Migraines suck
advertisement

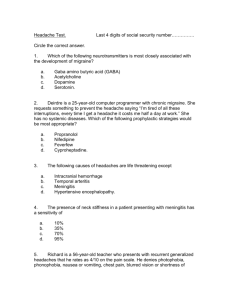
Headache By Wael Hamdy Mansy, MD Assistant Professor of Clinical Pharmacy King Saud University Classification of headaches Primary headaches OR Idiopathic headaches – THE HEADACHE IS ITSELF THE DISEASE – NO ORGANIC LESION IN THE BEACKGROUND – TREAT THE HEADACHE! Secondary headaches OR Symptomatic headaches – THE HEADACHE IS ON LY A SYMPTOM OF AN OTHER UNDERLYING DISEASE – TREAT THE UNDERLYING DISEASE! History and examination should clarify if Type of hedeache (1ry or 2ry). Is any urgency? In case of 1ry headache only the headache attacks should be treated “attack therapy, or prophylactic therapy is also necessary. SECONDARY, SYMPTOMATIC HEADACHES THE HEADACHE IS A SYMPTOM OF AN UNDERLYING DISEASE, LIKE – – – – – – – – – – – Hypertension Sinusitis Glaucoma Eye strain Fever Cervical spondylosis Anaemia Temporal arteriitis Meningitis, encephalitis Brain tumor, meningeal carcinomatosis Haemorrhagic stroke… Primary, idiopathic headaches Tension type of headache Migraine Cluster headache Other, rare types of primary headaches Tension headache Renamed tension-type headaches by the International Headache Society in 1988, are the most common type of primary headaches. The pain can radiate from the neck, back, eyes, or other muscle groups in the body. Tension-type headaches account for nearly 90% of all headaches. Approximately 3% of the population has chronic tension-type headaches Tension –type headaches can be episodic or chronic. Episodic tension-type headaches occur 15 days a month. Chronic tension-type headaches 15 days or more a month for at least 6 months. Can last from minutes to days, months or even years, though a typical tension headache lasts 4-6 hs Cluster headache Nicknamed "suicide headache", is a neurological disease that involves an immense degree of pain. "Cluster" refers to the tendency of these headaches to occur periodically, with active periods interrupted by spontaneous remissions. The cause of the disease is currently unknown. It affects approximately 0.1% of the population, and men are more commonly affected than women Migraine Headache Prevalence Familial Young, healthy women; F>M: 3:1 – 17 – 18.2% of adult females – 6 – 6.5% adult males 2-3rd decade onset… can occur sooner Peaks ages 22-55. ½ migraine sufferers not diagnosed. 94% of patients seen in primary care settings for headache have migraines Common misdiagnoses for migraine: – Sinus Headache (HA) – Stress HA Referral to ENT for sinus disease and facial pain. The International Headache Society (IHS) classifies migraine headache The IHS defines the intensity of pain with a verbal, four-point scale: Number Pain Annotations 0 NO 1 Mild does not interfere with usual activities 2 Moderate inhibits, but does not wholly prevent usual activities 3 Severe prevents all activities Migraine Definition IHS criteria: Migraine/aura (3 out of 4) – One or more fully reversible aura symptoms indicates focal cerebral cortical or brainstem dysfunction. – At least one aura symptom develops gradually over more than 4 minutes. – No aura symptom lasts more than one hour. – HA follows aura w/free interval of less than one hour and may begin before or w/aura. IHS Diagnostic criteria: migraine w/o aura – HA lasting for 4-72 hrs – HA w/2+ of following: Unilateral Pulsating Mod/severe intensity. Aggravated by routine physical activity. – During HA at least 1 of following N/V Photophobia Phonophobia History, PE, Neuro exam show no other organic disease. At least five attacks occur Migraine mechanism