Approach to anemia f..
advertisement

Approach to anemia
• Abdul-Kareem Al-Momen, MD, FRCPC
• KSU-MED 341
• 17-04-2011 (13-05-1432)
Definition:
Anemia is defined as a reduction in one or more
of the major RBC measurements:
hemoglobin concentration, hematocrit, or
RBC count to a degree lower than normal values
for the tested population :newborn, childhood,
adulthood (males & females), and sea level
Hb (gm/L)
PCV
(Hct)%
Newborn 200 +/- 20
Chld. 110 +/- 10 60 +/- 20
33 +/- 3
Adult:
48 +/- 5
Male 160 +/- 20
42 +/- 5
Female 14 +/- 20
Sea Level:
47 %
Jeddah
150 g/L
58 %
Hi.Alt.:Albaha
190 G/l
Anemia?
Production?
Destruction?
The key test is the reticulocytic count
The reticulocyte count
• Increased reticulocytes (greater than 2-3% or
100,000/mm3 total) are seen in blood loss and hemolytic
processes.
The reticulocyte count
• To be useful the reticulocyte count must be adjusted for
the patient's hematocrit, because when hematocrit is
low, reticulocytes are released earlier (faster) from the
marrow so one can adjust for this phenomenon as
follows:
• Corrected retic. = Patients retic. x (Patients Hct/45)
Example: Hb 70 g/L, PCV (Hct) = 20,
Retics.= 16 %
Corrected Retics.= 16 X 20/45 = 7
The reticulocyte count
• Reticulocyte Production index (RPI) = corrected retic.
count/Maturation time
(Maturation time = 1 for Hct=45%, 1.5 for 35%, 2 for
25%, and 2.5 for 15%.)
Example: PCV = 20 %, Retics.= 16, Corrected Retics=7
RPI = 7/2 = 3.5
• Absolute reticulocyte count = retic x RBC number.
Causes of Anemia (kinetic
approach)
Decreased erythrocyte production
Bone marrow suppression
Bone marrow infiltration
Nutritional deficiencies
Decreased erythropoietin production
Inadequate marrow response to erythropoietin
Causes of Anemia
Blood loss
•Hemorrhage :
Bleeding tendencies,
Menorrhagea,
Anticoagulation
Liver disease
Hemolysis:
Autoimmune,
None-immune, (MAHA,
RBC defects, Hypersplenism)
Dilutional Anemia
• Dilutional- A patient's plasma
volume increases with
pregnancy,(Splenomegally), laying
down possibly responsible for as
much as a 3-6% drop in the
hematocrit in the first two days of
hospitalization.
Morphological Approach
(big versus small)
First, measure the size of the RBCs:
MCV (femtoliters) = 10 x HCT(percent) ÷ RBC (millions/µL)
High MCV
MCV>115
• B12, Folate
• Drugs that impair DNA synthesis (AZT,
chemo., azathioprine)
• MDS
Normal MCV
Normocytic normocytic
• Anemia of chronic disease
• Mixed deficiencies
• Renal failure
• Endocrinopaties
Low MCV
Microcytic
• Iron deficiency
• Thalassemia trait
• Anemia of chronic disease (30-40%)
• Sideroblastic anemias
• Lead poisoning
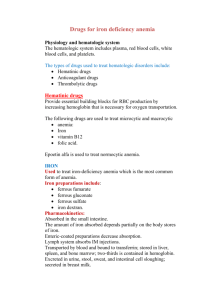
Iron deficiency anemia
• Iron deficiency is a common form of
malnutrition that affects more than 2 billion
people globally.
Iron Deficiency Anemia
– Smear:
• hypochromic and microcytic (low MCV) RBCs,
usually not seen unless Hct 30%
• platelet count is often elevated
– Ferritin: a measure of total body iron stores, but
also an acute phase reactant
• <15g/l = Fe deficiency, 150 g/l = Not Fe
deficiency
15-150 g/l = ?
