Ch 4: Synaptic Transmission
advertisement

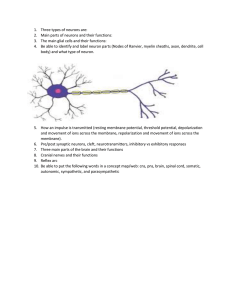
This chapter is about introducing the function of neurons ◦ How they conduct & transmit electrochemical signals through the nervous system Function of neurons centers around the membrane potential ◦ The difference in electrical charge between the inside & outside of the cell Can measure membrane potential using a microelectrode ◦ Measure the charge inside the cell & the charge outside. A neuron’s resting potential is -70mV ◦ Meaning, the charge inside the cell is 70mV less than the charge outside ◦ Inside < Outside Because this value is beyond 0, it is said to be polarized So at rest, neurons are polarized. It is polarized due to the arrangement of ions ◦ The salts in neural tissues separate into + and – charged particles called ions 4 main ions are responsible: 1. K+ (potassium) 2. Na+ (sodium) 3. Cl(chloride) 4. - charged proteins The ratio of – to + ions is greater inside a neuron than out, so you have a more – charge inside ◦ Again, why the neuron’s resting potential is polarized 2 things cause this imbalance & 2 things try to equalize (homogenize) Equalizers (homogenizers) 1. Random motion 2. Electrostatic pressure Cause imbalance 1. Passive flow 2. Active transport Random Motion Ions are in constant random motion Tend to be evenly distributed because they move down their concentration gradient 1. ◦ 2. Move from areas of higher concentration to lower concentration Electrostatic Pressure Ions with the same charge will repel each other Opposite charges attract Concentrations of Na+ and Cl- are greater outside the neuron (extracellularly) K+ concentration is greater inside the cell (intracellularly) Negatively charged proteins generally stay inside the neuron Passive Flow 1. Does not require energy The membrane is selectively permeable to the different ions ◦ ◦ K+ and Cl- ions easily pass through the membrane Na+ ions have difficulty passing through Ions passively flow across the membrane via ion channels ◦ Special pores in the membrane Active transport 2. ◦ Needs energy to power the pumps Active transport 2. Requires energy to power the pumps that transport the ions Discovered by Hodgkin & Huxley ◦ ◦ Nobel prize winning research Why is there high Na+ and Cl- outside and high K+ inside? Why are they not passively flowing down their concentration gradients & reaching equilibrium? Calculated the electrostatic pressure (mV) that would be necessary to counteract the passive flow down the concentration gradient (aka keep the concentrations uneven across the membrane) & how this differed from the actual resting potential Discovered that there are active pumps that counteract the passive flow of ions in & out of the cell (specifically for Na+ and K+) Sodium-potassium pumps ◦ Actively (using energy) pumps Na+ out & K+ in ◦ 3 Na+ ions out for every 2 K+ ions pumped in Other types of active transporters also exist *Summary Table 4.1 (pg. 79)* Remember: At a synapse, the presynaptic neuron releases NT that bind with receptors on the postsynaptic neuron, to transmit the signal from one neuron to the next When the NT bind with the postsynaptic neuron, they have either of 2 effects 1. Depolarize the membrane ◦ ◦ 2. ◦ ◦ Decrease the resting potential **this means become less negative, aka approach zero** Hyperpolarize the membrane Increase the resting potential ** make it more negative; further from zero** hyperpolarize depolarize Postsynaptic depolarizations: ◦ Excitatory postsynaptic potentials ◦ EPSPs ◦ Increase the likelihood that the neuron will fire Postsynaptic hyperpolarizations: ◦ Inhibitory postsynaptic potentials ◦ IPSPs ◦ Decrease the likelihood that the neuron will fire Graded responses ◦ Weak signals cause small PSPs; strong signals cause large PSPs Travel passively ◦ Very rapid (practically instantaneous) Like a cable ◦ Deteriorate over distance Lose amplitude as they go along Fade out Like sound Individual PSPs have almost no effect on getting a neuron to fire However, neurons can have thousands of synapses on them & combining the PSPs from all of those can initiate firing ◦ Called integration ◦ Add all the EPSPs + IPSPs ◦ Remember: PSPs are graded & have different strengths ExcitatoryPSPs increase the likelihood of firing & InhibitoryPSPs decrease the likelihood Neurons integrates PSPs in 2 ways 1. Over space: spatial summation ◦ ◦ ◦ EPSP + EPSP = big EPSP EPSP + IPSP = 0 (cancel each other out; assuming of equal strength) IPSP + IPSP = big IPSP Over time: temporal summation 2. ◦ 2 PSPs in rapid succession coming from the same synapse can produce a larger PSP If the sum of the PSPs reaching the axon hillock area at any one time is enough to reach the threshold of excitation, an action potential is generated ◦ The threshold is -65mV So the resting membrane potential must be depolarized 5mV for the neuron to fire Action potential ◦ Massive, 1ms reversal of the membrane potential -70 to +50mV ◦ Not graded; they are all-or-nothing responses Either fire at full force or don’t fire at all APs are generated & conducted via voltageactivated ion channels When the threshold of excitation is hit, the voltage-activated Na+ channels open & Na+ rushes in The Na+ influx