Chapter 7
advertisement

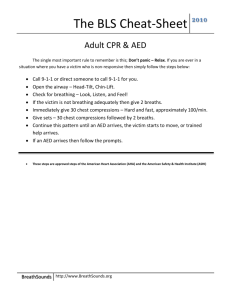
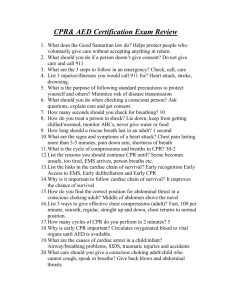
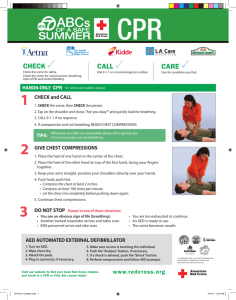
Chapter 6 Cardiac Emergencies Cardiovascular Disease Abnormal conditions that affect the heart and blood vessels Leading cause of death in US (male/female) 61 million suffer; 950,000 die each year (2005) Principle components: Coronary heart disease: arteries that carry oxygenrich blood to heart harden or narrow from build up of fatty deposits Stroke: disruption of blood flow to part of brain which causes permanent damage to brain tissue (cerebrovascular accident or CVA) Cardiovascular Emergencies 2 common emergencies: A) heart attack- (myocardial infarction) blood flow to some part of heart muscle is comprised and heart begins to die; if enough of heart dies, heart cannot circulate blood effectively -B) cardiac arrest – heart stops beating Cardiovascular Emergencies Clinically dead = no signs of life (no pulse or breathing) Cells of brain and other vital organs continue to live until oxygen is depleted CPR: cardiopulmonary resuscitation is needed; combination of chest compressions and rescue breathing Together take over functions of heart/lungs until advanced medical care given Only generates 1/3 of normal blood flow to brain Cardiovascular Emergencies Cardiac Chain of Survival: give victim of cardiac arrest the best chance of survival 1. Early recognition and early access: sooner 9-1-1 called; sooner early advanced medical care arrives 2. Early CPR: helps circulate oxygen-rich blood to vital organs until AED is ready to be used or advanced medical help arrives Cardiovascular Emergencies 3. Early Defibrillation: electric shock called defibrillation that can restore an effective heart rhythm to cardiac arrest victim; each minute delayed reduces chance of survival by 10% 4. Early Advanced Medical Care: given by trained medical personnel, who provide further care and transport to hospital Signals of Heart Attack Chest pain spreading shoulders/neck/jaw/arms Nausea or vomiting Dizziness, light headed or fainting * shortness of breath * sweating * denial *pale, ashen (gray) or bluish skin Additional Signs felt by Women Shortness of breath Nausea or vomiting Back or jaw pain Nearly ½ of all deaths from heart attacks are Women Heart Attack Most important first aid measure is to be able to recognize signals of heart attack and take action. Most victim’s will deny the seriousness of the signals he/she is experiencing. Many delay seeking care – usually 2 hours or more before going to hospital Some mistake signals for indigestion Care for Heart Attack Check, Call, Care Recognize signals of heart attack Call 9-1-1 Help victim rest comfortably Loosen any restrictive clothing Assist the victim w/any prescribed medication Monitor breathing and other signs of life Be prepared to perform CPR or use an AED if victim’s heart stops beating Heart Attack Angina Pectoris: chest pain or pressure that comes and goes at different times Heart needs more oxygen than it gets Lack of oxygen causes constricting chest pain that spreads to neck, jaw, and arms Seldom lasts longer than 3 to 5 minutes Nitroglycerin – medication that dilates blood vessels to make it easier for blood to reach heart; relieves pain If does not go away after 10 min; call 9-1-1 Cardiac Arrest Heart stops beating or beats to ineffectively to generate a pulse and blood is not circulated to brain and other vital organs Causes Cardiovascular disease Drowning *certain drugs Severe injuries to chest *suffocation Severe blood loss *electrocution Stroke or other brain damage Sudden Death- no warning signals at all Signals: no signs of life CPR for Adult Check the scene and victim If victim is unconscious, send someone to call 9-1-1 Check for breathing for no more than 10 seconds (Look, listen, and feel) Check for bleeding 30 chest compressions Head tilt/chin lift 2 slow breaths Repeat