Hypertonic Saline in the Treatment of Sepsis
Hershberger, T. and Nibblett, B.
Ross University School of Veterinary Medicine
Key Points
Discussion
A dog presenting with septic shock secondary to severe bite injuries
may benefited from the administration of hypertonic saline solution.
Potential benefits of hypertonic saline include:
• decrease in endothelial cell edema
• increased cardiac contractility
• decreased peripheral vascular resistance
• significant intravascular volume expansion with a synergistic
effect with concurrent colloid administration
• immunomodulation.
Septic
shock is a severe form of sepsis that is characterized by
.
organ dysfunction and failure with refractile hypotension1 and is
associated with a poor prognosis.
Systemic inflammatory response syndrome (SIRS) = imbalance
between pro-inflammatory and anti-inflammatory mediators 2
Inflammatory cells involved: macrophages, neutrophils, endothelium
and platelets
Widespread vasodilation and increased capillary permeability induce
hypotension, peripheral edema and cellular edema
Hypercoagulative state: disseminated intravascular coagulation
(DIC) with microclots that may lodge in the microvasculature.
Hypoxia: tissue injury and organ dysfunction multiple organ
dysfunction syndrome, or MODS3.
Case Summary
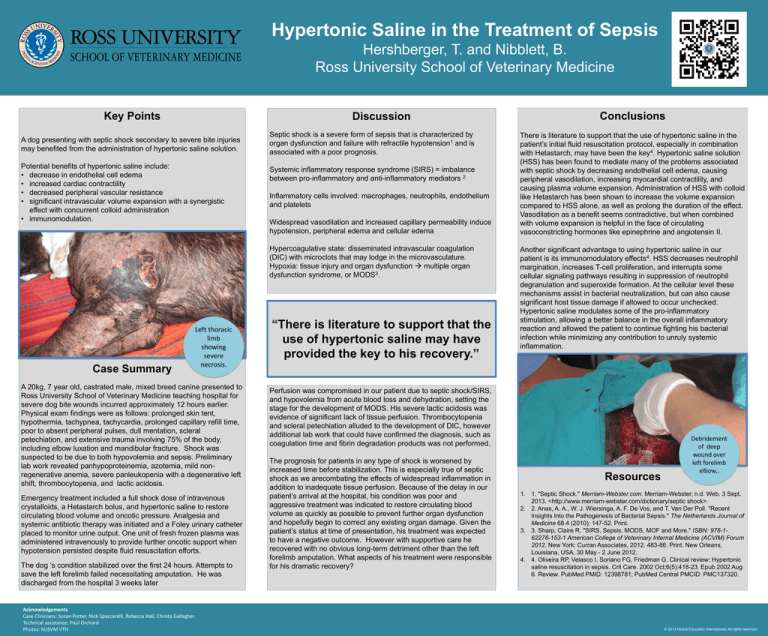
Left thoracic
limb
showing
severe
necrosis.
A 20kg, 7 year old, castrated male, mixed breed canine presented to
Ross University School of Veterinary Medicine teaching hospital for
severe dog bite wounds incurred approximately 12 hours earlier.
Physical exam findings were as follows: prolonged skin tent,
hypothermia, tachypnea, tachycardia, prolonged capillary refill time,
poor to absent peripheral pulses, dull mentation, scleral
petechiation, and extensive trauma involving 75% of the body,
including elbow luxation and mandibular fracture. Shock was
suspected to be due to both hypovolemia and sepsis. Preliminary
lab work revealed panhypoproteinemia, azotemia, mild nonregenerative anemia, severe panleukopenia with a degenerative left
shift, thrombocytopenia, and lactic acidosis.
Emergency treatment included a full shock dose of intravenous
crystalloids, a Hetastarch bolus, and hypertonic saline to restore
circulating blood volume and oncotic pressure. Analgesia and
systemic antibiotic therapy was initiated and a Foley urinary catheter
placed to monitor urine output. One unit of fresh frozen plasma was
administered intravenously to provide further oncotic support when
hypotension persisted despite fluid resuscitation efforts.
The dog ‘s condition stabilized over the first 24 hours. Attempts to
save the left forelimb failed necessitating amputation. He was
discharged from the hospital 3 weeks later
Acknowledgements
Case Clinicians: Susan Porter, Nick Spaccarelli, Rebecca Hall, Christa Gallagher
Technical assistance: Paul Orchard
Photos: RUSVM VTH
“There is literature to support that the
use of hypertonic saline may have
provided the key to his recovery.”
Conclusions
There is literature to support that the use of hypertonic saline in the
patient’s initial fluid resuscitation protocol, especially in combination
with Hetastarch, may have been the key4. Hypertonic saline solution
(HSS) has been found to mediate many of the problems associated
with septic shock by decreasing endothelial cell edema, causing
peripheral vasodilation, increasing myocardial contractility, and
causing plasma volume expansion. Administration of HSS with colloid
like Hetastarch has been shown to increase the volume expansion
compared to HSS alone, as well as prolong the duration of the effect.