causes the membrane potential to spike to +50mV This triggers the voltage-gated K+ channels to open & K+ flows out After 1ms, Na+ channels close End of rising phase Beginning of repolarizing phase ◦ K+ continues to flow out until the cell has been repolarized; then the K+ channels close Cell returns to baseline resting membrane potential For about 1-2ms after the AP, it is impossible to fire another one ◦ Absolute refractory period Followed by a period during which another AP can be fired, but it requires higher than normal levels of stimulation ◦ Relative refractory period Afterwards, the neuron returns to baseline & another AP can be fired as usual Ions can pass through the membrane at the nodes of Ranvier between myelin segments APs move instantly through myelinated segments to the next node, where concentrated Na+ channels allow the signal to be “recharged” and sent to the next Overall, this allows APs to be conducted much faster than in unmyelinated axons, because the AP “jumps” from node to node and effectively “skips” the lengths covered in myelin (saltatory conduction) Speed of conduction is faster with myelin Faster in thicker axons Ex: mammalian motor neurons are thick & myelinated & can conduct signals at around 224 mph!! Different types of synapses based on the location of the connection on each neuron ◦ Axodendritic “Normal” synapses Terminal button of axon on Neuron1 to dendritic spine of Neuron2 ◦ Axosomatic Axon of N1 to soma of N2 ◦ Dendrodendritic ◦ Axoaxonic 2 categories of NTs ◦ Large: Neuropeptides ◦ Small: Made in terminal buttons & stored in vesicles NTs are released via exocytosis At rest, NTs are in vesicles near membrane of presynaptic neurons When an AP reaches the terminal button, voltage-activated Ca2+ channels open & Ca2+ rushes in ◦ Ca2+ causes the vesicles to fuse with the membrane & release contents into the synaptic cleft NTs released from the presynaptic neuron cross the cleft & bind to receptors on the postsynaptic neuron Receptors contain binding sites for only certain NTs Any molecule that binds is a ligand There are often multiple receptors that allow one kind of NT to bind: receptor subtypes ◦ Different subtypes can cause different reactions There are 2 general types of receptors 1. Ionotropic ◦ ◦ NT binds & ion channel opens & ions flow through Immediate reaction Metabotropic 2. ◦ ◦ ◦ NT binds & initiates a G-protein to trigger a second messenger, which moves within the cell to create a reaction Slow, longer lasting effects More abundant A special type of metabotropic receptor Located on the presynaptic neuron & bind with NTs from its own neuron Function to monitor the # of NTs in the synapse ◦ If too few, signal to release more ◦ Too many, signal to slow/stop release In order to allow the synapses to be available to signal again, the extra NT in the synaptic cleft need to be “cleaned up” by: Reuptake ◦ Most of the extra NT are quickly taken back into the presynaptic neuron by transporters to be repackaged in vesicles for future release Enzymatic degradation ◦ NTs in the cleft are broken down by enzymes ◦ Ex: acetylcholine broken down by acetylcholinesterase ◦ Even these pieces are taken back into the neuron & recycled Unique signal transmission alternative to traditional synapses Called electrical synapses Narrow gaps between neurons connected by fine tubes called connexins that let electrical signals pass Very fast & allow communication in both directions Not yet fully understood in mammalian systems Amino Acid NTs Monoamine NTs Acetylecholine Unconventional/Misc. NTs Neuropeptides AAs are the building blocks of proteins Glutamate ◦ Most common excitatory NT in the CNS Aspartate Glycine GABA ◦ Most common inhibitory NT 2 groups with a total of 4 NTs in this class Catecholamines: 1. Dopamine (DA) ◦ Made from tyrosine/L-Dopa Norepinephrine (NE) 2. ◦ Made from dopamine Epinephrine 3. ◦ Made from NE Indolamines: Serotonin (5-HT) 4. ◦ Made from tryptophan Functions at neuromuscular junctions, in ANS & CNS Extra is mostly broken down in the synapse; by acetylcholinesterase Receptors for Ach are said to be cholinergic Act differently than traditional NTs Nitric oxide & carbon monoxide ◦ Gases that diffuse across the membrane, across the extracellular fluid & across the membrane of the next neuron Endocannabinoids ◦ Essentially, the brain’s natural version of THC (main active chemical in marijuana) ◦ Ex: annandimide Don’t worry about the specific types Just know that they are another type of NT Generally large NTs Pharmaceutical drugs generally affect synaptic in 2 ways ◦ Agonists facilitate the effects of a NT Can bind to a receptor & activate it like the NT would ◦ Antagonists inhibit Can bind to a receptor & block it so NTs cannot bind Acetylcholine has 2 types of receptors 1. Nicotinic ◦ ◦ ◦ ◦ ◦ 2. ◦ ◦ ◦ Many in the PNS between motor neurons & muscle fibers Ionotropic Nicotine: agonist Curare: antagonist (causes paralysis) Botox: antagonist Muscarinic Many located in the ANS Metabotropic Atropine: antagonist, receptor blocker Endogenous ◦ Compounds naturally made within the body ◦ Ex: enkephalins & endorphins The body’s endogenous opioids An exogenous opioid is morphine Opioids are analgesics (pain relievers)