Lightman et al_revision 18-6-14
advertisement

Pegylated Interferon α-2breduces corticosteroid requirement in patients with Behcet’s disease with
upregulation of circulating regulatory T cells and reduction of Th17
S Lightman,1,2 S RJ Taylor,1,3 C Bunce,1 H Longhurst,4 W Lynn,5 R Moots,6 M Stanford,7 O TomkinsNetzer,1,2 D Yang,2 V L Calder,2 D O Haskard3
1
Moorfields Eye Hospital NHS Foundation Trust, London, UK
2
UCL Institute of Ophthalmology, London, UK
3
Imperial College Healthcare NHS Trust, London, UK
4
Barts Health NHS Trust, London, UK
5
Ealing Hospital NHS Trust, London, UK
6
Aintree Hospitals NHS Trust, Liverpool, UK
7
GSTT NHS Foundation Trust, London, UK
Corresponding author:
Professor Sue Lightman
UCL Institute of Ophthalmology, Moorfields Eye Hospital
162-165 City Road
London EC1V 2PD
Tel: 020 7566 2266
Fax: 020 7251 9350
Email: s.lightman@ucl.ac.uk
1
ABSTRACT
Objective To determine whether the addition of 26 weeks of subcutaneous peginterferon-α-2b
could reduce the requirement for systemic corticosteroids and conventional immunosuppressive
medication in patients with Behçet’s disease (BD).
Methods We conducted a multicentre randomised trial in patients with BD requiring systemic
therapy. Patients were randomised to a 26 week of peginterferon-α-2b in addition to their standard
care or to standard care only and followed 6 monthly for 3 years with BD activity scores and quality
of life questionnaires. Patients at one centre had blood taken to measure regulatory T cells (Tregs)
and Th-17cells.
Results 72 patients were included. At months 10-12, while among the entire patient population
there was no difference in the corticosteroid dose or immunosuppression use between the
treatment groups (adjusted OR 1.04,95% CI, 0.34-3.19), post hoc analysis revealed in patients who
were on corticosteroids at baseline the corticosteroid requirement was significantly lower in the
peginterferon-α-2b (6.5 {5,15} mg/day) compared with the non-interferon group (10 {8.25, 16.5}
mg/day ,p=0.039). Furthermore, there was a trend towards an improved quality of life that became
significant by 36 months (p= 0.008). This was associated with a significant rise in Tregs and a
decrease in Th17 cells which was still present at 1 year, 6 months after the interferon was stopped.
The safety profile was similar with adverse events in 10% in both groups.
Conclusions The addition of peginterferon-α-2b to the drug regime of BD patients did not
significantly reduce corticosteroid dose. However in a post hoc analysis, the treatment resulted in a
significant reduction in corticosteroid dose with an improved quality of life and trend to reduce
other required immunosuppressive agents among patients who were on corticosteroids at baseline.
The effect was seen at 1 year and was associated with a rise in Tregs suggesting a possible mode for
interferon action.
Trial registration number The study is registered on the following trial registries: ISRCTN 36354474;
EudraCT 2004-004301-18.
Keywords: Behçet’s disease, peginterferon-α-2b, regulatory T cells, corticosteroid,
immunosuppressive agents
2
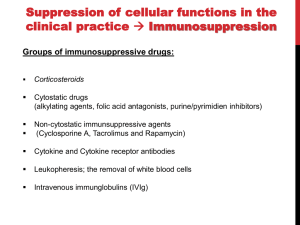
Behçet’s disease (BD) is a multisystem condition of unknown causation.[1] Its severity varies, ranging
from mucocutanous lesions to more severe manifestations – particularly ocular involvement, in
which retinal ischaemia can occur with permanent visual loss.[2] Treatment of major organ
involvement is with immunosuppressive agents and corticosteroids, and is usually required for many
years,[3, 4] with relapses occurring when drug doses are reduced.[2, 5]Biologics such as infliximab
are increasingly used with and without corticosteroids, especially when other drugs have failed or
had to be discontinued because of adverse events.[6] Use of interferon alpha 2a and 2b in BD have
been reported in several randomized studies as well as small case series .[7-10] In some studies
interferon alpha has been used continuously but in others a short course of the drug appears to
induce prolonged disease remission allowing discontinuation of all medication without relapse. The
mechanism of interferon in BD is unknown, but in some patients treated for hepatitis B infection,
regulatory T cells (Tregs) are induced.[11]
This study aimed to determine whether the addition of 26 weeks of subcutaneous peginterferon-α2b at a standard dose of 0.3μg/kg/week could reduce the requirement for systemic corticosteroids
and conventional immunosuppressive medication at one and three years in patients with BD. Tregs
and Th17 cells in peripheral blood were measured over the course of the first year in patients from
both treatment groups attending one site.
