you can see
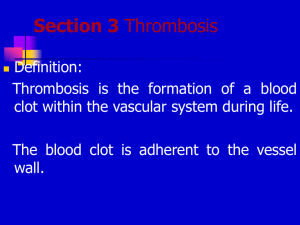
advertisement
CARDIOVASCULAR SYSTEM PATHOLOGY LABORATORY MICROSCOPY H – 3 Infective Endocarditis • A young drug addict who had injection marks on her arms was admitted to the hospital with high fever, chills, skin and mucosal petechia, and somnolance. • Blood culture was positive for S.aureus. • Despite vigorous treatment with antibiotics the patient died of sepsis and of acute congestive heart failure. • At autopsy large, friable, bulky, irregular masses were hanging from the free margins of mitral and aortic valves. • The microscopic sections prepared from these vegetations reveal masses of bacteria ( violet-colored granular amorpous masses ) covered with fibrin strands and inflammatory cells-mainly neutrophil leucocytes. • You can see the highly edematous leaflet tissue and myocardium infiltrated by bacteria. INFECTIVE ENDOCARDITIS bacteria inflammatory cells and fibrin H-3 myocardium • Masses of bacteria (violet colored, granular amorphous masses) in the vegetations • Fibrin strands • Inflammatory cells, mainly neutrophil leukocytes INFECTIVE ENDOCARDITIS bacteria myocardium H-3 H – 10 Myxoma • This section is prepared from a soft, translucent, irregularly lobulated mass removed from the left atrium of a 15 year-old girl. • The tumor had a gelatinous appearance and areas of hemorrhage on cut section. • Microscopic sections reveal stellate or elongated cells with oval nuclei, numerous small blood vessels, inflammatory cells, macrophages with hemosiderin pigment embedded in a pale, abundant matrix. • The tumoral mass is partly covered by intact endothelium. • Try to find areas of hemorrhage the fragment of the leaflet to which the tumor was attached MYXOMA blood vessels H-10 • Stellate or elongated cells with oval nuclei • Numerous small blood vessels • Inflammatory cells • Macrophages with hemosiderin pigment in a pale, abundant matrix MYXOMA stellate cells hemorrhage H-10 G – 7 Aneurysm and Thrombus • A 52 year-old man, who had recurrent episodes of embolisation of distal arteries of the lower extremities, was found to have an aneurysm of the abdominal aorta. • At operation the dilated segment of aorta between the renal arteries and iliac bifurcation was removed and replaced by synthetic graft. • The wall of this segment was extremely thin, with scattered atheromatous ulcers and attached mural thrombi. • In the microscopic slides you see the extreme thinning of the aortic wall and thrombus composed largely of pale staining finely granular masses (platelets) and eosinophilic strands (fibrin). • The luminal part of the thrombus consists of masses of erythrocytes. Try to find the area where the thrombus is attached to the aortic wall. • There are newly formed small blood vessels, macrophages, lymphocytes and fibroblasts in this area. ANEURYSM AND THROMBUS thrombus • Extreme thinning of the aortic wall • Thrombus composed largely of pale staining finely granular masses (platelets) and eosinophilic strands (fibrin) • Erythrocytes in the luminal part of thrombus G-7 aortic wall erythrocytes ANEURYSM AND THROMBUS • In the area where the thrombus is attached to the aortic wall: you can see; • • • • G-7 Inflammatory cells and fibroblasts newly formed small blood vessels macrophages Lymphocytes fibroblasts G – 10 Medial degeneration and dissecting aneurysm • A 53 year-old hypertensive man complaining of sudden onset of severe chest pain was admitted to the emergency room. • Although the patient had signs of shock and acute left-sided heart failure, his blood pressure was elevated. • After angiography, he was immediately operated on dissecting aneurysm of ascending aorta. • An intimal tear was found 7 cm above the aortic valve. The blood filled in, dissecting the media. • The dissecting hematoma reached proximally to the aortic valve and distally to the great arteries. • In the microscopic slides, the media of the aorta shows reduced cellularity, destruction of its normal lamellar pattern and small cleft like cystic poorly defined spaces filled with slightly basophilic material ( cystic medial necrosis ). G – 10 Medial degeneration and dissecting aneurysm • The blood that filled the dissecting