MDCT in ACS (RSNA 2010)
advertisement

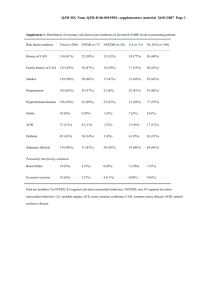
David Tso, BSc Nima Kashani, BSc Arash Eftekhari, MD Anja Reimann, MD Chris Davison, MBChB Ahmed Albuali, MD Savvas Nicolaou, MD Vancouver General Hospital University of British Columbia Objectives To review the imaging modalities available in assessing patients with acute coronary syndrome (ACS) To summarize the clinical trials investigating Multi-detector CT (MDCT) in diagnosing ACS To discuss the benefits of MDCT in assessing ACS with regards to cost, time to diagnosis, outcomes To discuss the role of a Triple-Rule-Out Protocol in evaluation of chest pain syndromes Cause for concern ACS is associated with increase in cardiac death and subsequent MI 2-8% of patients with ACS are misdiagnosed and inappropriately discharged home, which is associated with doubling mortality rate Important to differentiate serious causes of chest pain from less serious causes Angina Pulmonary embolism Aortic dissection Christenson J, et al. CMAJ 2004 Jun 8;170(12):1803-7 Chinnaiyan KM, Raff GL, Goldstein JA. Cardiol Clin. 2009 Nov;27(4):587-96. White CS, Kuo D. Radiology. 2007 Dec;245(3):672-81. Definition of ACS Constellation of clinical symptoms that are compatible with acute myocardial ischemia STEMI & NSTEMI Unstable Angina (UA) UA/NSTEMI ECG ST-segment depression or prominent T-wave inversion +/- Positive biomarkers of myocardial necrosis J Am Coll Cardiol. 2007 Aug 14;50(7) Standard of Care Clear evidence of STEMI Suggestive clinical history & exam ST-elevation on ECG Positive Cardiac biomarkers Consider immediate reperfusion therapy ○ Fibrinolysis ○ Percuntaneous coronary intervention Extremely low probability of ACS Discharge J Am Coll Cardiol. 2007 Aug 14;50(7) Management based on work-up Chest pain indeterminate at initial work-up Atypical clinical history & exam ECG showing only non-specific T-wave changes Normal biomarkers Further diagnostic evaluation required Rest myocardial perfusion imaging w/ SPECT Stress echocardiography MRI MDCT White CS, Kuo D. Radiology. 2007 Dec;245(3):672-81. J Am Coll Cardiol. 2007 Aug 14;50(7) SPECT Benefits vs. Limitations BENEFITS Highly sensitive 90-100% Moderate specificity 60-78% High negative predictive value 97-100% Good prognostic value LIMITATIONS High radiation exposure Nuclear medicine near ED Only assesses CAD and not other causes Time intensive Potential for false negatives Provides no anatomical information Reza Fazel et al. N Engl J Med, 27 Aug 2009, 361(9):849. White CS, Kuo D. Radiology. 2007 Dec;245(3):672-81. Echo: Benefits vs. Limitations BENEFITS No radiation exposure Similar sensitivity and specificity as radionuclide perfusion imaging Portability LIMITATIONS Off hours availability False-negative results in patients with small myocardial infarctions or unstable angina May fail to identify nonstructural infarcts Might have ischemia but no wall abnormality Limited anatomical information White CS, Kuo D. Radiology. 2007 Dec;245(3):672-81. Cardiovascular Magnetic Resonance Accepted indications for assessment by CMR Congenital heart disease Great vessels Acquired myocardial & pericardial disease CAD Role in ACS less well established CMR may be useful in the acute setting as a problem solving tool Patients with suspect ACS but no angiographic evidence of coronary artery stenosis Utility in negative or equivocal findings on CT Establish degree of myocardial necrosis after establishing MI Scirica BM. J Am Coll Cardiol. 2010 Apr 6;55(14):1403-15. Lockie et al, Circulation. 