METHODS
Design
The study was a multicentre, randomised, controlled, parallel group, single-masked clinical trial of
peginterferon-α-2b in BD patients on systemic treatment. Patients were randomly assigned in a 1:1
ratio, to one of two treatment groups and were stratified in blocks according to centre, disease
duration (< three years, or ≥three years) and the presence of ocular involvement. Stratification
according to disease duration was based on an increased risk of ocular involvement among patients
with disease over 3 years because higher treatment doses are frequently required for sightthreatening disease.[12]
The two treatment groups were as follows: systemic corticosteroids and/or immunosuppressive
agents; or systemic corticosteroids and/or immunosuppressive agents plus peginterferon-α-2b at a
dose of 0.3 μg/kg/week for 26 weeks. The study was masked with regard to treatment assignment
only to the study assessors but unmasked to the patients, research nurse and the clinicians
overseeing medical care of the patients. This was because the flu-like symptoms associated with
interferon treatment made patient masking unfeasible. The study was approved by each centre’s
institutional review board and was conducted in accordance with the provisions of the Declaration
of Helsinki and Good Clinical Practice guidelines (ISRCTN 36354474 EudraCT number 2004-00430118).
Study oversight
3
The trial was conducted at five sites in the UK with randomisation and pegylated interferon
distribution for all sites undertaken by the study research nurse. Schering Plough donated the
peginterferon-α-2b at a concessionary cost but had no role in the design of the study, the collection
or analysis of the data. The principal investigators and the study sponsor were jointly responsible for
the study design, protocol, statistical analysis plan and data analysis.
The trial was managed by a Trial Steering Committee and had an independent Data Monitoring
Committee. The audited data was inputted to the trial database by the sponsor’s staff and analysed
by the trial statistician (CB).
Study participants
We enrolled 72 BD patients, who were 18 years of age or older, had been diagnosed on the basis of
the International Study Group criteria,[13] and required treatment with corticosteroids and/or
systemic immunosuppressive agents for systemic and/or ocular disease. Patients were excluded if
they had severe renal or hepatic dysfunction, uncontrolled thyroid function or a severe psychiatric
disorder. Women were required to be taking effective contraceptive measures. Patients were also
required to be on stable levels of immunosuppressive therapy for four weeks before enrolment. For
a full list of inclusion and exclusion criteria see the study protocol (Appendix 1).
Interventions
Patients continued to receive their medications at baseline. As azathioprine and peginterferon-α-2b
may induce leukopenia, ALL patients taking azathioprine were initially required to stop this drug,
although some patients randomised to standard therapy did not do so at their request. Participants
who were assigned to the peginterferon-α-2b group were given packs of four interferon injections
monthly. Study visits for all patients were at 6, 12, 18, 24, 30 and 36 months. Additionally, all
patients were seen as required by clinical need and for all immunosuppressive drug monitoring.
Systemic immunosuppression was adjusted according to the clinical findings and reduced where
possible as per protocol (Appendix 1). The addition of biologic agents was based on clinical
judgement according to either treatment efficacy or drug intolerance. Serious adverse events and
adverse events were documented, reported and managed appropriately. The PI with expertise in
interferon (WL) was consulted where necessary.
At the time of enrolment and at every study visit, validated interviewer administered BD-QoL15and
fatigue questionnaires[14]were undertaken. Systemic disease activity was measured clinically by
masked observers using the previously validated Leeds BD Activity questionnaire (excluding the
ocular disease section).[15, 16] Ocular disease activity was measured separately by masked
observers using the International Uveitis Study Group grading scales.[17] As part of the trial
protocol, a standardised definition of ocular and systemic relapses was used, and were graded as
mild, moderate or severe (Appendix 1). For statistical analysis, mild and moderate relapses were
combined, a decision taken in advance of examining outcome data.