Iron Deficiency Anemia
– Low Iron Saturation (Fe/TIBC ratio)
• Fe (not reliable)
• TIBC
• Fe/TIBC (% saturation) 15%
– BM bx: absent Fe stores
• Gold standard
– Therapeutic Trial of Oral Iron
Increased iron requirements
•Blood loss
•Gastrointestinal disorders (esophageal varices, hemorrhoids)
•Extensive and prolonged menstruation
•Pulmonary (hemoptysis, pulmonary hemosiderosis), urologic, or nasal disorders
•Dialysis
•Hookworm infestation
•Intravascular hemolysis with hemoglobinuria
•Paroxysmal nocturnal hemoglobinuria
•Cardiac valve prostheses
•Rapid growth in body size between 2 and 36 months of age
•Pregnancy and lactation
Inadequate iron supply
• Poor nutritional intake in children (not a common independent
mechanism in adults but often a contributing factor)
• Malabsorption
• Gastric bypass surgery for ulcers or obesity
• Achlorhydria from gastritis or drug therapy
• Severe malabsorption (for example, celiac disease
[nontropical sprue])
• Abnormal transferrin function
• Congenital atransferrinemia
• Autoantibodies to transferrin receptors
Oral iron failure?
•
•
•
•
•
Incorrect diagnosis (eg, thalassemia)
anemia of chronic disease?
Patient is not taking the medication
Not absorbed (enteric coated?)
Rapid iron loss?
Intravenous Iron Therapy
• Iron sacharate (Ferrosac), 200 mg in
100-250 cc normal saline IV over one
hour daily to the total dose required
•(Weight {kg} x Hb deficit {target Hbcurrent Hb] x 4).
• Ferric gluconate (Ferrlecit ) in patients
on renal dialysis. The number of allergic
reactions is lower than that from iron
dextran
Utility of supraphysiologic
doses of erythropoietin in the
setting of inflammatory block.
B12/Folate Deficiency
• Etiology:
– Anemia-- Vitamin B12 and folate are needed
for DNA synthesis deoxyuridate to thymidylate
, including RBC precursors
– Deficiency
• B12 - Dietary intake, acid-pepsin in the
stomach, pancreatic proteases, gastric
secretion of intrinsic factor, an ileum with Cbl-IF
receptors (fish tapeworm)
• Folate-- Poor dietary intake EtOH,
malabsorption, increased demand (pregnancy,
hemolytic anemias), inhibitors of DHFR
B12/Folate Deficiency (2)
• Dx:
– Smear: Macrocytic (High MCV) RBCs, +/- hypersegmented
neutrophils, +/- modest neutropenia, but…
– the diagnosis of B12 def. was made in patients in whom only
29 percent had anemia, and only 36 percent had a MCV
greater than 100 fL (Pruthi RK, Tefferi A, Mayo Clin Proc
1994 Feb;69(2):144-50)
– B12
• Low serum B12, elevated serum methylmalonic acid
levels
• Anti-IF Abs, Schilling test (?), PA accounts for 75%
– Folate
• Serum folate level-- can normalize with a single good
meal
B12/Folate Deficiency (3)
• Tx:
– B12 deficiency: B12 1 mg/month IM, or 1-2
mg/day po
– Folate deficiency: Improved diet, folate 1
mg/day
– Monitor for a response to therapy.
– Pernicious Anemia – monitor for gi cancers.
Cobalamin deficiency and neurological problems
• Subacute combined degeneration of the dorsal and lateral
spinal columns.
• Well known study of B12 deficiency in the nursing home
population (Carmel R Karnaze DS, JAMA 253:1284, 1985)
• Vitamin B-12 deficiency is present in up to 15% of the elderly
population as documented by elevated methylmalonic acid in
combination with low or low-normal vitamin B-12
concentrations.
• Is oral B12 good enough?
• Association between nitrous oxide anesthesia and
development of neurological symptoms responsive to B12 in
patients with subclinical cobalamin deficiency (methionine?).
Diagnostic tests for Vit. B12 Deficiency
Test
Serum methylmalonic acid and
serum homocysteine
MCV>115, smear, CBC
Antibodies to IF and Parietal cells
Schilling test
Spot urine for homocysteine
Sideroblastic Anemias
• Heterogenous grouping of anemias defined by
presence of ringed sideroblasts in the BM
• Etiologies:
– Hereditary (rare), type of porphyria
– Myelodysplasia
– EtOH
– Drugs (INH, Chloramphenicol)
• Tx:
– Trial of pyridoxine for hereditary or INH induced
SA
Hemolytic Anemias
Hemolytic anemias are either acquired or congenital. The laboratory
signs of hemolytic anemias include:
1. Increased LDH (LDH1) - sensitive but not specific.
2. Increased indirect bilirubin - sensitive but not specific*.
3. Increased reticulocyte count - specific but not sensitive
4. Decreased haptoglobin - specific but not sensitive.
5. Urine hemosiderin - specific but not sensitive.
*The indirect bilirubin is proportional to the hematocrit, so with a
hematocrit of 45% the upper limit of normal is 1.00 mg/dl and with a
hematocrit of 22.5% the upper limit of normal for the indirect bilirubin is
0.5mg/dl. Since tests for hemolysis suffer from a lack of sensitivity and
specificity, one needs a high index of suspicion for this type of anemia.
