phys(tut+Imp)1st mid ( 1updated)
advertisement
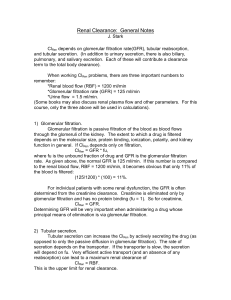
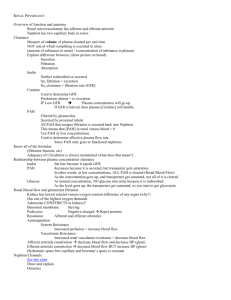
PHYSL Important notes , tutorial 1st 5 lecs mid1 LEC 1 Function of kidney “ slide 4+5” : • Excretion • Homeostatic function • Biosynthesis/Metabolism Type of nephron : THE FILTRATION MEMBRANE: 1. Capillary Endothelium: negative charges that restrict the passage of plasma proteins 2. Basement Membrane: mesangial cells are located between the basal lamina and the endothelium. 3. Podocytes (Epithelium) : foot-like processes all layers of glomerular capillary membrane have negative charge provide a barrier to the filtration of plasma proteins. Juxtaglomerular Apparatus: “ slide 23 “ • The Macula Densa: Detect & respond to changes in the sodium chloride levels in the distal tubule of the kidney. • Juxtaglomerular Cells : secrete renin LEC 2 Glomerular Filtration: The first step in urine formation is the Glomerular filtration during which, large quantity of water and solutes pass through the filtration membrane from the blood into the Bowman’s Capsule due to pressure gradient. Abnormal value : Microalbuminuria is 30–300 mg/24 hours Macroalbuminuria is 300mg/24 hours Factors affecting GFR: • Changes in renal blood flow • Changes in glomerular capillary hydrostatic pressure – Changes in systemic blood pressure – Afferent or efferent arteriolar resistance • Changes in hydrostatic pressure in Bowman’s capsule – Ureteral obstruction – Edema of kidney inside tight renal capsule • Changes in concentration of plasma proteins: – Dehydration – Hypoproteinemia, etc. • Changes in Kf – Changes in glomerular capillary permeability – Changes in effective filtration surface area Glomerular Capillary Hydrostatic Pressure (PG): “slide 15” It is the primary means for physiologic regulation of GFR. Increase PG raises GFR, and vice versa. It is determined by three variables: Arterial Pressure Afferent Arteriolar Resistance Efferent Arteriolar Resistance. LEC 3 Remember • Loop of Henle ascending : electrolyte • Loop of Henle descending : only water • Proximal convoluted tubule PCT: glucose and amino acid 100% reabsorped LEC 4 Remember • Level of glucose in blood will cause TM and it’ll cause threshold • Threshold = 180-200 • The main function of urea is controlling water balance and concentration of urine • Ca and phosphate influenced by PTH Lec 5 Most important substances secreted by the tubules Is H+and K+ • H+ • • Important in regulating acid-base balance Secreted in proximal, distal, and collecting tubules • K+ • • Keeps plasma K+ concentration at appropriate level to maintain normal membrane excitability in muscles and nerves Secreted only in the distal and collecting tubules under control of aldosterone During acidosis H+ secretion is increase lead to retention of K+. small increase in plasma potassium will cause cardiac arrhythmias, and higher concentrations can lead to cardiac arrest or fibrillation. small loss of potassium from the extracellular fluid could cause severe hypokalemia. rapid and appropriate compensatory response mechanism is vital to avoid dangerous Hyperkalemia(with bradycardia) or Hypokalemia (with tachycardia ) Factor effecting secretion : slide 13+14+17 • Diet • Aldosterone • Acid base balance • RAAS will reabsorb Na+ and excrete K+ – Renin–Angiotensin–Aldosterone system (RAAS) – Increase of RAAS cause hypertension. – RAAS is also responsible for fluid retention and EDEMA occurring in congestive heart failure. – Angiotensin Converting Enzyme inhibitor – ACE inhibitor drugs are used for hypertension and congestive heart failure • diuretics will block the Na+\K+ pump • PAH is used to diagnose renal blood flow , cus it’s not reabsorbed • NSAID + Aspirin cause tubular damage, will cause in large dose acute renal failure Tutorial For all the 5 lecs Lec1 1-Biosynthesis/Metabolism FUNCTIONS OF KIDNEYS? – Renin secretion – Erythropoietin – Activation of Vitamin D> Calcitriol (1,25 DHCC) – Other substances: • Prostaglandin, • Adenosine… etc .. But the 1st 3 are most important 2-Homeostatic function of kidney ? – acid-base balance – Osmolality and volume of ECF – blood pressure. – water and electrolyte balances. – Plasma ions concentration. 3-Excretion function of kidney ? – metabolic end product, e.g. urea – foreign substances, e.g. drugs, toxins Parts of Nephron? 