4
Patients attending the Moorfields Clinic (PI SL) had blood taken at study visits 0, 3, 6 and 12 months
for measurement of Treg subsets to see if these changed by the addition of peginterferon-α-2b and
whether these correlated with the clinical outcome at 1 year. Full details of laboratory analysis
including cell phenotyping and flow cytometry can be found in Appendix 2.
Outcomes
The primary outcome measure was whether a corticosteroid dose equivalent to no more than 10mg
of prednisolone per day was required throughout months ten to twelve following treatment
initiation. Secondary endpoints included the number of disease relapses, mean doses of
corticosteroids and immunosuppressive agents required for disease control, and questionnaire
scores up to 3 years. Additionally the average daily amount of corticosteroid throughout months 25
to 36 following treatment initiation was calculated.
Power calculation and statistical analysis
Recent literature in BD patients receiving interferon in published studies suggested a major
reduction of corticosteroid dose of up to 80%. We calculated the sample size using a less optimistic
steroid reduction but one that was still clinically significant. Assuming a 10% loss to follow-up, 70
randomised subjects, yielding 31 followed-up patients in each arm, would have 87% power to detect
a difference at 1 year between 5% of patients on a steroid dose of 10 mg or less on every day in the
non-interferon arm and a 60% in the peginterferon alfa-2b group with an alpha of 0.05 (using
Fisher's exact test.)
Fisher's exact test was used to compare the outcome measures between treatment groups at one
and 3 years. Since randomisation was stratified by centre, duration and ocular involvement, an
adjusted analysis was conducted using logistic regression. Analysis included data from all patients
who underwent randomisation and was performed on an intention-to-treat basis. A sensitivity
analysis was conducted using best case and worse case scenarios for missing data to ensure that the
findings were robust to loss to follow up. All analyses were conducted using Stata statistical
software (StataCorp, TX, USA) and all statistical tests used a significance level of 0.05. Post hoc
analysis of results of those patients grouped according to use of corticosteroids at baseline was also
carried out. Normally distributed data is presented as mean (standard deviation) and non-normally
distributed data are presented as median {IQR}.
RESULTS
Participants
Between June 2006 and April 2009, a total of 72 patients underwent randomisation and there were
no significant differences at baseline between the 2 groups (Table 1). After stratification on the
basis of centre, duration of disease and presence or absence of ocular involvement, 36 of 72 patients
5
(50%) were randomised to continue to receive systemic corticosteroids and/or 2nd-line
immunosuppressive agents and 36 (50%) to receive an addition of 26 weeks of subcutaneous
peginterferon-α-2b to their drug regime. 27/36 patients (75%) completed the full 26 week course of
peginterferon-α-2b. One additional patient missed one injection only due to transiently-raised liver
function tests; no patients were withdrawn from therapy with peginterferon-α-2b owing to adverse
events. 11 patients self-withdrew and were equally divided between the two groups (Figure 1). 25
patients in each arm were on corticosteroids at baseline, 5 and 7 patients respectively were taking
doses of less than 10 mg, 20 patients in the interferon arm were taking 10mg or more compared
with 18 in the standard treatment arm. 23 patients in the peginterferon group and 28 in standard
treatment arm were on 2nd-line agents and no patients were on biologics at baseline (Table 1).
