Bahamas-Walker
advertisement

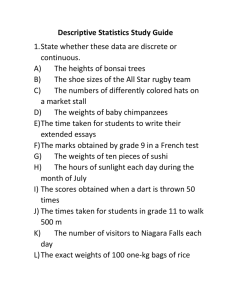
What Bahamas Can Learn from Global Experience with Health Policy? Nassau June 21, 2007 Michael Walker Senior Fellow The Fraser Institute 1 Plan of Discussion Why should you listen to what I have to say? Health Care Policy in Context Myth Versus Reality about the Canadian Model and its comparative performance Alternative futures for Bahamian Policy 2 Why Should You listen to me? Bahamians -- like many Americans-- are apparently attracted by the Canadian health care model I have been researching the Canadian model since 1978 and public policy for nearly 40 years For 17 years my colleagues and I have been measuring the extent of rationing in the Canadian system and its comparative performance Recently, the Canadian Supreme Court agreed with our research in finding that the combination of the actual performance of the Canadian health care system and the prohibition of private care in Canada violated the constitutional rights of Canadian citizens. 3 Background to the Health Care Debate - General Issues? Wealthy people and nations tend to be Healthy Policy can increase the health care access of the less wealthy by taxing the income of the wealthy Human and financial capital try to avoid taxes and the competition for both kinds of capital is global Nations which attempt to solve the health problem of the less wealthy by taxing human and financial capital will attract less of both Therefore, policy which pursues gains in population health without careful attention to the growth and per capita income effects of the methods chosen may produce short term gains at 4 the expense of larger long term loses Background to the Health Care Debate – Specific Issues II? Health care will become the largest non-traded sector of the Bahamian Economy It will be the source of the most interesting jobs and the highest tech employment in the economy. The policies you set there will have a huge impact on the Economic Policy setting overall and your economic success as: – – – – -Tax Policy is affected by the health tax -Labour policy is affected by GBE growth -The structure of your politics is affected by PS unions -The technological sophistication of you country is affected by politicization of capital allocation 5 How has Overall Bahamian Policy Been Doing? Fraser Institute in conjunction with Institutes in 70 countries has been measuring policy in 130 countries since the 1970s The measures score 38 policies 1 to 10 and rank the countries The following slides show how Bahamas performance has changed over time 6 Bahamas Versus the Top Ten Canada 20 Hong Kong 40 Ireland Iceland Luxembourg New Zealand 60 Singapore 80 Switzerland United Kingdom 100 United States 19 75 19 80 19 85 19 90 19 95 20 00 20 01 20 02 20 03 20 04 Rank 0 Bahamas 7 Source: The Fraser Institute. Bahamas Competitive Policy Rank 0 Regulation 20 Trade 60 Tarrif Rate 80 Money Policy 100 Property Rights RofL 120 Size of Government 19 75 19 80 19 85 19 90 19 95 20 00 20 01 20 02 20 03 20 04 Rank 40 8 Source: The Fraser Institute. The Quality of Policy Really Matters 9 Per Capita Income and Economic Policy Quality Quartile GDP Per Capita (ppp), 2003 $25,000 $20,000 $15,000 $10,000 $5,000 $0 Lowest Policy Quartile 3rd Quartile 2nd Quartile Highest Quartile Worst Policy…………… Best Policy Sources: The Fraser Institute; The World Bank, World Development Indicators CD-ROM, 2005. 