2009;119:1671-1681 MDCT in the Acute Care Setting Provides excellent spatial resolution provides superior information of anatomy Provides functional information through blood perfused volume and stress protocols Ability for plaque analysis Appropriate use of Triple-Rule-Out Protocol can explore other differential diagnoses for chest pain MDCT imaging protocols incorporated into ACS workup demonstrates savings in time to diagnosis, costs while providing good patient outcomes CT Angiography Direct visualization of coronary arteries was previously limited to invasive techniques I.e. coronary angiography Introduction of Multi-detector CT (MDCT) in noninvasive evaluation of CAD has become possible MDCT performs well in detection of significant coronary stenosis Sensitivity = 82-95% Specificity = 82-98% Presence of coronary calcifications in patients with ACS shown to be predictive of future cardiac events J Am Coll Radiol. 2006 Oct;3(10):751-71. MDCT: Occluded RCA Benefits of MDCT Performs well in ruling out CAD for low to intermediate probability of CAD High negative predictive values Patients with normal scan may be discharged safely CCTA may not provide additional relevant diagnostic information in patients with a high pretest probability for CAD May need further investigations because of low positive predictive value Test of choice = Conventional coronary angiography MDCT Limitations Image quality suffers from fast heart rate Requires premedication with β-blockers Arrhythmias, ectopy, or ECG artifacts result in degradation of image quality ECG-gating critical to coronary imaging Radiation dose to patient Provides anatomic information, but not physiologic data Chinnaiyan KM, et al. Cardiol Clin. 2009 Nov;27(4):587-96. MDCT: Cost & time to diagnosis Study n SOC MDCT Difference P-value May et al. AJR 2009 53 $7,597 $6,153 $1,444 P<0.001 Time to discharge 25.4 hours 14.3 hours 11.1 hours P<0.001 749 $3,458 $2137 $1,321 P<0.001 Time to diagnosis 6.2 hours 2.9 hours 3.3 hours P<0.0001 197 $1,872 $1,586 $286 P<0.001 Time to diagnosis 15.0 hours 3.4 hours 11.6 hours P<0.001 Chinnaiyan et al. AHA 2009 Goldstein et al. JACC 2007 1. Using CCTA vs. standard of care protocols (i.e. myocardial perfusion imaging) can diagnosis patients faster 2. Cost savings come from reduce time in hospital and reduced need for additional Goldstein et al. J Am Coll Cardiol 2007;49:863–71 tests from a negative CCTA exam May et al. AJR 2009; 193:150–154 Ruling out Non-cardiac Causes Routine CT acquisition has ability to examine other non-cardiac structures e.g. Aorta, pulmonary arteries Possible modality to rule out potentially fatal causes of chest pain CAD Acute aortic dissection Pulmonary embolism Triple rule out (TRO) protocol can allow in rapid discharge of patients with low to moderate ACS risk Chinnaiyan KM, et al. Cardiol Clin. 2009 Nov;27(4):587-96. Triple rule out: atypical chest pain Diagnosis = pulmonary embolism TRO – Pericardial Effusion 40 yo female Atypical chest pain SOB Diagnosis = Lymphoma resulting in pericardial effusion TRO – Pulmonary edema Diagnosis = Mitral Valve Prolapse Whole Body Rule-out Diagnosis = Aortic Dissection Dedicated CTA vs. Triple-Rule-Out Investigates coronary arteries only Greater spatial resolution of coronary arteries Less radiation Less contrast Time = 8 secs Craniocaudal Investigates CAD, PE, Aortic dissection Lesser spatial resolution of coronary arteries More radiation More contrast Time = 15 secs Caudalcranial Dedicated CTA Triple-Rule-Out Heart perfused volume imaging Myocardial blood pool analyzed by assessing iodine content within myocardium Using unique X-ray absorption characteristics of iodine at different kV levels Color-coded “iodine maps” represent myocardial blood pool Perfused myocardium contains iodine vs. an infarct which will not have iodine uptake Single cardiac CTA exam that examines both coronary anatomy and myocardial perfusion is promising Rocha-Filho et al. Radiology: Volume 254: Number 2—February 2010 Ruzsics et al. Eur Radiol. 