Table 1- Baseline Demographic and Disease Characteristics of the Study Patients, in each treatment
group (figures are mean ± SD, unless otherwise stated)
Characteristic
Peginterferonα-2b
n = 36
40.4 ± 9.6
14/36 (39%)
Non-interferon
n = 36
41.9 ±9.4
16/36 (44%)
Age in years
Male sex – no. (%)
Race or ethnic group – no. (%)
- White
27 (75%)
27 (75%)
- Asian
4(11 % )
1 (3%)
- Other/ Unknown
5 (14%)
8 (22%)
Weight – kg median {IQR}
80 {65,92}
69.9 {64, 82}
Diabetes mellitus – no. (%)
2/34 (5.9%)
2/34 (5.9%)
Systolic BP – mm Hg
120.7 ± 13.3
124.9 ± 12.9
Diastolic BP – mm Hg
77.6 ± 9.4
76.9 ± 12.6
Disease location – no. (%)
- Ocular
15 (42%)
21 (58%)
- Systemic
18 (50%)
14 (39%)
- Both
3 (8%)
1 (3%)
Duration of disease – year
9 {4.5, 12.5}
12 {7, 17}
median {IQR}
Requiring immunosuppressive
agents – number
- Corticosteroids
25/36
25/36
- Conventional second-line
23/36
28/36
agents*
- Biological agents
0/36
0/36
Dose of corticosteroid at baseline
11.5 (5.3)
16.1 (16.4)
in patients taking corticosteroid
at baseline – mg/day
*indicates either azathioprine, mycophenolate, ciclosporin, tacrolimus, methotrexate, but excludes
concomitant use of colchicine
Primary outcome
6
The primary outcome for this study was whether a corticosteroid dose equivalent to no more than
10mg of prednisolone per day was required throughout months ten to twelve following treatment
initiation. Looking at the whole group, there was no difference in the number of patients receiving
10mg or less per day of corticosteroids at months 10 -12 - 66% (95% CI, 46%-82%) for the
peginterferon-α-2b group and 62% for the non-interferon group (44%-79%, p=1.00, adjusted OR
1.04,95% CI, 0.34-3.19), Table 2, online supplementary Table S1). The median {IQR} dose of
prednisolone measured by the mean dose over months 10-12inclusive, was 5.00mg/day {1-10} in the
peginterferon-α-2b group and 10.00mg/day ({2.5-15} in the non-interferon group. The number of
additional immunosuppressive agents and the number of patients using biologics were also not
significantly different. Additionally there was no difference in the corticosteroid dose of 10mg or
more in the last year of the study between the treatment groups - 50% for the peginterferon-α-2b
group and 58% for the non-interferon group (p=0.78). At three years, the median daily doses of
prednisolone were 5.1mg/day {0-10} and 7.5mg/day {0-11.5} respectively. There was no difference
in the relapse rates recorded between the two groups. There was no significant difference in BD-QoL
scores at the primary endpoint of 12 months, although there was a tendency for the interferon
treated group to have better scores throughout the trial and at 36 months this difference was
statistically significant (P = 0.008, online supplementary Figure S1). Higher fatigue scores were
observed in the standard treatment arm, though not statistically significant.
Table 2- Outcome measures in whole group
Peginterferon
α-2b
Noninterferon
P value
Patients on 10mg corticosteroid
or less – no/total no (%, 95 %
CI) at year 1
19/29 (66%)
{46 %, 82 %}
mAbs
20/32 (62%)
{44 %, 79 %}
1.000
- Ocular patients
- Systemic patients
Ocular patients rate of relapse
at year 1
Systemic patients rate of
relapse at year 1
Severe relapse rate in year 1 –
no./total no. (%)
Severe relapses in year 1
0
1
2
3 or >3
Patients on 10mg corticosteroid
or less – no/total no (%,95 %
CI)at year 3
- Ocular patients
Systemic patients
7/13 (54%)
12/16 (75%)
4/13 (31%)
12/19 (63%)
8/13 (61%)
5/19 (26%)
1.000
2/16 (13%)
5/13 (38%)
0.192
6/29 (21%)
10/32 (31%)
0.395
23
3
3
0
12/24 (50%)
{29%, 71%}
22
6
1
3
15/26 (58%)
{37%, 77%}
4/10 (40%)
8/14 (57%)
9/16 (56%)
6/10 (60%)
Measure
0.189
7
0.777
Ocular patients rate of relapse
at year 3
Systemic patients rate of
relapse at year 3
Severe Relapse rate in year 3 –
no./total no. (%)
Severe relapses in year 3
0
1
2
3 or >3
1/10 (10%)
2/16 (12.5%)
1.000
2/14 (14%)
3/10 (30%)
0.615
3/24 (12.5%)
5/26 (19%)
0.704
21
2
0
1
21
4
1
0
0.658
Outcomes for patients on corticosteroids at baseline
The secondary analysis included evaluation of treatment effect among patient receiving
corticosteroids at baseline. The baseline characteristics of these patients (25/36 in each arm) were
the same between the two treatment groups (online supplementary Table S2). However at 1 year,
the corticosteroid dose required to control the disease was significantly lower in the peginterferonα-2b group (6.5mg/day {5-15}) compared with the non-interferon group (10mg/day {8.25-16.5},
p=0.039). This effect was lost by three years when the amount of corticosteroid was the same in
both groups at 8.8mg/day {0.4-10} in the non-interferon group versus 8.8mg/day {6.7-14.6} in the
peginterferon-α-2b group (p=0.309). Additionally there was a non-significant trend for less use of
2nd-line immunosuppressive agents, use of biologics and a decreased severe relapse rate in the
peginterferon treated group at 1 year that was also less apparent by 3 years (Table 3). Response was
unaffected by the duration of disease, location (ocular or systemic), age or gender.