10 GDP Per Capita % Growth, 1994-2003 Growth in Real GDP Per Capita and Policy Quality Quartile 2.5 2.0 1.5 1.0 0.5 0.0 -0.5 Lowest Quartile 3rd Quartile 2nd Quartile Highest Quartile Worst Policy …………….Best Policy Sources: The Fraser Institute; The World Bank, World Development Indicators11 CD-ROM, 2005. Human Poverty Index and Policy Quality Quartile Human Poverty Index 40 35 30 25 20 15 10 5 0 Lowest Quartile 3rd Quartile 2nd Quartile Highest Quartile Worst Policy …………..Best Policy Sources: The Fraser Institute; United Nations Development Programmme, Human Development Indicators 2005, available at http://hdr.undp.org/statistics/data/index_indicators.cfm. 12 United Nations Human Development Index Human Development Index and Policy Quality Quartiles 1.0 0.9 0.8 0.7 0.6 0.5 0.4 Lowest Quartile 3rd Quartile 2nd Quartile Highest Quartile Worst Policy …………Best Policy Sources: The Fraser Institute; United Nations Development Programmme, Human Development Indicators 2005, available at http://hdr.undp.org/. 13 Years Life Expectancy at Birth and Policy Quality Quartiles 80 75 70 65 60 55 50 45 40 Lowest Quartile 3rd Quartile 2nd Quartile Highest Quartile Worst Policy ………… Best Policy Sources: The Fraser Institute; The World Bank, World Development Indicators CD- ROM, 2005. 14 Infant Mortality and Policy Quartile Per 1,000 live births, 2003 80 60 40 20 0 Lowest Quartile 3rd Quartile 2nd Quartile Highest Quartile Worst Policy………..….Best Policy Sources: The Fraser Institute; The World Bank, World Development Indicators CD-ROM, 2005. 15 % of Population Using Improved Water Sources and Policy Quartile 100 Percentage 90 80 70 60 50 Lowest Quartile 3rd Quartile 2nd Quartile Highest Quartile Worst Policy ……………Best Policy Sources: The Fraser Institute; The World Bank, World Development Indicators CD-ROM, 2005. 16 As is clear from this global scan… The Quality of Policy Really Matters For Bahamians And We can se the effects of Bahamas’ policy decline 17 Bahamian Per Capita Income Rank declining compared to the World 0 5 Rank 10 15 20 25 30 35 40 1970 1975 1980 1985 1990 1995 2000 18 Source: The Fraser Institute. Bahamian Growth Rank Declining Growth Rate Rank compared to rest of world 0 -10 -20 -30 -40 -50 1970-85 Average Per Capita Growth 1.27% 1985-2000 Average Per Capita Growth 0.06% -60 -70 -80 -90 19 So, The decline in Policy Quality is showing up in lower average incomes and lower growth rates. Apart from any other development, this is going to reduce the comparative health status of Bahamians 20 The Canadian Case The only country in the OECD that has an exclusively public sector single payer for heath care is Canada The Canadian system should be carefully studied before launching a National Health Insurance plan in The Bahamas The following is a careful set of measurements of the Canadian system. These measurements caused the Canadian Supreme Court to rule that the provisions of the sort of System we have were injurious to the health of Canadians and violated their Constitutional Rights. 21 Ic e Sw Ca lan i tz n a d e d A rla a us n t d N rali o a N F rwa et ra y he n r c N Ge lan e ew r d m s Ze an a y A lan us d G tri r a B ee el ce Po giu D rtu m en g O m al EC a D Irel rk A an ve d r K ag e Sw ore ed a H L C u x un en ze e g U ch mb ary ni R o te e u d pu rg Ki b ng li c Fi d o nl m Po and la Sl Sp n d ov ai ak R Ita n ep l ub y Ja l ic pa n Percent of GDP Age-adjusted Health Spending in the NHI OECD Nations 2003 14 12 10 8 6 4 2 0 Source: OECD (2006) Calculations by Authors 22 99 04 05 06 - 07 f 06 f 05 04 - 20 03 - 20 03 02 02 - 20 01 - 20 01 00 00 - 20 99 - 19 98 - 19 98 97 97 - 19 20 96 96 - 19 95 - 19 95 94 94 - 19 20 93 93 - 19 92 - 19 92 91 91 - 19 90 - 19 $1997 Per Capita Inflation Adjusted