CPR Chest compressions- victim needs to be on a hard surface to be effective Hand position: 2 hands in center of chest kneel down beside victim Place heel of hand on the center of victim’s sternum (breastbone) Place other hand directly on top of first Use heel of hand to apply pressure Keep fingers off chest Shoulders directly over hands Arms straight and elbows locked CPR Compressions: push sternum down 2 inches Each movement should be smooth not jerky Do not pause between compressions Hands never leave chest during compressions 100 per minute (30 compressions – 18 seconds) Count: one and two and three and four and five ….. Up to 30 Push down saying #, up say “and” CPR Cycles of 30 compressions and 2 rescue breaths Use head tilt/chin lift technique to open airway after compressions Breath until see the chest rise (1 second); pinch nose during breath and release If two responders, send one to call 9-1-1 and get an AED When to stop CPR Scene becomes unsafe Victim shows signs of life An AED becomes available and is ready to use Another trained rescuer arrives and takes over You are too exhausted to continue Child and Infant CPR Children do not often initially suffer a cardiac emergency Generally, they suffer a respiratory emergency that can develop into a cardiac emergency Infant in need of CPR: no breathing and no signs of life Causes: car crashes, drowning, smoke inhalation, poisoning, choking, firearm injury, falls, and also from acute respiratory conditions such as asthma attack Child CPR Same as for the adult except for Give 2 minutes of CPR then call 9-1-1 if you are alone otherwise ask someone to call for you Use heel of only two hands for compressions Shoulders over hands Compress chest 2 inches smoothly 30 compressions in 18 seconds (100 per min) 2 slow rescue breaths (until see chest rise); pinch nose and release after breath Repeat cycle (30 compressions and 2 breaths) Infant CPR Same as for the adult except for Use only pads of 2 fingers for compressions and the other on the infant’s forehead to maintain open airway Shoulders over hands Compress chest 11/2 inches smoothly 30 compressions in 18 seconds (100 per min) 2 slow rescue breaths (until see chest rise); cover infant’s nose and mouth with your mouth Repeat cycle (30 compressions and 2 breaths) Automated External Defibrillator (AED) Abnormal rhythms of the heart Ventricular Fibrillation (V-fib): totally disorganized electrical activity in the heart Results in fibrillation or quivering of the ventricles Heart cannot pump blood and no signs of life (including no pulse) Ventricular Tachycardia (V-tach): very rapid contraction of ventricles Regular rhythm, rate is so fast heart unable to pump blood properly No signs of life including no pulse Fibrillation can be corrected by early defibrillation (85% of people) If not corrected, all electrical activity will cease – asystole (flatline)… cannot be corrected or reversed AED Precautions Do not touch victim while AED is analyzing (disrupts analysis) Do not touch victim during defibrillation (you could be injured) Do not use alcohol to wipe victim’s chest (flammable) Do not use AED in a moving vehicle Do not use AED on victim in contact with water Use proper pads for adults and children (under 8 yrs and less than 55 lbs) Do not use AED on victim with a nitroglycerin patch Do not use cell phones or radio transmissions w/in 6 ft of AED- interrupts analysis AED How to use an AED: As soon as it is available and safe to do so, CPR is stopped Turn on AED Open victim’s shirt and wipe chest dry Attach AED pads (upper right chest, lower left side) Plug in connector to AED AED analyze heart rhythm Say: “everyone stand clear” (do not touch victim) Deliver shock by pushing button when told to do so Say: “everyone stand clear, shocking” AED analyze again Recheck for pulse, provide additional shock if advised to do so No shock advised, continue CPR, leave AED attached