Table 3- Change from Baseline in patients on corticosteroids at baseline
Measure
Peginterferon
Non- interferon
P value
6.5 (5, 15)
10 (8.25, 16.5)
0.039
8.8 (0.4, 10)
8.8 (6.7, 14.6)
0.309
At Year 1
-0.29 (0.85)
0 (0.58)
0.24
At Year 3
-0.24 (1.25)
0 (0.73)
0.55
0 (0)
15.8 (3)
0.23
Corticosteroid dose mg/day
at 1 year
Corticosteroid dose mg/day
at 3 years
Change from baseline in
number of 2nd line agents,
mean (SD)
% of pts. using biologic
agents, % (n) Year 1
8
Year 3
Severe relapse rate in year 1 –
no./total no. (%)
Number of Severe relapses
during year 1
- 0
- 1
- 2
- 3
- 4
- 5
Severe relapse rate in year 3–
no./total no. (%)
Number of severe relapses
during year 1
- 0
- 1
- 2
- 3
23.5 (4)
5/21 (23.8%)
18.7 (3)
9/24 (37.5%)
0.54
0.36
16
2
3
0
0
0
3/18
(16.7%)
15
6
0
2
0
1
4/18
(22.2%)
0.293
1.0
0.713
15
2
0
1
14
3
1
0
Adverse events
The types and frequency of ocular and systemic adverse events were different, as expected, among
the two groups (online supplementary Table S3). There were 63 adverse events, including recurrent
pulmonary embolism and septicaemia, but there was no difference between the two groups in their
frequency during the course of the trial. Even though more patients in the non-peginterferon-α-2b
group had haematological abnormalities this was not statistically significant (p=0.305). The severe
relapse rate was similar in both groups (Table 2).
Regulatory cells
In the 33 patients on corticosteroids at baseline who had Tregs measured, there was no difference at
baseline between the 2 treatment groups (p=0.41). However, Tregs (CD4+CD25hi, FoxP3+) were found
to be significantly increased by 3 months’ treatment with peginterferon-α-2b (p=0.05), and
remained increased at 6 months (p=0.01) and at 12 months (p=0.01), six months after ceasing
peginterferon-α-2b therapy. No such increases were seen in the non-interferon treated group of 17
patients (Figure 2).
9
There was a significant downregulation of Th17 cells in the peginterferon-α-2b treated group at all
timepoints to 12 months in cultures stimulated with PMA/ionomycin (Figure 3). As early as 3 months
after initiation of peginterferon-α-2b therapy, the median percentage of IL-17+ expression by CD4+ T
cells decreased (0.8% (0.3-1.9%),p=0.03) compared to baseline (2.0% (1.7-2.6%)). Th17 cells
remained low at 6 months (0.8% (0.7-1.2%), p=0.03) and at 12 months (1.0% (0.7-1.8%),p=0.03), six
months after cessation of peginterferon-α-2b therapy. This effect on Th17 cells was detected at 6
months in the conventional treatment group, but was not found at the other timepoints.
DISCUSSION
This study primarily aimed to see if treatment with peginterferon-α-2b for six months allowed
significant corticosteroid reduction in BD patients. While among the entire patient population there
was no difference in the corticosteroid dose between the treatment groups, in those patients
already on corticosteroids at baseline there was a significant decrease in the dose of corticosteroids
required to control the disease. In addition there was a trend for less use of corticosteroids and
other immunosuppressive agents and biologics (anti-tumour necrosis factor inhibitors) without an
increase in the severe relapse rate and a relatively better quality of life score. This was associated
with an increase in the number of circulating Tregs which was still present at 1 year and not present
in those on conventional therapy.