Provincial/Territorial Spending Per Person $3,000 Canada $2,600 Ontario $2,200 $1,800 $1,400 $1,000 Source: CIHI (2006) 23 Health Results: Getting What We Pay For? 24 Health Results: Waiting Times 25 Median Wait by Province, 2006 BC 7.4 AB 11.9 7.8 8.5 SK 8.4 MB 7.7 20.1 10.3 GP to Specialist ON 7.4 QC 7.5 Specialist to Treatment 8.3 10.2 NB 11.1 20.8 NS 10.9 PE 11.8 NL 12.4 Canada 11.3 14.0 8.1 8.8 0.0 4.0 9.0 8.0 12.0 16.0 Weeks 20.0 24.0 28.0 26 32.0 Median Wait by Specialty, 2006 15.3 Plastic Surgery Gynaecology 20.1 6.6 7.7 15.4 Ophthalmology Otolaryngology 6.6 4.4 General Surg. 10.6 5.7 21.0 Neurosurgery 3.0 24.2 5.0 Urology Internal Med. 10.7 16.2 Orthopaedic Surg. Cardio. Surg. 11.8 6.4 4.8 5.1 GP to Specialist 6.7 Specialist to Treatment Radiation Onc. 1.5 3.4 Medical Onc. 2.8 2.1 8.8 Overall Weeks 0.0 4.0 9.0 8.0 12.0 16.0 20.0 24.0 28.0 32.0 36.0 27 40.0 Waiting For Care – 2006 v. 1993 Waiting Time Between Referral by GP and Treatment, by Province, 1993 and 2006 35.0 1993 31.9 28.5 30.0 2006 25.8 25.0 22.2 Weeks 19.3 18.0 20.0 16.3 10.4 10.5 9.8 10.5 12.3 11.5 10.6 9.1 10.0 17.8 17.1 14.9 15.0 20.5 18.5 9.3 7.3 5.0 0.0 BC AB SK MB ON QC NB NS PE NL CAN 28 Actual Wait Time v. Reasonable Actual versus Reasonable Waits Between Appointment with Specialist and Treatment, Canada, 1994 through 2006 10 6 4 Actual Reasonable 2 20 06 20 05 20 04 20 03 -0 2 20 01 -0 1 20 00 19 99 19 98 19 97 19 96 19 95 0 19 94 Weeks 8 29 Wait Times for Diagnostic Technology 14 MRI CT Ultrasound 12 8 6 4 2 20 06 20 05 20 04 20 03 02 20 01 - 01 20 00 - 19 99 19 98 19 97 19 96 19 95 0 19 94 Weeks 10 30 Diagnostic Wait Times in 2006 12 Ontario Canada Wait Time (Weeks) 10 8 6 4 2 0 CT M RI Ultrasound 31 Canadians Wait Longer Than Others 90% 81% Australia Canada Germany New Zealand United Kingdom United States 80% 69% 66% Percent of Respondents 70% 61% 60% 47% 50% 36% 36% 40% 30% 23% 15% 20% 10% 10% 13% 3% 0% Sicker Adults: Ability to get an appointment to see a doctor same day or next day Sicker Adults: Wait 6 days or more or never get an appointment to see a doctor 32 Source: Schoen et al. (2005 ) Canadians Wait Longer Than Others 60% Percent of Respondents 50% Australia Canada Germany New Zealand United Kingdom United States 60% 57% 46% 40% 40% 27% 30% 22% 23% 20% 17% 20% 11% 10% 11% 10% 0% Sicker Adults: Wait less than 1 week for specialist appointment Sicker Adults: Wait more than 4 weeks for appointment with a specialist 33 Source: Schoen et al. (2005) Canadians Wait Longer Than Others 60% 53% 59% 48% Percent of Respondents 50% Australia Canada Germany New Zealand United Kingdom United States 41% 40% 32% 33% 25% 30% 20% 19% 20% 15% 6% 8% 10% 0% Sicker Adults: Wait less than 1 month for elective Sicker Adults: Wait 4 months or more for elective surgery surgery 34 Source: Schoen et al. (2005) Health Results: Access to Doctors & Technology 35 Doctors in the OECD Iceland Greece Czech Republic Netherlands Slovakia Belgium Italy Switzerland Norway Austria France Ireland Hungary Portugal Denmark OECD Average Sweden Australia Germany Spain Luxembourg Poland New Zealand Korea Canada Finland United Kingdom Japan (2002) Turkey 0.0 24th 0.5 1.0 1.5 2.0 2.5 3.0 3.5 Doctors per 1000 population (Age Adjusted, 2003) 4.0 4.5 36 Source: OECD (2006) Calculations by Authors MRI Machines in the OECD Japan (2002): 29.9 MRI Machines Per Million Population (Age Adjusted, 2003) 20 15 10 13th 5 0 ) l y y a a a n c e d y d c d rg aly rk ge d ria ai ium an ad a nd dom rali uga rke bli nc gar bli 0 02 la n t ma ra an ore lan s t lan ou I p l e S e lg rm a n e al ng b K e r Au