aneurism was lost during tissue processing, but you can see the tear and seperation between the middle and outer thirds of media. • The patient also had atherosclerosis, and you can see an intimal plaque composed of lipid and lipid-laden histiocytes, necrotic cells, spindle cells (smooth muscle cells) capped by a thin fibrous tissue. MEDIAL DEGENERATION Reduced cellularity G-10 Tear/Seperation • Reduced cellularity and destruction of normal lamellar pattern in the media of aorta • Small cleft like cystic poorly defined spaces filled with basophilic material (cystic medial necrosis) • Seperation between the middle and outer thirds of media G – 15 Hemangioma • This section is prepared from a red elevated nodule from the skin of a 3-year-old child. • Beneath a thinned epidermis, in the dermis, you see an unencapsulated tumor composed of aggregations of different sized capillaries sepatared by septa of connective tissue stroma. • Some capillaries are formed of endothelial cell buds and have no visible lumina. • Some capillaries are lined by plump endothelial cells and have small lumina; others make up larger channels filled with blood. • You can see hemosiderin pigment, scattered inflammatory cells and fibrosis in the stroma. HEMANGIOMA epidermis • Beneath the thin epidermis, in the dermis, you can see an unencapsulated tumor • Different sized capillaries Capillaries are seperated by septa of connective tissue stroma Some capillaries have small lumina whereas larger ones are filled with blood • G-15 • capillary hemangioma HEMANGIOMA • Some capillaries are lined by plump endothelial cells • You can see; • • Hemosiderin pigment Scattered inflammatory cells Fibrosis in the stroma G-15 capillaries • Plump endothelial cells G – 21 Vasculitis • This slide is prepared from a loop of infarcted small intestine macroscopically showing dark hemorrhagic discoloration. • The patient was a 75-year-old woman with the clinical diagnosis of acute mesenteric ischemia. • Histologically there is mucosal edemai inflammatory infiltration (especially mononuclear cells), submucosal vascular proliferation, telangiectasis and intramural necrosis. G – 21 Vasculitis • Now try to see pathology in the small caliber muscular arteries. • There is fibrinoid necrosis which extents in some to involve the full thickness of the arterial wall. • Besides endothelial cell swelling you can see numerous leucocytes, including neutrophils, eosinophils and mononuclear cells that present in and around the vessel wall. Submucasal vascular proliferation VASCULITIS Edema in the intestinal mucosa G-21 • Mucosal edema • Inflammatory infiltration (especially mononuclear cells) • Submucosal vascular proliferation • Telengiectasis • Intramural necrosis VASCULITIS Intramural necrosis Telengiectasia Inflammatory cell infiltration G-21 VASCULITIS • In the small caliber musculary arteries, you can see “fibrinoid necrosis” which extents in some to involve the full thickness of the arterial wall. • Besides endothelial cell swelling you can see Leucocytes(neutrophils, eosinophils and mononuclear cells that present in and around the vessel wall. Inflammation • G-21 Fibrinoid necrosis G – 22 Atherosclerosis • A 68-year-old male patient who had a history of uncontrolled diabetes mellitus presented with gangrene of the lower extremity. • Amputation was performed. • This slide is prepared from arteria tibialis posterior, and stained with EVG, which stains elastic fibers black. • The microscopic sections reveal a plaque which consists of dense fibrous tissue (brown), much of it is acellular and hyaline. • The internal elastic lamina is wrinkled and reduplicated to form a second thinner elastic lamina. • You see areas of thinner elastic lamina and the thickened intima ATHEROSCLEROSIS Fibrous plaque G-22 Reduplication • This slide is stained with EVG • EVG stains elastic fibers black • This section reveals a plaque which consists of dense fibrous tissue (brown) much of it is acellular and hyaline ATHEROSCLEROSIS Thickened intima G-22 Reduplication • The internal elastic lamina is wrinkled and reduplicated to form a second thinner elastic lamina • You see areas of thinner elastic lamina and the thickened intima