BD is heterogeneous with different phenotypes so a heterogeneous response to therapies could be
anticipated. A major role in pathogenesis is suggested for Th1 and Th2 cells and more recently for
Th17 cells.[18]Individual susceptibility seems to be modulated by genetic variants in genes codifying
these cytokines.[18, 19] Th1 and Th17 cells are thought to be involved in active disease phases
whereasTh2 cells affect the development or severity of the disease.[20] Th17 responses were
controlled by Tregs in rheumatoid arthritis (RA) patients on infliximab [21] and anti-TNF therapy was
found to induce Tregs in RA patients.[22] In ocular fluids, infliximab inhibited Th17 differentiation by
CD4+ cells.[23]This suggests that Tregs are able to modulate Th17 responses and therefore can
decrease inflammatory activity in disease settings. IL-17 is also thought to co-ordinate the cross talk
between lymphocytes and neutrophils in BD, so the related cytokines could be potential targets for
therapy.[24, 25]
In this study, a beneficial effect of peginterferon-α-2b was seen only in those patients already on
corticosteroids at baseline, possibly those with more severe disease manifestations. This was
accompanied by an increase in quality of life, despite the negative effect interferon has on patients
quality of life. Others have suggested that interferon only works when corticosteroids and other
immunosuppressive agents have been discontinued as its effect is mitigated by these agents.[7]
We did not confirm this in our study and indeed those on minimal systemic therapy did not have
any benefit from the addition of peginterferon-α-2b at least in the parameters measured. The
mode of action of interferon may depend on the dose used, as at very high doses, such as those
used in treating melanoma, an immunostimulatory mechanism has been suggested[26] although
others have found an increase in Tregs.[27] In patients undergoing interferon therapy for liver
fibrosis, upregulated Tregs have also been detected.[28] It is possible that corticosteroids
10
themselves can increase the number of Treg cells that are then further upregulated by the
interferon.[29, 30]Tregs control immune responses to self antigens and can modulate the effect of
many immune cells by blocking proliferation, differentiation and effector functions.[31] It remains
unknown whether persistence of some Tregs is responsible for the reduced relapse rate with time
seen in some studies where Infliximab and interferon-α were compared to conventional
immunosuppressive agents such as ciclosporine and azathioprine. In addition to the potentiating
effect on Tregs, there was a concomitant decrease in the percentages of Th17 cells in the paired
blood specimens that were obtained at all time points. Th17 cells have been proposed as effector
cells in active BD, and their downregulation by interferon-α could be a reflection of the
upregulation of Tregs, although this requires further study.
Interferon-α has been used in BD patients since the mid-1980s and there is no consensus about
the ideal dose or duration of treatment. Anti-TNF drugs, particularly infliximab are also very
effective in rapidly resolving inflammatory episodes in patients with BD[32, 33] and recently have
been shown in open label trials to reduce the relapse rate.[34, 35] Infliximab therapy confers an
increased risk of infection, particularly reactivation of latent tuberculosis [36] which is not seen
with interferon-α. Other biologics and anti-interleukin therapies have been reported as effective in
small series of BD patients.[37]
Previously reported studies have involved treating patients with varying levels of disease activity
whereas in this study all patients had to have stable disease with no change in medication for at
least 1 month prior to the trial. BD is also very heterogenous in terms of disease severity so that
reported studies may not be comparable for this reason.
In summary, six months of peginterferon-α-2bhad a significant effect on corticosteroid reduction
which lasted for a further six months after treatment was stopped. This occurred when the
peginterferon-α-2b was added into the systemic treatment regime and did not require the other
drugs to be discontinued first. The rise in Tregs and Th17 reduction, occurring in the peginterferonα-2b group, may have contributed to disease suppression.
11
Acknowledgements The authors would like to thank Dr Colin Barnes and Professor Richard Powell
for chairing the Trial Steering Committee and the Data Monitoring Committee respectively and for
the help of the research fellows and nurses. The Behcet’s syndrome society assisted greatly by
helping fund patients travel expenses and also by assisting with data audit prior to the analysis
Funding This study was funded by the Moulton Trust. Patient travel expenses were funded by the
Behcet’s syndrome society.