in s t ort Tu e pu Fra un pu (2 Po n ve u Ic e F em C e i A B H Re ce Z ti z P A R D D K G e x w w d h 37OECD (2006) u ak re Source: S c L e Ne ite EC v G z o O C Calculations by Authors Un Sl xe m b Be ou lg rg i Au um s Ic tri el a O EC an d D Ita A Sw v ly G it z era re e g e c rla e e nd ( De 20 0 nm 2) N a Cz e w Fin rk ec Ze lan h al d Re a n p d G ub er lic m Po an rtu y ga Sl S ov p l ak Ca ain Re na pu da b Fr lic an Un Tu ce rk ite P d o ey Ki la ng nd Hu do ng m ar y Lu CT Scanners Per Million Population (Age Adjusted, 2003) CT Scanners in the OECD Japan (2002): 78.4 30 15 Korea: 49.4 25 20 17th 10 5 0 Source: OECD (2006) Calculations by Authors 38 nc e K or e N Fi n a ew la Ze nd al an d Lu Gre xe ec m e bo u C rg an ad O I EC ce a D lan A d ve r B ag e el gi u Sl ov P m ak ol a n C ze Rep d ch u Re bl ic pu H bli c un g Po ary rt ug U a ni te Sp l d Ki ain ng do Tu m rk ey Fr a Mammographs Per Million Population (Age Adjusted, 2003) Mammographs in the OECD 40 30 7th 20 10 0 Source: OECD (2006) Calculations by Authors 39 Ko r ak Ja e a R p Sw ep a n it z ubl e r ic la Ic nd el Cz ec Be and h lg Re iu pu m O EC P blic D ola A nd ve G rag Lu er e xe ma m ny bo u Au rg st r Sp ia Au a s t in Po rali rtu a Hu ga ng l a Tu r y rk Fr ey a Ne C nc w an e Ze ad al a a Fi nd nl an d Sl ov Lithotripters Per Million Population (Age Adjusted, 2003) Lithotriptors in the OECD 6 5 4 3 2 1 18th 0 Source: OECD (2006) Calculations by Authors 40 Comparisons of Age Adjusted Access 24th of 28 countries for access to physicians 13th of 24 countries for access to MRI machines 17th of 23 countries for access to CT scanners 7th of 17 countries for access to Mammographs 18th of 20 countries for access to Lithotriptors41 Health Results: Health Outcomes 42 Sw G ed er e m n Lu a xe J ny m ap bo an N urg or w Sp ay Sw a itz I in er tal N F lan y et in d he la r n A lan d us d C ze t s ch A ral i Re ust a pu ria Fr blic D an en c e B ma el rk gi C u O an m E U C Ic ad ni D e a te A la d ve nd K r in ag N Ggdo e ew re m Z Sl e a ece ov ak Ir lan R el a d ep nd Po ub r li H t ug c un a g l Po ar la y K nd Tu ore rk a ey HALE/LE (%) (2002) Life Expectancy in Full Health in the OECD 92% 91% 16th 90% 89% 88% 87% 86% Source: OECD (2006); WHO (2006) 43 Ic el a Ja nd Fi pa Swnla n ed nd N C or en ze w ch a Re Sp y pu ain Fr bli a c G nc r Po ee e c G rtu e er g m al an y Sw B Ita e itz lg ly e iu D r la m en nd m A C u ark ha s rt tria A N u Av e Lu th stra g. xe erla lia m n bo ds Ire urg K C la U ore an nd n a O ite (2 ada E d N CD K 002 ew i A n... ) Ze ve al ra an ge Sl Po d.. . ov ak Hu lan R ng d ep ar ub y lic Rate per 1,000 Live Births (2003) Infant Mortality in the OECD Turkey not shown 8.0 7.0 6.0 21st 5.0 4.0 3.0 2.0 1.0 0.0 44 Source: OECD (2006) Ic el a C ze A Ja nd ch us pa K Re tra n or p lia ea ub (2 lic Fi 00 nl 2 an d Ita ) N P (2 ly or o 00 w rt 2 ay u ) g Lu S (20 al xe we 02) Sp mb de ai ou n n r G (20 g C erm 02) ha a rt ny C Avg an . A ad O u w EC G st a Ze D re ria D ala Av ec en n e e m d ( rag F a 2 e U ra rk ( 00 ni nc 2 2) te e 00 d (2 1 N Kin 00 ) et g 1 he d ) Sl rla om o w va itz k P nds er R ola la ep n nd u d (2 blic 0 Ire 01) H l an un d ga ry Rate per 1,000 Births (2003) Perinatal Mortality in the OECD 10.0 8.0 7.0 Turkey not shown 9.0 14th 6.0 5.0 4.0 3.0 2.0 1.0 0.0 Source: OECD (2006) 45 w Ja it p ze a rl n Fr and A an us c tr e Ic ali e a S la w nd ed en I C ta an ly a S da N pai or n Fi wa nl y Lu N x K and ew e o m r Ze b ea N al ou et an rg h d er . . la . A nd us s G t O G re ri a E e e C r c D m e A an U ni P ver y D