4-What is peritubular capillaries? Around the tubules and its function is to reabsorb substances from tubules 5-What is vasa recta ? straight capillaries in the medulla 6-Difference b\w cortical and juxta medullary nephrons ? 7-What are the layers of Glomerulus? 1. Capillary Endothelium 2. Basement Membrane 3. Podocytes (Epithelium) 8-What are the layers of Bowmans Capsule? – Visceral > Podocytes ( which is the last layer of Glomerulus) – Parietal 9-What is the specialty\feature of Capillary Endothelium? Fenestrations =pores 10-What is the specialty\feature of Basement Membrane? negatively charged 11-What is the specialty\feature of Podocytes ? foot-like processes which helps in interlocking with other cells (gaps) to have a better surface area 12-What are the layers of Filtration Membrane? 1. Endothelium 2. Basement Membrane 3. Podocytes 13-What is Juxtaglomerular Apparatus\ or what is the purpose of them? Regulatory center for nephron 14-What are the Cells in JG Apparatus? The Macula Densa Where located? DCT What are they ? modified cells of DCT What is the function? Detect & respond to changes in the sodium chloride levels in the distal tubule of the kidney. Juxtaglomerular Cells: also called granular cells Where present? wall of afferent arteriole endothelium What are they ? Modified cells of endothelium What is the function? secrete renin Which cells have granules? Juxtaglomerular cells Extra Glomerular Mesangial Cells B\W arteries and tubules 15 –Where’s the JG Apparatus Cells present? Wall of efferent artery 16-What is the 1st step in urine formation ? 1.Glomerular filtration – GF Then the 2nd and 3rd steps .. 2. Tubular reabsorption - TR 3. Tubular secretion - TS Lec 2 17-What are the substances that are not filtered ? – Blood cells – Protein – Protein-bound molecules (calcium, fatty aids, amino acids) 18-What is the Definition Glomerular Filtration Rate (GFR)? – It is the Volume of plasma filtered by all nephrons of both kidneys per unit time. 19-What is Normal GFR value? 125ml/min or 180L/day. 20-What are the factors Determine the GFR? – NET FILTRATION PRESSURE which is : Sum of the hydrostatic and colloid osmotic pressures across the glomerular membrane – Capillary Filtration Coefficient (Kf): Surface Area “Membrane Permeability”= thickness 21-what is Net filtration Pressure value ?: 10mmHg And it’s consisting of 4 pressures Glomerular hydrostatic pressure Glomerular colloid osmotic pressure Bowman’s capsular hydrostatic pressure Bowman’s capsular colloid osmotic pressure 22- 2 pressures helps in filtration ? – – Glomerular hydrostatic pressure Bowman’s capsular colloid osmotic pressure 23-Which pressure is used by body primarily for physiological regulation of GFR? | What’s primary mean of physiological GFR? Glomerular hydrostatic pressure -Hydrostatic pressure could affected by ? Renal blood flow 24- 2 pressures Opposing filtration? – Glomerular colloid osmotic pressure – Bowman’s capsular hydrostatic pressure • So all 7 factors affecting the GFR? 1. 2. 3. 4. 5. 6. 7. Glomerular hydrostatic pressure Glomerular colloid osmotic pressure Bowman’s capsular hydrostatic pressure Bowman’s capsular colloid osmotic pressure Surface Area “Membrane Permeability”= thickness Renal blood flow 25-How the regulation of GFR is done?| the methods of regulation in GFR? 1. Extrinsic mechanisms 2. Intrinsic mechanisms by Autoregulation 26-What are the Extrinsic mechanisms? • sympathetic nervous system(autonomic) • Baroreceptor reflex (mainly autonomic also) 27-What is the Intrinsic mechanisms ? • Myogenic mechanism • Tubuloglomerular feedback (TGF) 28-What is Myogenic mechanism? increase ↑ pressure in capillary, the capp will be stretched , the stretching will cause entry of ca into smooth muscle = constriction of capillary So ↑stretch = ↓ 𝐺𝐹𝑅 29-What is Tubuloglomerular feedback (TGF)? It’s the func of Juxtaglomerular Apparatus Detects how much Na+ loss or reabsorbed in blood ..will make it balanced 30- what is Effect of Afferent Arteriolar Constriction of FGR? ↓GFR, ↓Renal Blood Flow 31-What is the Effect of Efferent Arteriolar Constriction of FGR? ↑ GFR, ↓ Renal Blood Flow 32-What is the Filtration Fraction (FF) and how much is it ? ratio of the GFR to the renal plasma flow (GFR/TRPF). 