Competing interests SLhas received consultancy fees, research grants, received payment for
development of educational presentations, done speakers bureaus and/or been on the advisory
board of GSK, BBRS and Allergan. HL has received consultancy fees, research grants, received
payment for development of educational presentations and/or done speakers bureaus from CSL
Behring, Shire, Viropharma, Baxter, Dyaxand Biocryst. SRJT has received consultancy fees and/or
been on the advisory board of Novartis and Santen and has received meeting expenses from
Novartis. DOH has received consultancy fees and/or research grants from Novartis and the British
Heart Foundation and has been on the advisory board of Servier. No other authors have any
competing interests to disclose.
12
REFERENCES
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
Barnes CG, Yazici H. Behcet's syndrome. Rheumatology (Oxford) 1999;38:1171-4.
Taylor SR, Singh J, Menezo V, et al. Behcet Disease: Visual Prognosis and Factors Influencing the
Development of Visual Loss. Am J Ophthalmol 2011;152:1059-66.
Yazici H, Pazarli H, Barnes CG, et al. A controlled trial of azathioprine in Behcet's syndrome. N
Engl J Med 1990;322:281-5.
Masuda K, Nakajima A, Urayama A, et al. Double-masked trial of cyclosporin versus colchicine
and long-term open study of cyclosporin in Behcet's disease. Lancet 1989;1:1093-6.
Sakane T, Takeno M, Suzuki N, et al. Behcet's disease. N Engl J Med 1999;341:1284-91.
Okada AA, Goto H, Ohno S, et al. Multicenter study of infliximab for refractory uveoretinitis in
Behcet disease. Arch Ophthalmol 2012;130:592-8.
Zouboulis CC, Orfanos CE. Treatment of Adamantiades-Behcet disease with systemic interferon
alfa. Arch Dermatol 1998;134:1010-6.
Kotter I, Zierhut M, Eckstein A, et al. Human recombinant interferon-alpha2a (rhIFN alpha2a) for
the treatment of Behcet's disease with sight-threatening retinal vasculitis. Adv Exp Med Biol
2003;528:521-3.
Alpsoy E, Durusoy C, Yilmaz E, et al. Interferon alfa-2a in the treatment of Behcet disease: a
randomized placebo-controlled and double-blind study. Arch Dermatol 2002;138:467-71.
Calguneri M, Ozturk MA, Ertenli I, et al. Effects of interferon alpha treatment on the clinical
course of refractory Behcet's disease: an open study. Ann Rheum Dis 2003;62:492-3.
Sprengers D, Stoop JN, Binda RS, et al. Induction of regulatory T-cells and interleukin-10producing cells in non-responders to pegylated interferon-alpha therapy for chronic hepatitis B.
Antivir Ther 2007;12:1087-96.
Deuter CM, Kotter I, Wallace GR, et al. Behcet's disease: ocular effects and treatment. Prog
Retin Eye Res 2008;27:111-36.
International Study Group for Behcet's Disease. Criteria for diagnosis of Behcet's disease. Lancet
1990;335:1078-80.
Chalder T, Berelowitz G, Pawlikowska T, et al. Development of a fatigue scale. J Psychosom Res
1993;37:147-53.
Gilworth G, Chamberlain MA, Bhakta B, et al. Development of the BD-QoL: a quality of life
measure specific to Behcet's disease. J Rheumatol 2004;31:931-7.
Bhakta BB, Brennan P, James TE, et al. Behcet's disease: evaluation of a new instrument to
measure clinical activity. Rheumatology (Oxford) 1999;38:728-33.
Bloch-Michel E, Nussenblatt RB. International Uveitis Study Group recommendations for the
evaluation of intraocular inflammatory disease. Am J Ophthalmol 1987;103:234-5.
Hamzaoui K, Bouali E, Ghorbel I, et al. Expression of Th-17 and RORgammat mRNA in Behcet's
Disease. Med Sci Monit 2011;17:CR227-34.
Zhou ZY, Chen SL, Shen N, et al. Cytokines and Behcet's disease. Autoimmun Rev 2012;11:699704.
Sojka DK, Fowell DJ. Regulatory T cells inhibit acute IFN-gamma synthesis without blocking Thelper cell type 1 (Th1) differentiation via a compartmentalized requirement for IL-10. Proc Natl
Acad Sci U S A 2011;108:18336-41.
