow patient to touch (hands, arms), may be the only way of expressing (comfort, etc)
• If patient has visual disturbances:
– During initial phase of recovery, position where patient can easily see you; in later stages, patient can be directed to adjust position for visual contact
Nursing Diagnoses/Interventions
• Impaired Swallowing
– Goal is safety, adequate nutrition, and hydration
• Position person upright, using puree or finely chopped soft foods
• Hot or cold food or thickened liquids
• Teach patient to put food behind teeth on unaffected side and tilt head backwards
• Check for food pockets, especially on affected side
• Have suctioning equipment at bedside
• Minimize distractions while eating
• Never leave patient with food etc. in mouth
Question
A patient with a right hemisphere stroke has a nursing diagnosis of unilateral neglect R/T sensoryperceptual deficits. During the patient’s rehabilitation, it is important for the nurse to
A. avoid positioning the patient on the affected side.
B. place all objects for care on the patient’s unaffected side.
C. teach the patient to care consciously for the affected side.
D. protect the affected side from injury with pillows and supports.
Question
A patient who experienced a thrombotic stroke and has residual hemiparesis of the right side is undergoing rehabilitation. The nurse caring for this pt reinforces OT recommendations by placing items for personal hygiene:
A. on the overbed table on the right side.
B. on the overbed table on the left side.
C. one foot away from the bed on the right side.
D. one foot away from the bed on the left side.
Complications
• Increased intracranial pressure
• Rebleeding
• Vasospasm
• HCP
• Death
• Age
• Size, volume
• Location
• HCP, IVH
• Deficit, LOC, MAP
• Duration
• Co-morbidities
Outcomes
• 44% mortality
Evaluation
• Reduce mortality and morbidity
• Baseline neurological function
• Outcomes
• Evidenced based practice
Patient/Family Education
• PREVENTION is key
– Smoking cessation
– Physical activity
• Weight reduction
– Diet
• Plavix
– LDL chol reduction
• Statins
• > HDL
– BP normalization
• ACE inhibitors
• ARB
• Thiazide diuretics
– Antiplatelet agents
• ASA
– DM
– ETOH
– Homocysteine reduction
Legal/Ethical Concerns
• Advanced directives
– MPOA
• Category status
• Code status
• Withdrawal of care
• Palliative care
• Placement
Resources www.stroke.org
-- National Stroke Association (800-787-
6537) www.ninds.nih.gov
-- National Institute of Neurological
Disorders and Stroke (800-352-9424) www.naric.com
-- National Rehabilitation Information
Center (8003462742) www.aphasia.org
-- National Aphasia Association (800-
922-4622) www.aan.com
-- American Academy of Neurology www.dynamic-living.com
-- Daily living products www.ninds.nih.gov/doctors/NIH_Stroke_Scale.pdf
-- NIH stroke scoring system www.strokecenter.org/trials -- Find a clinical trial on stroke
Question
• The incidence of ischemic stroke in patients with TIAs and other risk factors is reduced with the administration of
– A. furosemide (Lasix).
– B. lovastatin (Mevacor).
– C. daily low-dose aspirin (ASA).
– D. nimodipine (Nimotop).
Question
• A diagnosis of a ruptured cerebral aneurysm has been made in a patient with manifestations of a stroke. The nurse anticipates that treatment options that would be evaluated for the patient include a. hyperventilation therapy.
b. surgical clipping of the aneurysm.
c. administration of hypersomotic agents.
d. administration of thrombolytic therapy.
Question
• A nursing intervention that is indicated for the patient with hemiplegia is
– A. the use of a footboard to prevent plantar flexion.
– B. immobilization of the affected arm against the chest with a sling.
– C. positioning the patient in bed with each joint lower that the joint proximal to it.
– D. having the patient perform passive ROM of the affected limb with the unaffected limb.
Question
The nurse can assist the patient and the family in coping with the long-term effects of a stroke by
A. informing the family members that the patient will need assistance with almost all ADLs.
B. explaining that the patient’s prestroke behavior will return as improvement progresses.
C. encouraging the patient and family members to seek assistance from family therapy or stroke support group.
D. helping the patient and family understand the significance of residual stroke damage to promote problem solving and planning.