2008 Nov;18(11):2414-24. Dual energy CT + adenosine stress Recent studies show results from adenosine-mediated CT perfusion imaging is comparable to SPECT– myocardial perfusion in detecting perfusion abnormalities Allow for comparison of rest and stress DECT in detecting perfusion deficits Protocol allows for quantification of iodine DECT adenosine stress protocol enables examination of anatomy and function in a single investigation Radiation exposure equivalent to SPECT Regadenoson = selective α2a receptor agonist Coronary vasodilator Less side effects than adenosine Easier to use iv bolus 5cc(0.4 mg) with no weight adjustment CTA + CT Heart Perfused Blood Volume Combination of cardiac CT angiography and CT perfusion in a single examination improved diagnostic accuracy Comparable to SPECT–MPI For stenosis > 50% luminal narrowing Combination shown to increase PPV by more than 20% after incorporation of CT perfusion analysis over CTA alone (66% to 86%) Myocardial hypoenhancement seen on MDCT has potential in evaluating CAD without additional cost in radiation dose or contrast load. Kachenoura N, et al. Am J Cardiol. 2009 Jun 1;103(11):1487-94. Rocha-Filho et al. Radiology: Volume 254: Number 2—February 2010 DECT - Coronary artery occlusion Perfusion defects at rest anterior LAD posterior RCA lateral LCx 100% iodine overlay 100 kV (Stress) 50:50 heart perfused volume (Stress) Heart perfused blood volume at rest 50:50 100% iodine overlay DE – Heart blood perfused volume Stress Rest Perfusion Perfusion Quantification of Iodine Acute chest pain 1. High Risk Low-tointermediate risk No known CAD (positive EKG ± cardiac enzymes) 2. Known CAD MDCT/ = MDCT DECT Shop One Stop Strong clinical suspicion for CAD ± PE or AD Guidelines-based Standard of care Intermediate/ Non-diagnostic Abnormal Very low risk Normal Scan Outpatient follow-up Triple Triple Rule-Out Rule-Out Stress testing Abnormal Invasive Angiography Normal Discharge Acute Chest Pain Algorithm Chinnaiyan KM, et al. Cardiol Clin. 2009 Nov;27(4):587-96. Conclusions MDCT has a role as a multipurpose triaging tool in assessing patients with atypical chest pain MDCT has been proven in clinical trials to have great accuracy in ruling out ACS MDCT in combination with stress perfusion may yield better diagnostic accuracy Appropriate use of Triple-Rule-Out Protocol can explore other differential diagnoses for chest pain MDCT imaging protocols incorporated into ACS workup demonstrates savings in time to diagnosis, costs while providing good patient outcomes Protocol Triple Rule Out FLASH GATED Spiral Triple Rule Out Gated FLASH Cardiac 65 BPM DS SPIRAL Cardiac mAs (Tube A) kV 120 Kernel B Kernel B Kernel B Kernel B for Collimation Pitch Rot Time CTDI vol Multiphasic 350 B26(Cardiac) 0.6mm x 0.4mm 370 B26(Cardiac) 0.6mm x 0.4mm 450 B26(Cardiac) 0.6mm x 0.4mm 400 B26(Cardiac) 0.6mm x 0.4mm B36 3mm x 1.5mm B70 3.0mm x 1.5mm B36 3mm x 1.5mm B70 3.0mm x 1.5mm B36 3mm x 1.5mm B70 3.0mm x 1.5mm B36 3mm x 1.5mm B25 1mm x 0.7mm B35 1.5mm x 1.0mm B35 1.5mm x 1.0mm 128 mm x 0.6mm 3.2 0.28 6.05 128 mm x 0.6mm 0.23 0.28 32.84 128 mm x 0.6mm 3.4 0.28 7.42 128 mm x 0.6mm 0.23 0.28 53.5 1. CTA scans use Test Bolus of 6.5cc/sec for 65 cc isovue 370, followed by a 60/40 split bolus of saline/isovue 370, followed by 40cc of pure saline. 2. Peak HU for contrast is determined at ascending aorta, and 5-6 sec is added for delay time for scan after contrast flow is started at the R.ACF