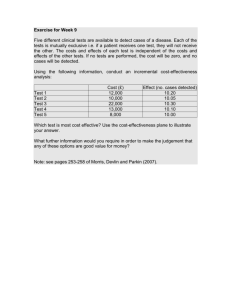
Quality of life and health utility in drug abuse comparative
advertisement

Quality of life and health utility in drug abuse comparative effectiveness and cost-effectiveness research Bruce R. Schackman, PhD Department of Public Health Weill Cornell Medical College January 23, 2013 Center for Advancing Longitudinal Drug Abuse Research UCLA Integrated Substance Abuse Programs Funding and financial disclosures • Funding – National Institute on Drug Abuse: R01 DA027379; R01 DA033424; R01 DA031059 – National Institute of Mental Health: R01 MH087328 – National Institute of Allergy and Infectious Diseases: R37 A1042006 – Robert Wood Johnson Foundation Substance Abuse Policy Research Program Grant #63625 • Financial Disclosures: None 2 Health care costs are rising Rettenmaier and Wang, 2009 3 Drug abuse treatment is becoming part of the health care system • Parity requirements in health insurance coverage • Impact of health reform on expanded access to health insurance • More medication-assisted treatment options • Consolidation of mental health and substance abuse treatment systems 4 Drug abuse treatment is becoming part of the health care system: implications • Investments in drug abuse treatment should be valued on the same basis as treatment for other chronic diseases – Benefit to the patient – Efficiency – Cost-savings not required 5 Paying for value • • • • • • Pay for performance Value-based purchasing Comparative effectiveness Patient-centered outcomes Cost-effectiveness The “R” word 6 Agenda • Comparative effectiveness and patientcentered outcomes definitions • Quality-of-life measures • Cost-effectiveness overview • Cost-effectiveness of medication-assisted treatment of opioid dependence • Addressing methodological and data gaps: planned studies 7 Comparative effectiveness research (CER) “Comparative effectiveness research is the conduct and synthesis of research comparing the benefits and harms of different interventions and strategies to prevent, diagnose, treat, and monitor health conditions in “real world” settings. The purpose of this research is to improve health outcomes by developing and disseminating evidence-based information to patients, clinicians and other decision makers, responding to their expressed needs, about which interventions are most effective for which patients under specific circumstances.” Coordinating Council for Comparative Effectiveness Research, 2009 http://www.hhs.gov/recovery/programs/cer/cerannualrpt.pdf 8 Categories of methods for CER • Systematic reviews, including meta-analysis • Decision modeling, with or without cost information • Retrospective analysis of existing clinical or administrative data, including “natural experiments” • Prospective observational studies, including registries, which observe patterns of care and outcomes but do not assign patients to specific study groups • Experimental studies, including randomized clinical trials (RCTs), in which patients or groups of patients are assigned to alternative treatments, practices, or policies Tunis SR, Benner J, McClellan M. Stat Med 2010;29:1963-76. 9 Estimated types of CER studies by federal agency/department 2006-2009 Study Type AHRQ n = 144 NIH DoD VHA Total n = 466 n = 25 N = 96 Randomized controlled trial 11% 79% 0% 77% 60% Practical/pragmatic controlled trial 3% 1% 16% 1% 2% Other non-randomized controlled trial 2% 2% 32% 0% 3% Observational study (natural experiment) 1% 2% 0% 4% 3% Observational study (prospective registry) 4% 3% 16% 6% 4% Observational study (retrospective) 9% 5% 6% 4% 6% Systematic review 58% 0% 13% 0% 14% Meta-analysis 3% 0% 0% 0% 1% Mathematical model 4% 3% 3% 3% 3% Federal Coordinating Council for Comparative Effectiveness Research, 2009 http://www.hhs.gov/recovery/programs/cer/cerannualrpt.pdf 10 Estimated types of interventions in CER studies by federal agency/department 2006-2009 Study Type AHRQ n = 144 NIH n = 466 DoD n = 25 VHA N = 96 Total Pharmacologic treatment 35% 68% 24% 10% 34% Biologic treatment 1% 1% 10% 4% 4% Alternative medicine 2% 8% 1% 2% Medical device/equipment 17% 0% 7% 11% Surgical procedure 11% 3% 9% 9% Behavioral intervention 11% 11% 24% 16% Public health intervention 2% 17% 3% 3% Delivery system 11% 19% 41% 20% Other 10% 8% 1% 2% 6% 24% Federal Coordinating Council for Comparative Effectiveness Research, 2009 http://www.hhs.gov/recovery/programs/cer/cerannualrpt.pdf 11 Patient-centeredness “Patient-centeredness refers to the extent to which the preferences, decision-making needs, and characteristics of patients are addressed, and is the key characteristic differentiating PCOR from comparative effectiveness research.” Methods Committee of PCORI. JAMA 2012;307:1636-40. 