Neurovascular theory. – Abnormal brainstem responses. – Trigemino-vascular system. Calcitonin gene related peptide Neurokinin A Substance P Extracranial arterial vasodilation. – Temporal – Pulsing pain. Extracranial neurogenic inflammation. Decreased inhibition of central pain transmission. – Endogenous opioids. Important role in migraine pathogenesis. Mechanism of action in migraines not well established. Main target of pharmacotherapy. Aura Mechanism Cortical spreading depression – Self propagating wave of neuronal and glial depolarization across the cortex Activates trigeminal afferents – Causes inflammation of pain sensitive meninges that generates HA through central/peripheral reflexes. Alters blood-brain barrier. – Associated with a low flow state in the dural sinuses. Auras – Vision – most common neurologic symptom – Paresthesia of lips, lower face and fingers… 2nd most common – Typical aura Flickering uncolored zigzag line in center and then periphery Motor – hand and arm on one side Auras (visual, sensory, aphasia) – 1 hr Prodrome – Lasts hours to days… MIGRAINE WITH AURA DURING AURA: – VASOCONSTRICTION – HYPOPERFUSION DURING HEADACHE – VASODILATION – HYPERPERFUSION BUT: AURA SYMPTOM IS NOT CONSEQUENCE OF VASOCONSTRICTION INDUCED HYPOPERFUSION CUASE OF THE AURA: SPREADING DEPRESSION. THE VASOCONSTRICTION AND HYPOPERFUSION ARE CONSEQUENCES OF THE SPREADIND DEPRESSION AURA SPREADING DEPRESSION VASOCONSTRICTION, HYPOPERFUSION IMPORTANT TO KNOW! MIGRAINE WITH AURA IS A RISK FACTOR FOR ISCHAEMIC STROKE – THEREFORE PATIENTS SUFFERING FROM MIGRAINE WITH AURA SHOULD NOT SMOKE!!! SHOULD NOT USE ORAL CONTRACEPTIVE DRUGS!!! THE PROPROTION OF PATENT FORAMEN OVALE IN PATIENTS WITH MIGRAINE WITH AURA IS ABOUT 50-55%! (IN THE POPULATION IS ABOUT 25%). Is there a relationship between aura and patent foramen ovale ? Paradoxic emboli theory is not likely Shunting of venous blood to the arterial side could be the reason no breakdown of certain neurotransmitters (5HT) in the lung! Comorbidity could be also an explanation. However, closure of patent foramen ovale decreases the frequency of migraine attacks. BUT! Migraine is a benign disease. Please do not indicate closure of patent foramen ovale just because of migraine with aura! Migraine Subtypes Basilar type migraine – Dysarthria, vertigo, diplopia, tinnitus, decreased hearing, ataxia, bilateral paresthesias, altered consciousness. – Simultaneous bilateral visual symptoms. – No muscular weakness. Retinal or ocular migraine – Repeated monocular scotomata or blindness < 1 hr – Associated with or followed by a HA Migraine Subtypes Menstrual migraine Hemiplegic migraine – Unilateral motor and sensory symptoms that may persist after the headache. – Complete recover Familial hemiplegic migraine Migrainous vertigo Vertigo – sole or prevailing symptom. Benign paroxysmal vertigo of childhood. Prevalence 7-9% of pts in referral dizzy and migraine clinics. Not recognized by the IHS Diagnosis (proposed criteria) – Recurrent episodic vestibular symptoms of at least moderate severity. – One of the following: Current of previous history of IHS migraine. Migrainous symptoms during two or more attacks of vertigo. Migraine-precipitants before vertigo in more than 50% of attacks. – Response to migraine medications in more than 50% of attacks Clinical manifestations Clinical manifestations – Lateralized in severe attacks – 60-70% – Bifrontal/global HA – 30% – Gradual onset with crescendo pattern. – Limits activity due to its intensity. – Worsened by rapid head motion, sneezing, straining, constant