McGovern JL, Nguyen DX, Notley CA, et al. Th17 cells are restrained by Treg cells via the
inhibition of interleukin-6 in patients with rheumatoid arthritis responding to anti-tumor
necrosis factor antibody therapy. Arthritis Rheum 2012;64:3129-38.
Nadkarni S, Mauri C, Ehrenstein MR. Anti-TNF-alpha therapy induces a distinct regulatory T cell
population in patients with rheumatoid arthritis via TGF-beta. J Exp Med 2007;204:33-9.
Sugita S, Kawazoe Y, Imai A, et al. Inhibition of Th17 differentiation by anti-TNF-alpha therapy in
uveitis patients with Behcet's disease. Arthritis Res Ther 2012;14:R99.
13
24. Neves FS, Spiller F. Possible mechanisms of neutrophil activation in Behcet's disease. Int
Immunopharmacol 2013;17:1206-10.
25. Wright GP, Stauss HJ, Ehrenstein MR. Therapeutic potential of Tregs to treat rheumatoid
arthritis. Semin Immunol 2011;23:195-201.
26. Mozzillo N, Ascierto P. Reduction of circulating regulatory T cells by intravenous high-dose
interferon alfa-2b treatment in melanoma patients. Clin Exp Metastasis 2012;29:801-5.
27. Soldevila B, Alonso N, Martinez-Arconada MJ, et al. Regulatory T cells and other lymphocyte
subpopulations in patients with melanoma developing interferon-induced thyroiditis during
high-dose interferon-alpha2b treatment. Clin Endocrinol (Oxf) 2013;78:621-8.
28. Feng L, Kang H, Liu LN, et al. CD4CD25 Foxp3 Regulatory T Cells Contribute in Liver Fibrosis
Improvement with Interferon Alpha. Inflammation 2013;36:1374-82.
29. Seissler N, Schmitt E, Hug F, et al. Methylprednisolone treatment increases the proportion of
the highly suppressive HLA-DR(+)-Treg-cells in transplanted patients. Transpl Immunol
2012;27:157-61.
30. Yang L, Ma QL, Yao W, et al. Relationship between the anti-inflammatory properties of
salmeterol/fluticasone and the expression of CD4(+)CD25(+)Foxp3(+) regulatory T cells in COPD.
Respir Res 2011;12:142.
31. Vaccarino L, Triolo G, Accardo-Palombo A, et al. Pathological Implications of Th1/Th2 Cytokine
Genetic Variants in Behcet's Disease: Data from a Pilot Study in a Sicilian Population. Biochem
Genet 2013;51:967-75.
32. Suhler EB, Smith JR, Wertheim MS, et al. A prospective trial of infliximab therapy for refractory
uveitis: preliminary safety and efficacy outcomes. Arch Ophthalmol 2005;123:903-12.
33. Niccoli L, Nannini C, Benucci M, et al. Long-term efficacy of infliximab in refractory posterior
uveitis of Behcet's disease: a 24-month follow-up study. Rheumatology (Oxford) 2007;46:11614.
34. Taylor SR, Singh J, Menezo V, et al. Behcet disease: visual prognosis and factors influencing the
development of visual loss. American journal of ophthalmology 2011;152:1059-66.
35. Tugal-Tutkun I, Mudun A, Urgancioglu M, et al. Efficacy of infliximab in the treatment of uveitis
that is resistant to treatment with the combination of azathioprine, cyclosporine, and
corticosteroids in Behcet's disease: an open-label trial. Arthritis Rheum 2005;52:2478-84.
36. Hatemi G, Melikoglu M, Ozbakir F, et al. Quantiferon-TB Gold in tube assay for the screening of
tuberculosis before and during treatment with tumor necrosis factor alpha antagonists. Arthritis
Res Ther 2012;14:R147.
37. Mesquida M, Molins B, Llorenc V, et al. Current and future treatments for Behcet's uveitis: road
to remission. Int OphthalmolPublished Online First:1 Jun 2013.
14
Figure Legends
Figure 1- Recruited patient data
Figure 2- Treg populations in whole blood from patients on corticosteroids in the non-interferon
(n=17) and peginterferon (n=16) treated groups, measured over 12 months. **p=0.01
Figure 3- Th17 populations in whole blood from patients on corticosteroids in the non-interferon
(n=7) and peginterferon treated (n=6) groups, measured over 12 months. *P<0.05
15