12 Patient-centered outcomes research • Assesses the benefits and harms of preventive, diagnostic, therapeutic, palliative, or health delivery system interventions to inform decision making, highlighting comparisons and outcomes that matter to people; • Is inclusive of an individual’s preferences, autonomy and needs, focusing on outcomes that people notice and care about such as survival, function, symptoms, and health related quality of life; • Incorporates a wide variety of settings and diversity of participants to address individual differences and barriers to implementation and dissemination; and • Investigates (or may investigate) optimizing outcomes while addressing burden to individuals, availability of services, technology, and personnel, and other stakeholder perspectives. Patient Centered Outcomes Research Institute (PCORI) http://www.pcori.org/what-we-do/pcor/ 13 Quality of life is not frequently measured in drug abuse research • Primary outcomes of treatment studies are abstinence-based • Economic studies focus on financial costs and savings • General health status quality-of-life measures (SF36, SF-12, WHOQOL-BRF) sometimes used for patients entering treatment • IDU-specific quality-of-life measure (IDUQOL) not widely used • Little data on quality of life among prescription drug users 14 Health status versus health utility • Health status measures emphasize rating different domains, e.g. – – – – Physical function Psychological function Social function Impairment • Preference-based utility measures require uncertainty or tradeoff – Societal preferences for cost-effectiveness analyses 15 Changes in health status after 12 months in the NAOMI trial Nosyk B, Guh DP, Sun H, et al. Drug Alcohol Depend 2011;118:259-64 16 Health utility measure: standard gamble 17 Drug abuse research studies using directly-elicited health utilities • Utilities for ASI-defined health states derived from 143 local health planning board members in Massachusetts1 • Utilities for pharmacy-dispensed methadone and buprenorphine treatment health states derived from internet survey of 22 members of the general UK population2 1 2 Daley M, Shepard DS, Bury-Maynard D. Subst Use Misuse 2005;40:375-94. Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al. Health Technology Assessment 2007;11:1-171, iii-iv. 18 Translating health status to health utility: EQ-5D 19 Health utility trajectories in the NAOMI trial Nosyk B, Guh DP, Sun H, et al. Drug Alcohol Depend 2011;118:259-64. 20 Drug abuse research studies in the US reporting indirectly elicited utilities • Utilities measured in a trial of substance use treatment linkage and engagement strategies in a Midwestern city1,2 • Cost-effectiveness of extended buprenorphine-naloxone for opioiddependent youth from the CTN-0010 trial3 1 Pyne JM, French M, McCollister K, Tripathi S, Rapp R, Booth B.. Addiction 2008;103:1320-9. 2 Pyne JM, Tripathi S, French M, McCollister K, Rapp RC, Booth BM.. Addiction 2011;106:507-15. 3 Polsky D, Glick HA, Yang J, Subramaniam GA, Poole SA, Woody GE. Addiction 2010;105:1616-24. 21 Translating utilities into QALYs CABG 1 MI P o s t M I Utility Perfect Health 0.5 0 1 2 Post-CABG A n g i n a 3 4 5 6 7 8 9 10 Years • Life expectancy: 10 years • QALYs = (3.5)(1) + (1)(0.5) + (5)(0.9) + (0.5)(0.2) = 8.6 QALYs M. Roberts, University of Pittsburgh 22 Cost-effectiveness ratio Additional Resources Used ($) Additional Health Benefits Gained (QALYs) 23 Cost-effectiveness misconception #1 “Cost-Effective” = “Cheap” “Cost-Effective” = “Saves Money” 24 Cost-effective ≠ Cost saving 25 Cost-effectiveness is about value for money • Very, very few health interventions save more money than they cost • Cost-effectiveness analysis is about comparative assessment of worth • Investments in health can be compared to evaluate competing claims on scarce resources 26 Cost-effectiveness misconception #2 If an intervention is cost-effective, payers should pay for it 27 Cost-effectiveness depends on the perspective of the analysis • Cost-effectiveness analyses attempt to account for all costs and benefits, regardless of payer or beneficiary • “Cost-effective” from the societal perspective doesn’t mean “budget-neutral” from the payer perspective • Budget impact analysis addresses the question of where the money comes from 28 Cost-effectiveness misconception #3 Cost-effectiveness is the only consideration when making resource allocation decisions 29 Only one of many measures of the appropriateness of health interventions • • • • • Clinical duty Ethical duty Equity / justice Patient preference Economic efficiency 30 Cost-effectiveness vs. cost-benefit? • Cost-benefit analysis (CBA) allows consideration of benefits and costs outside the health care system • CBAs have shown methadone maintenance to be cost-saving considering savings in crime costs, welfare payments, and health care costs and/or increases in earnings1 1 Simoens S, Ludbrook A, Matheson C, Bond C. Drug Alcohol Depend 2006;84:28-39. 