motion or exertion. – Focal facial pain, cutaneous allodynia, GI dysfunction, facial flushing, lacrimation, rhinorrhea, nasal congestion and vertigo… Precipitating factors stress head and neck infection head trauma/surgery aged cheese dairy red wine nuts shellfish caffeine withdrawal vasodilators perfumes/strong odors irregular diet/sleep light Treatment Abortive – Stepped – Stratified – Staged Preventive Abortive Therapy Reduces headache recurrence. Alleviation of symptoms. Analgesics – Tylenol, opioids… Antiphlogistics – NSAIDs Vasoconstrictors – Caffeine – Sympathomimetics – Serotoninergics Selective - triptans Nonselective – ergots Metoclopramide Abortive care strategies Stepped – Start with lower level drugs, then switch to more specific drugs if symptoms persist or worsen. Analgesics – Tylenol, NSAIDs… Vasoconstrictors – sympathomimetics… Opioids (try to avoid) - Butorphanol Triptans – sumatriptan (oral, SQ, nasal), naratriptan, rizatripatan, zomatriptan. – Limited by patient compliance. Stratified – Adjusts treatment according to symptom intensity. Mild – analgesics, NSAIDs Moderate – analgesic plus caffeine/sympathomimetic Severe – opioids, triptans, ergots… – Severe sx treatment limited due to concomitant GI sx’s. Staged – Bases treatment on intensity and time of attacks. – HA diary reviewed with patient. – Medication plan and backup plans. Preventive therapy Consider if pt has more than 3-4 episodes/month. Reduces frequency by 40 – 60%. Breakthrough headaches easier to abort. Beta blockers Amitriptyline Calcium channel blockers Lifestyle modification. Biofeedback. Botox 51% migraineurs treated had complete prophylaxis for 4.1 months. 38% had prophylaxis for 2.7 months. Randomized trial showed significant improvement in headache frequency with multiple treatments. Conclusions Migraine is common but unrecognized. Keep migraine and its variants in the differential diagnosis. References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Landy, S. Migraine throughout the Life Cycle: Treatment through the Ages. Neurology. 2004; 62 (5) Supplement 2: S2-S8. Bailey, BJ. Head and Neck Surgery – Otolaryngology 3rd Edition. 2001. Pgs. 221-235. Bajwa, ZH, Sabahat, A. Pathophysiology, Clinical Manifestations, and Diagnosis of Migraine in Adults. Up To Date online. 2005. Lipton, RB, Stewart, WF, Liberman, JN. Self-awareness of migraine: Interpreting the labels that headache sufferers apply to their headaches. Neurology. 2002; 58(9) Supplement 6: S21-S26. Cady, RK, Schreiber, CP. Sinus headache or migraine?: Considerations in making a differential diagnosis. Neurology. 2002; 58 (9) Supplement 6: S10-S14. Perry, BF, Login, IS, Kountakis, SE. Nonrhinologic headache in a tertiary rhinology practice. Otolaryngology – Head and Neck Surg 2004; 130: 449-452. Daudia, AT, Jones, NS. Facial migraine in a rhinological setting. Clinical Otolaryngology and Allied Sciences. 2002; 27(6): 521-525. Spierings, EL. Migraine mechanism and management. Otolarynogol Clin N Am 36 (2003): 1063 – 1078. Avnon, y, Nitzan, M, Sprecher, E, Rogowski, Z, and Yarnitsky, D. Different patterns of parasympathetic activation in uni- and bilateral migraineurs. Brain. 2003; 126: 1660-1670. Stroud, RH, Bailey, BJ, Quinn, FB. Headache and Facial Pain. Dr. Quinn’s Online Textbook of Otolaryngology Grand Rounds Archive. 2001. http://www.utmb.edu/otoref/Grnds/HA-facialpain-2001-0131/HA-facial-pain-2001.doc Ondo, WG, Vuong KD, Derman, HS. Botulinum toxin A for chronic daily headache: a randomized, placebo-controlled, parallel design study. Cephalalgia 2004 (24): 60-65.