Hereditary anemias
• 1- RBC memberane defects :e.g.Heriditary
Spherocytosis
• 2-Reduced Globin Chains:e.g.
α
thalassemia ( reduced α chain ) ,&
β thalassemia
( reduced β chain)
• 3-Abnormal amino-acid sequence e.g. Sickle Cell
Anemia
• 3-Enzymopathies :e.g G6PD deficiency
Hemoglobinopathies
• Sickle cell disease/anemia
• Thalassemias
Sickle Cell Anemia / Disease
• Hb SS due to replacement of glutamic acid by
valine at position 6 on the β globin chain
• HbS molecule are less soluble ,tend to form
crystals and fibers,which leads to RBC
deformity ,sickling ,vaso-occlusion &
hemolysis
Complications of Sickle Cell Disease
• 1- Vaso-occlusion ,with recurrent painful
episodes (mild-moderate-severe )
• Acute chest syndrome
• Recurrent infection (URT & chest )
• Splenic sequestration
• Priapism
• Thrombo-embolic disease (CVA,PE,DVT)
SCD Complication: (cont.)
•
•
•
•
Avascular necrosis (head of femur & humerus)
Tendency for Osteo-myelitis ( salmonella)
Leg ulcers
Gall stones
Presipitators of Vaso-Occlusive Episodes
• 1-Hypoxia : - low atmospheric oxygen , Lung
diseases ,heart diseases
• 2-Increased blood viscosity: increased Hb/Hct
,dehydration, infection ,general anesthesia
• 3-Extreme hot/cold weather
• 4-Unknown causes
Management of SCD
•
•
•
•
•
•
•
Vaccination
Antibiotic prophylaxis
Avoidance of hypoxia and extreme weathers
Increase fluid intake
Treatment of acute episodes
Exchange transfusion /transfusion
Prevention: premarital screening & genetic
counseling
β Thalassemia
• 2 β genes on chromosome # 11 give 2 β globin
chains.
• ββ = normal
• -β = β thalassemia trait (hypochromic ,
microcytic anemia, asymptomatic , confused
with iron deficiency anemia )
Thalassemia Major (Homozygous β
Thalassemia )
•
•
•
•
•
•
•
•
No β chains
Severe intramedullary hemolysis
Severe hemolytic anemia
Jaundice + Pallor
Bone marrow expansion
Hepatosplenomegaly
Delayed puperty
Iron overload ( absorption + hemolysis )
H. Spherocytosis
•
•
•
•
•
•
•
RBC = Spheres (not biconcave )_
Reduced survival (hemolytic anemia )
Jaundice,
Splenomegaly
Gall stones
Reticulocytosis
Increased direct billirubin
Treatment
• 1-Folic acid
• 2-Splenectomy after vaccination against
S.Pneomoniae & H.Influenzaeز
• Malaria avoidance / prophylaxis
Enzymopathies : G6PD Deficiency
• G6PD is essential for the production of the
anti-oxidant Glutathione
• Acute hemolysis upon exposure to oxidative
stress food (fava beans),drugs (e.g.sulfa
derivatives ),chemicals or infection
• X- linked
Approach to anemia:
• History: Onset (acute versus chronic),Age at
onset, character, associations (splenomegally,
growth retardation, painful episodes,
transfusions, dietary habits, family history,
consanguinity, involvement of other systems,
drug history : ASA, anticoagulantsetc )
• Symptoms (fatigue, exercise intolerance,
headache, palpitation, lack of concentration, poor
appetite,
• Adaptation
Approach to anemia:
• Signs (physical exam):
Pallor, dry skin, smooth tongue, thin hair, hair
loss, splenomegally, neuropathy,
• Signs of systemic diseases ( renal, hepatic,
musculoskeletal, cancer, infection, etc )
Approach to anemia:
• Laboratory: RBC, Hb, Hct (PCV), MCV, MCH,
MCHC, RDW, Reticulocytes, WBC, Platelets,
blood filnm ( smear)
• Fe, Transferrin, ferritin, B12, folates (RBC)
• ESR, ANA, RF, BUN, Cr,
• Hb electrophoresis (Hb A, A2, S, F, )
•Good Luck