ted or ag en K tu e m in ga ar g l k do (2 m . Ir .. C e ze ch P lan S lo R ol a d va ep n k ub d R li e H pu c un .. g . ar y S Rate per 100,000 (2002) Mortality from Disease in the OECD 900 800 700 600 8th 500 400 300 200 100 0 Source: OECD (2006) Calculations by Authors 46 Ic e Sw la n ed d en Sw J itz ap er an l N and o A rw us a tr y Fi alia nl an d I t C Can aly Lu ha a xe rt A da m v bo g. u A rg us Fr tria a G nce G ree er ce m an N e N O th Sp y ew E e a Ze CD rlan in al Av d an e s d rag (2 e D en 00 U m Ire 0) ni ar l te k an d (2 d K 00 in 1 gd ) o K m or ea Years (2002) Potential Years of Life Lost in the OECD 2900 2500 Portugal, Czech Republic, Poland, Slovak Republic, and Hungary not shown 2700 9th 2300 2100 1900 1700 1500 Source: OECD (2006) Calculations by Authors 47 n Ja ce A p us an t C rali an a S ad w a ed en Ita S ly p N No ain et r h w er a la y n A ds us G tri r a D ee e c C nm e ha a rt rk N A ew Fi vg Ze G nl . al e an r O an ma d d E C (2 ny D 0 A 00 ve ) U ni ra te d Ko g e K r i n ea gd Ir om C e ze P la ch or nd R tug ep a u l P bli ol c an d Fr a Mortality per 100,000 (2000) Medically Avoidable Mortality (MAHC) Slovak Republic, and Hungary not shown 160 140 120 100 4th 80 60 40 20 0 Source: WHO (2006) Calculations by Authors 48 Sw e Fi de nl n a K nd o Ic re A ela a us n tr d Lu a F xe r lia m an bo ce Sw N ur g itz orw er a l y C and an ad a N ew Ita J ly Ze ap U ni G a an te e la O d K rm nd EC i a n D gd ny A o ve m A rag us e G tri r a B ee el ce Po giu rt m u Po ga D l l en an m d N et S ark he p C rla ain ze ch I nd re s R Sl e p l an ov u d ak Hu bl i R ng c a ep r u y Tu bli rk c ey Female Mortality (2002) Breast Cancer Mortality in the OECD 45% 40% 35% 30% 10th 25% 20% 15% 10% 5% 0% Source: Ferlay et al. (2004) Calculations by Authors 49 itz e A r la us n tr d C ali an a ad J Lu ap a a xe m It n bo aly Ic urg el a K nd N S o ew w re e a Ze de al n a U ni G Fr nd te e an d rm ce K a in n gd y Fi om n N N la e O t h or nd EC e w D rla ay A nd ve s A rag us e t Sp ria G a r in B eec el e g Ire ium la C P ze ol nd P ch o an Re rtu d Sl g ov D pu al ak en bl i R ma c ep r k H ub un li g c Tu ar rk y ey Sw Combined Male and Female Mortality (2002) Colon/Rectum Cancer Mortality in the OECD 70% 60% 50% 2nd 40% 30% 20% 10% 0% Source: Ferlay et al. (2004) Calculations by Authors 50 Health Results: Getting What We Pay For? High cost system. Worsening waiting times. Poor performance on waiting times for elective medical care Poor results on access to doctors and technology. Mediocre performance on health outcomes. 51 Canada’s Policies are the Problem 52 Cost Sharing – User Fees, Deductibles and Co-payments – in the OECD 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Overall Hospital Cost Sharing GP No Cost Sharing Specialist 53 Cost Sharing in the OECD Only 5 countries do not have some form of cost sharing for major health care services in the public system: Canada, Czech Republic, Denmark, Spain, and the United Kingdom. Following reform in January 2006, The Netherlands allows cost sharing. Four of the 5 experience problems with waiting times— Canada, Denmark, Spain, and the United Kingdom and growing waiting lists are seen as a problem in the 5th. 54 Providers of Public Health Care in the OECD 70% 60% 50% 40% 30% 20% 10% 0% Public Ownership/Management Mixed Ownership 55 Providers of Public Health Care in the OECD 11 OECD countries rely exclusively on public hospitals to deliver publicly-funded health care. Of these 11, 8 experience problems with long waiting times. The remaining 3 are transition economies still in the process of reforming their economies and social service systems. Not one of the countries with strictly public provision exhibits attributes that would be counter to economic theory which suggests that this would result in inefficient provision of services. 