Vasodilation as a benefit seems contradictive, but when combined
with volume expansion is helpful in the face of circulating
vasoconstricting hormones like epinephrine and angiotensin II.
Another significant advantage to using hypertonic saline in our
patient is its immunomodulatory effects4. HSS decreases neutrophil
margination, increases T-cell proliferation, and interrupts some
cellular signaling pathways resulting in suppression of neutrophil
degranulation and superoxide formation. At the cellular level these
mechanisms assist in bacterial neutralization, but can also cause
significant host tissue damage if allowed to occur unchecked.
Hypertonic saline modulates some of the pro-inflammatory
stimulation, allowing a better balance in the overall inflammatory
reaction and allowed the patient to continue fighting his bacterial
infection while minimizing any contribution to unruly systemic
inflammation.
Perfusion was compromised in our patient due to septic shock/SIRS,
and hypovolemia from acute blood loss and dehydration, setting the
stage for the development of MODS. His severe lactic acidosis was
evidence of significant lack of tissue perfusion. Thrombocytopenia
and scleral petechiation alluded to the development of DIC, however
additional lab work that could have confirmed the diagnosis, such as
coagulation time and fibrin degradation products was not performed.
The prognosis for patients in any type of shock is worsened by
increased time before stabilization. This is especially true of septic
shock as we arecombating the effects of widespread inflammation in
addition to inadequate tissue perfusion. Because of the delay in our
patient’s arrival at the hospital, his condition was poor and
aggressive treatment was indicated to restore circulating blood
volume as quickly as possible to prevent further organ dysfunction
and hopefully begin to correct any existing organ damage. Given the
patient’s status at time of presentation, his treatment was expected
to have a negative outcome. However with supportive care he
recovered with no obvious long-term detriment other than the left
forelimb amputation. What aspects of his treatment were responsible
for his dramatic recovery?
Resources
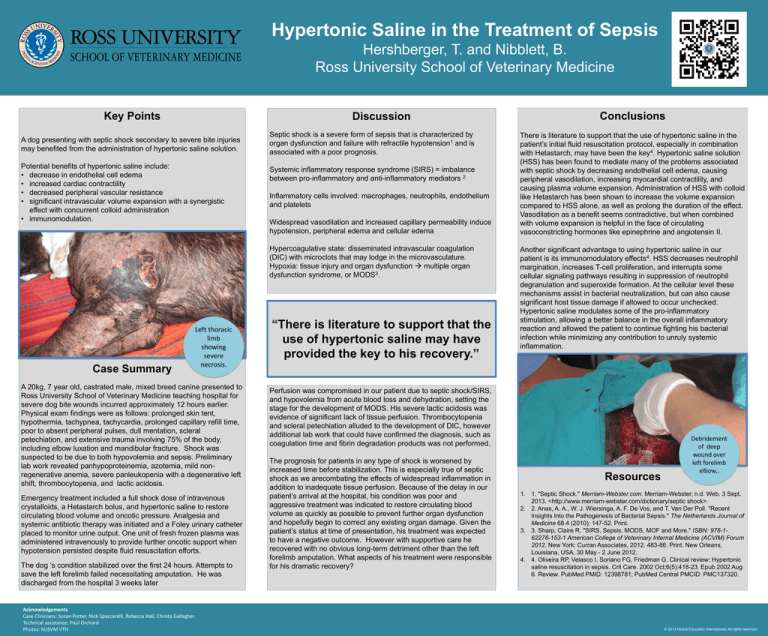
Debridement
of deep
wound over
left forelimb
elbow..
1. 1. "Septic Shock." Merriam-Webster.com. Merriam-Webster, n.d. Web. 3 Sept.
2013. <http://www.merriam-webster.com/dictionary/septic shock>.
2. 2. Anas, A. A., W. J. Wiersinga, A. F. De Vos, and T. Van Der Poll. "Recent
Insights Into the Pathogenesis of Bacterial Sepsis." The Netherlands Journal of
Medicine 68.4 (2010): 147-52. Print.
3. 3. Sharp, Claire R. "SIRS, Sepsis, MODS, MOF and More." ISBN: 978-162276-153-1 American College of Veterinary Internal Medicine (ACVIM) Forum
2012. New York: Curran Associates, 2012. 483-86. Print. New Orleans,
Louisiana, USA, 30 May - 2 June 2012.
4. 4. Oliveira RP, Velasco I, Soriano FG, Friedman G. Clinical review: Hypertonic
saline resuscitation in sepsis. Crit Care. 2002 Oct;6(5):418-23. Epub 2002 Aug
6. Review. PubMed PMID: 12398781; PubMed Central PMCID: PMC137320.
© 2013 Global Education International. All rights reserved.