31 Cost-benefit issues • CBA is not commonly accepted for evaluating medical treatments; cannot compare results to other health care interventions • Decision makers may not be interested in savings outside the health care system • Requires extrapolation from studies of methadone treatment and heroin use; may not be relevant to other patient populations 32 33 Opioid dependence treatment gap • Estimated population with opioid dependence or abuse in last year1: – Pain relievers: 1,921,000 – Heroin: 359,000 • Many patients are unwilling or unable to attend methadone maintenance clinics – Lack of availability (only 1,521 sites nationwide)2 – Often requires daily visits and directly observed dosing – Stigma • Very limited use of office-base methadone maintenance3 1 SAMHSA, National Survey on Drug Use and Health (NSDUH), 2010 SAMHSA, United States National Survey of Substance Abuse Treatment Services (N-SSATS), 2009 33Gunderson EW, Fiellin DA. CNS drugs 2008;22:99-111 2 34 Buprenorphine cost • Cost has been considered a barrier to adoption – Drug cost is at least 7x higher than methadone, but methadone is very rarely used in the outpatient setting1 • Brand-name buprenorphine lost patent exclusivity in October 20091,2 – Brand-name buprenorphine/naloxone (Suboxone) has no generic competitors – Brand-name buprenorphine (Subutex) has one generic competitor; cost was estimated to be 80% of Subutex cost 1 2 Murray L (ed), Red Book Pharmacy’s Fundamental Reference, 2010 http://www.accessdata.fda.gov/scripts/cder/ob/default.cfm 35 Study aims • To evaluate the cost-effectiveness of long-term officebased buprenorphine treatment compared to no treatment for clinically stable patients – Assume patients are unwilling or unable to engage in methadone maintenance treatment – Health care perspective with patient benefits measured in QALYs • To evaluate the impact of uncertainty about model inputs on cost-effectiveness results – Price of buprenorphine – Duration of treatment – Quality of life on/off buprenorphine 36 All models are wrong, some models are useful 37 Treatment cohort simulation model Enter In Treatment Off Drugs Off Treatment Off Drugs In Treatment On Drugs Off Treatment On Drugs Note: Separate models run for injection drug users (IDUs) and non-IDUs 38 Data from published cohort study • Patients had been followed in an RCT of buprenorphine management strategies and successfully completed 24 weeks on buprenorphine/naloxone (w/ at least 9 weeks abstinence)1 • We used follow-up study data on retention in treatment up to 24 months after completion of the RCT2 • For those not retained in treatment, assumed 89% to be actively using drugs when out of treatment3 • Unit cost data from previous analysis of the same cohort4 • Average weekly cost for IDU and non-IDUs calculated based on patient-level resource utilization 1 Fiellin DA, Pantalon MV, Chawarski MC, Moore BA, Sullivan LE, O'Connor PG, Schottenfeld RS. N Engl J Med 2006;355:365-74. DA, Moore BA, Sullivan LE, Becker WC, Pantalon MV, Chawarski MC, Barry DT, O'Connor PG, Schottenfeld RS. Am J Addict 2008;17:116-20. 3 Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al. Health Technology Assessment 2007;11:1-171, iii-iv. 4 Jones ES, Moore BA, Sindelar JL, O'Connor PG, Schottenfeld RS, Fiellin DA. Drug Alcohol Depend 2009;99:132-40. 2 Fiellin 39 Monthly probability of retention in treatment 100% 90% 80% 70% 60% Probability of 50% Retention 40% 30% 20% 10% 0% 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Months in Treatment 40 Mean (SD) utility weights Base Case1 Sensitivity Analysis2 In treatment, off drugs 0.867 (0.152) 0.856 (0.150) In treatment, on drugs non-IDU 0.683 (0.204) Health State 0.876 (0.100) In treatment, on drugs IDU 0.633 (0.208) Out of treatment, off drugs 0.867 (0.152) Out of treatment, on drugs non-IDU 0.678 (0.207) 0.856 (0.150) 0.806 (0.194) Out of treatment, on drugs IDU 1 2 0.588 (0.212) Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al. Health Technology Assessment 2007;11:1-171, iii-iv. CTN 0010 (NCT00078130), Buprenorphine/Naloxone-Facilitated Rehabilitation for Opioid Dependent Adolescents 41 Mean cost-effectiveness ratios Base case Current drug cost 20% drug cost reduction 50% drug cost reduction $35,100/QALY $30,300/QALY $23,000/QALY 42 Mean cost-effectiveness ratios Current drug cost 20% drug cost reduction 50% drug cost reduction Base