56 Private Parallel Health Care in the OECD 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Available Not Available 57 Is Canada Unique? Only 2 of the 28 countries surveyed have no comprehensive private provision of healthcare: Canada and the Czech Republic. Canada is the only country to have full and complete public management of hospital resources and no private parallel insurance system. Canada is the only country to effectively outlaw private parallel 58 A Look at the Most Successful Universal Health Insurance Programs 59 Understanding Australia, Sweden, and Japan Lower healthcare costs. Better healthcare outcomes. User fees or co-payments. Parallel private medical treatment supply publicly funded care. 60 Australia Cost sharing accounted for 16% of total expenditure Benefit is 75% for professional inhospital services and 85% for all other professional services No controls on physician fees (extra billing), though physicians who accept 85% of the “schedule” can bill the government directly Private health insurance cover. Community rated with tax incentives 61 Sweden County councils deliver care Co-payments for physician services, hospital care, outpatient care, elderly care, dental, and drugs. Fees vary by county but are capped. Less than 2% of resources devoted to health care come from patient fees. No gatekeeping Stockholm county contracting with private providers – better care 62 Understanding Austria, Belgium, France, Germany, Japan, Luxembourg, and Switzerland Lower/similar healthcare costs. No Waiting Lists. User fees or co-payments. Parallel private medical treatment Social Insurance Financing Private hospitals competing to supply publicly funded care. 63 Japan Cost sharing accounted for 11.7 percent of total health expenditures in 2001 User fees of between 25 and 30 percent for physician services and hospital care. Varying rates for drugs. Almost total freedom to choose and use private and public health care services without a referral system. Competitive private delivery of care (79.9 percent of hospitals and 93.8 percent of clinics privately owned) 64 Switzerland Competing insurance funds – decentralized, self-administered, private and public. (Risk redistribution) Various deductible arrangements (varies between insurance policies) and 10% coinsurance rate. Direct patient payments accounted for 28% of total expenditure (both co-payments and private out of pocket payments) 65 Competitive private delivery of care So… How Good Is Canadian Health Care? Less than top performance in health care outcomes Ranks at the bottom in access to care, supply of technologies, supply of physicians Ranks at the very top in spending 66 The Trojan Horse for the Budget The Economics of the Canadian Health Care system 67 Avg Ann % Growth in GDP, CPI, TREV and PHEX 2000/01 to 2004/05 8.1% 4.6% 3.5% 2.4% National GDP National CPI Consolidated Provincial Total Revenues Consolidated Provincial Public Health Expenditures 68 Source: StatisticsCanada, Financial 2005 C Management System Avg Ann % Growth in PHEX and TREV, by Province 2000/01 to 2004/05 11.2 9.2 9.0 8.4 7.7 7.2 6.5 7.0 6.4 6.1 5.3 4.5 3.5 NFLD 4.3 3.7 3.5 3.3 PEI 5.3 NS NB QB PHEX ON 4.0 MB 4.0 SK AB BC TREV 69 Source: Statistics Canada, Financial Management System 2005 PHEX as % of TREV, by Province 1997 & 2005 