33-How much of blood flow goes to kidney= renal blood flow ? – 20-25% of total cardiac output. = 1 L/min 34-Out of that how much plasma supply to kidney ? • 625 ml • Out of that 125 ml is filtered 35-So Filtration fraction normal value ? (GFR/TRPF) = 0.2( 20%) Measurement of GFR: • Characteristic of substance used for measurement: – 1- Freely filtered (not reabsorbed not secreted) – 2- Not metabolized by the kidney – 3- Not toxic and stable – 4- Not bound to plasma protein – 5- Does not change renal plasma flow 36-Substance used to Measurement of GFR? – Inulin lec3 37-Transport mechanism used in reabsorption ? active Primary active Sodium-potassium pumps in basolateral membrane. passive Secondary active co-transport (glucose, amino acids, fatty acid) counter-transport (K+, H+) 38-What are the Substance utilize for co-transport for many substances in renal tubule ? Na+ (sodium ) -GLUT depends on ? Facilitated diffusion 39-Glucouse utilizes which type of transport? co-transport or 2ry active transport 40- H+ ion utilizes which type of transport ? mostly counter-transport 41-Common Substances Reabsorbed in PCT: – – – – – – – – Sodium Chloride Glucose Water Amino acid Bicarbonate Phosphate Urea 65% 50% 100% 65% 100% 90% 42-What is the specialty of Loop of Henle? descending limb: highly permeable to water Ascending limb: only permeable to electrolyte and impermeable to water. 43-What is the specialty Late DCT and Cortical Collecting Tubule? Hormone regulation - Which Hormone can control the Permeability of substances in Water? Anti diuretic Hormone (ADH) or Vasopressin 44-What are the type of cells present in the segment ? Principal cells +Intercalated cells 45-What is the function of Principal cells ? Have receptors for hormones like aldosterone , help in reabsorption of electrolytes 46-What is the function of Intercalated cells? Acid base balance , control reabsorb and excretion of H+ ions and Bicarb 47-Medullary Collecting Duct importance? – Last step where any change can occur into the tubular fluid , after that the tubular fluid is passed on as urine 48-What are the factors or mech that help in reabsorption? – Mostly hormones (aldosterone, angiotensin II,(ADH)… etc.) – Then same forces, pressures in GFR 49- What is pressure natriuresis ? ↑ blood pressure, ↑ loss of NA+ 50- What is Pressure diuresis ? ↑ blood pressure , ↑ loss of H2O Na+ sodium 51-Where’s reabsorbed? in the tubule (including aescending limb of Loop of Henle) except descending limb of Loop of Henle 52-What’s the effect of aldosterone on Na+? ↑ NA reabsorption 53-What’s the effect of aldosterone on K+? ↑ K+ excretion Aldosterone : صائد الصوديوم طارد البوتاسيوم 54-What’s the effect of Na on urea and chloride ? ↑ their reabsorption by passive transport Just remember that Tubular Reabsorption – Sodium: • Proximal convoluted tubule 65 - 67% • Loop of Henle (thick ascending limb) 25 % • Distal and Collecting Tubule 8% Tubular Reabsorption – Water: • Proximal convoluted tubule (PCT) – 60-70%. It is passive. • Loop of Henle(Descending Limb) – 15%. • DCT and CT – 20%. DCT – 5%. CT – 15%. • In DCT and CT, water is reabsorbed under the action of ADH (Anti-Diuretic Hormone) or Vasopressin. Lec 4 55-How’s glucose reabsorbed? Co-transportation or 2ry active transport 56-Whare glucose is reabsorbed? PCT 57-How much of glucose is reabsorbed by PCT? 100% 58-What is Tubular Maximum (Tm) of glucose ? the maximum amount of glucose which can be reabsorbed after that point glucose appears in urine 59-Normal value of Tm? 375 mg/minute. 60-What is the renal threshold concentration of glucose at which glucose will appear in the urine 61-Normal value or the renal threshold ? 180mg % - 200mg %. 62-Urea reabsorbed? proximal tubule 63-Urea secreted ? loop of Henle. 64-reabsorbed again in? the medullary collecting duct 65-Under the influence of? Hormones 66-What is Obligatory Urine Volume? minimum amount of urine which has to be formed in excretion of harmful substance each day 67-Normal value of Obligatory Urine Volume? 0.5 L/day Lec 5 68-What are the substance important for secretion: H+ and K+ 69-Factors affect secretion? 1. Diet 2. Aldosterone 3. Acid base balance 70-What is the affect of H+ ion on K+ secretion ? – Whenever Acidosis (↑H+) , K+ retention occurs , so hyperkalemia will occur Normal values GFR value: 125ml/min or 180L/day Net filtration Pressure value: 10mmHg Renal blood flow : 20-25% of total cardiac output. = 1 L/mi Plasma supply to kidney: 625 ml Filtration fraction normal value: 0.2( 20%) Tm: 375 mg/minute. Renal threshold: 180mg % - 200mg %. Obligatory Urine Volume: 0.5 L/day