case $35,100/QALY $30,300/QALY $23,000/QALY 60-month treatment duration $35,200/QALY $30,300/QALY $23,100/QALY 43 Mean cost-effectiveness ratios Current drug cost 20% drug cost reduction 50% drug cost reduction Base case $35,100/QALY $30,300/QALY $23,000/QALY 60-month treatment duration $35,200/QALY $30,300/QALY $23,100/QALY $138,000/QALY $119,000/QALY $90,600/QALY Sensitivity analysis QOL 44 Cost-effectiveness acceptability curve 45 Value of information • Using the $100,000/QALY threshold – Value of eliminating uncertainty about quality-oflife estimates is $6,400 per person eligible for this office based buprenorphine/naloxone treatment – Value of eliminating uncertainty about nonmedication cost items is <$5 per person eligible for this office-based buprenorphine/naloxone treatment 46 Limitations • Cohort treated at a single site • Drug use out of treatment was not observed, we assume 89% return to drug use based on available data • Ignores 6-month “start-up” costs and benefits • Ignores other costs and benefits – Other medical costs saved or incurred – Deaths avoided 47 Conclusions • Office-based buprenorphine for clinically stable patients is cost-effective compared to no treatment using accepted thresholds for medical treatment in the US • Price reductions have a small effect on costeffectiveness findings • Lack of certainty about quality-of-life weights reduces robustness of findings • Further research about quality of life on and off buprenorphine is necessary 48 Quality of life in prescription and injection opioid dependence: study team • Weill Cornell – Bruce Schackman, PhD (PI); Brandon Aden, MD, MPH; Ann Beeder, MD; Jared Leff, MS; Ashley Eggman, MS • Harvard School of Public Health – Eve Wittenberg, PhD; Adrianna Saada, MPH • UCLA/University of British Columbia – Bohdan Nosyk, PhD; Yih-Ing Hser, PhD • RTI International – Jeremy Bray, PhD • Consultants – David Fiellin MD, Yale; Louise Haynes, MSW, MUSC; Todd Korthuis, MD, MPH OHSU; Don Shepard, PhD, Brandeis 49 Quality of life in prescription and injection opioid dependence: Aim #1 • To create an “off the shelf” list of utility weights for opioid dependence health states with and without social welfare considerations – Develop descriptions of opioid use and treatment and their effects on family members with and without non-health descriptors (stigma, legal involvement, etc.) – Conduct a web-based survey of a representative panel of US residents (community members) to assign utility weights to these health states 50 Health states included in survey Health-related QOL “Extended” QOL Family spillover Active IDU X X X Active Rx user X X X Early-stage treatment, methadone X X X Early-stage treatment, buprenorphine-naloxone X X X Maintenance treatment, methadone X X Maintenance treatment, buprenorphine-naloxone X X Health State Post-treatment X 51 Quality of life in prescription and injection opioid dependence: Aim #2 • To estimate utility weights for patientreported opioid dependence health states using self-reported data from two CTN randomized trials – Determine utility weights (SF-6D) for heroin IDU and prescription opioid-dependent patients on and off treatment with methadone or buprenorphine/naloxone – Determine the effect of non-health problems described in ASI-Lite on these utility weights 52 Quality of life in prescription and injection opioid dependence: Aim #3 • To assess the impact on opioid dependence utility weights of poorly controlled HIV and chronic HCV using self-reported data from the BHIVES cohort – Determine utility weights for heroin IDU and prescription opioid-dependent patients on and off treatment with buprenorphine/naloxone by HIV and HCV status – Compare algorithms that combine off the shelf utility weights from Aim 1 and the literature to BHIVES results 53 Impact of illicit drug use and HCV status on health utility by HIV status in the WIHS cohort Aden B, Nosyk B, Schackman BR, Wittenberg E. 34th Annual Meeting of the Society for Medical Decision Making. October 19, 2012. Phoenix, AZ. 54 CTN-0051 comparative effectiveness trial • Extended-Release Naltrexone vs. Buprenorphine for Opioid Treatment – To assess the comparative effectiveness of extended release injectable naltrexone (XR-NT) versus buprenorphine-naloxone (BUP-NX) – Duration of treatment: 6 months • XR-NT requires complete detoxification, BUPNX requires sufficient withdrawal for induction • XR-NT costs more than BUP-NX 55 Economic analysis design issues • How collect quality-of-life information? – Which questionnaire? How frequently? – Consider non-health benefits? • Which economic outcome? – Cost/opioid-free day? – Cost/QALY? – Cost-benefit? • Model treatment outcomes beyond 6 months? 56