39% 35% 31% 34% 31% 31% 28% 21% NFLD 24% 23% PEI NS 36% NB 32% 29% 28% 24% QC 1997 30% 23% ON MB SK 29% 30% 22% AB BC 2005 70 Source: Statistics Canada, Financial Management System 2005 ONTARIO: Projection based on 2000/01 to 2004/05 Avg Ann % Growth in actual PHEX and TREV 200000 180000 PHEX = 100% of TREV 160000 Millions Current $ 140000 120000 100000 80000 PHEX > 66% TREV 60000 PHEX > 50% TREV 40000 20000 0 32 31 30 29 28 27 26 25 24 23 71 20 20 20 20 20 20 20 20 20 22 21 20 19 18 17 16 15 14 13 12 11 10 09 08 07 06 TREV 20 20 20 20 20 20 20 20 20 20 20 20 20 20 20 20 20 20 PHEX Why projections are cautious 1. PHEX does not include the impact of aging population: 50% of per-capita, lifetime health expenditures occur after the age of 65. (Brimacombe et al., 2001) 2. PHEX includes drug delisting; reform efforts; rationalization 3. TREV overstated: Net of debt service costs, AVAILABLE revenues are lower 4. TREV includes Federal transfers 5. TREV includes tax increases 72 Other sustainability warnings Government (QC) Clair 2000 (SK) Fyke 2001 (AB) Mazankowski 2001 (Senate) Kirby 2001 (QC) Menard 2005 MacKinnon 2002 Private Sector Fraser Institute annually since 1990 C.D. Howe 2001 AIMS 2002 Fraser Institute 2004 – Mullins, Esmail, Skinner Conference Board 2001 & 2005 PWC 2005 73 PROBLEM CAUSE SOLUTION 1. Over utilization; moral hazard 1. 1st $ coverage; universal public subsidy 1. User fees; limited eligibility for public subsidy 2. Inadequate insurance protection 2. Insuring highfrequency, affordable expenses 2. Catastrophic insurance design 3. Inefficient allocation of resources 3. Central planning 3. Consumer empowerment and managed care 4. Absence of payer accountability 4. Public monopoly health insurance 4. Allow private insurance options 5. Undercapitalization 5. Non-profit provision 5. For-profit provision 74 The Canadian System is not the one to copy But What should be done? Lets consider the recommendations of the Blue Ribbon Commission 75 Health Insurance should be Universal OK 76 Health Insurance must be legislated – that is not optional for residents OK 77 National Health Insurance should be Administered by the National Insurance Board Not OK Commission notes that the NIB is hopelessly inefficient – 25% overstaffed….this is not coincidental Commission notes that the inefficiency of the NIB will have to be dealt with…yes…but how?? Commission doesn’t question “Central planning model” and hidden costs of monopoly 78 The NHI plan should be comprehensive Not OK This is the real Trojan horse 1. Cost of insuring for “oil changes” 2. Eliminates the private option because private spending only permitted for services which exceed or are not covered by NHI 3 This provision is the most sinister in the report and is the Achilles heel of the Canadian Model – recently rejected by the Supreme Court of Canada 79 Contributions set at a level Affordable by the Majority Not what the Commission actually advises Commission’s recommendation is that in the summary but in the document the Commission proposes a progressive Income Tax to finance the program 80 No User Fees Not OK Evidence shows that they don’t prevent access Exempt the poor Involve the patient in the paying process 81 Conclusion There are many models for Bahamians to follow that will produce better outcomes than following the Canadian Plan In considering the Commission’s report Bahamians should note that it recommends the adoption of the Canadian system while nobody else in the world has thought it a good idea to do so I wonder why? 82 www.freetheworld.com www.fraserinstitute.ca 83