Employers* Role in Healthcare and the Impact of Health Reform
advertisement

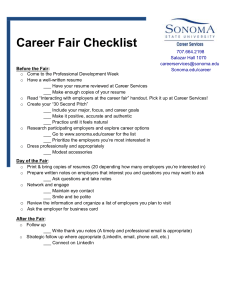
Employers, Coalitions and Health System Transformation Presentation to Florida Commission on Healthcare and Hospital Funding Laurel Pickering, MPH President & CEO Northeast Business Group on Health August 31, 2015 Agenda • • • • • Why Employers Matter in Transformation Coalitions and NEBGH New York’s Health System Transformation Commission Topics of Interest Leapfrog: Transparency of hospital quality and safety Transforming Healthcare Why Employers Matter • Employers pay for healthcare • Employers can improve access to high-value care solutions • Employers can implement health and wellness initiatives • Employers can use benefit design • Employers can engage employees and create a “culture of health” • Employers hire numerous vendors to fill gaps in the system Supporting Employers as Purchasers: Regional Business Coalitions: • Groups of employers within a local or regional community collaborate to influence their healthcare delivery systems to achieve greater value • Coalitions began in the early 1980’s; Now more than 50 local and regional coalitions around the country • Vary in size, model, and member composition • Represented in Washington, D.C. by the National Business Coalition on Health (NBCH) What do coalitions do? Education Leverage Commercial Purchasers Business Community Leadership Products & Services Drive Value And Improvement in the System Community Stakeholder Convenings Delivery System Evaluation Northeast Business Group on Health • Represents 70 employers based in New York, New Jersey, Connecticut and Massachusetts – many are large national, selfinsured employers • Employer driven and multi-stakeholder: 180 members also include health plans, providers, benefit consultants, suppliers and other stakeholders • Represents about 12 million covered lives • Use employer purchasing leverage to drive value in the system • Mission: Empowering our members to drive excellence in health and achieve the highest value in healthcare delivery and the consumer experience NEBGH Employer Members 7 NEBGH Activities • Education • Vendor Management – Health plan evaluation (eValue8) – User Groups: Aetna, Anthem, United, Kaiser and PBM • Multi-Stakeholder Collaboration – – – – – Diabetes Weight Management Cancer Readmissions Integrating Behavioral Health into Primary Care • Leapfrog • HealthPass • Future: Direct Contracting “You have to have a collaborative force to push back on the status quo” Don Berwick, former Administrator of the Centers for Medicare and Medicaid Services • One of the nation’s oldest, most successful small business, multi-carrier private exchanges (est. 1999) • 2-50 employees (expanding to 100) • Public/private partnership; seed money from City of New York • Over 15 years, insured 14,000+ small businesses and 175,000+ members • Owned by NEBGH New York State: Charting a New Course The Vision • • • • Healthier New Yorkers (population health) Lower costs Engaged consumers Systems, programs, financing, policies that support and value these goals • Triple Aim State Health Innovation Plan (SHIP) Goals Identify and stimulate the spread of promising innovations in health care delivery and finance that result in optimal health outcomes for all New Yorkers. Population Health Goal of the SHIP: • Improve population health through strengthened capacity and improved screening and prevention through closer linkages between primary care, public health, and community based supports. • 2020 Goal: Achieve top quartile performance among states in prevention and public health Shift to Payment for Value Fee-for-Service Payment for Value • More services and more complex services drive higher payments • Better practice of medicine and better outcomes drive higher payments • Time spent coordinating care generally not paid for • Coordination of care paid for • No rewards for better quality and outcomes; ‘re-work’ rewarded • Focal point is the ‘whole person’ • Incorporates population health management • Focal point is the provider and the procedure 14 The Source of Funds (SHIP/DSRIP) Strong, expert, coordinated state leadership can create value over the next four years Advanced Primary Care DSRIP Capital Restructuring Common Scorecard Prevention Agenda SHIN-NY Currently funded NY SHIP value-based purchasing Planned SIM funding Multi-payer funding Rate Review SIM Testing Grant ▪ Statewide leadership ▪ Stakeholder alignment ▪ Multi-payer business design and support NY State of Health PHIPs Workforce strategy APD The Acronyms • ACA – Affordable Care Act • ACO – Accountable Care Organizations • APC – Advanced Primary Care • APD – All Payer Database • DSRIP – Delivery System Reform Incentive Payment Program (Medicaid) • PHIP – Population Health Improvement Program • SHINY-NY – Statewide Health Information Network for New York Systems • SHIP – New York State Health Innovation Plan (all payers) • SIM – State Innovation Model (all payers) Why Advanced Primary Care? Primary care is viewed as the foundation of valuebased care and the Triple Aim, focused on: • Prevention • Care coordination (particularly for chronic conditions) • Management of complex/multiple conditions 17 SIM Grant • The Affordable Care Act (ACA) created State Innovation Model (SIM) grants • To qualify, States must demonstrate commitment to multi-payer health care payment and delivery reform to: • Improve health system performance • Increase quality of care • Decrease costs 18 SIM Grants 19 New York State SIM Grant • New York received a $100 million four-year grant • Two-thirds ($67 million) of the funds will be invested in practice transformation • The New York SIM grant is focused on transforming and strengthening primary care based on the Advanced Primary Care (APC) approach • State Goal: 80% of residents with access to primary care under a value-based payment model by 2019 20 Multi-Payer Collaboration is key • • • Greater impact on health care delivery Less complexity for primary care practices – particularly smaller practices More consistency for consumers/patients “Successful multi-payer alignment can amplify the impact of payment and delivery system reforms by sending consistent incentives to health care providers and aligning performance measurement” Millbank Memorial Fund/Pacific Business Group on Health All Aboard: Engaging Self-Insured Employers in Multi-Payer Reform 21 Role of NEBGH with NYS Reform • How come about? – No long standing relationship – NEBGH had a vision and track record of working with self-insured employers and multi-payer projects • Our Role: – Engage and gather input from payers (health plans and self-insured employers) and regional collaboratives – Help move towards multi-payer approaches – Provide feedback to New York State 22 SIM Structure Integrated Care Create an advanced primary care delivery model, inclusive of behavioral and population health, and payment methodology that is reasonable, workable, and sustainable and achieves the Triple Aim to ensure access to high quality, cost effective care for all New Yorkers. Workforce HIT, Transparency and Evaluation Modernize care delivery to best maximize new technologies that enable enhanced communications between care providers and that are able to utilize data to inform care, assure quality and promote value. Health Innovation Council Support training the next generation of the healthcare workforce who will function in a system that is better integrated and includes a strong focus on behavioral and population health. Access to Care Elimination of financial, geographic, cultural and operational barriers to access appropriate care in a timely manner. 23 This initiative will create benefits across the system Consumers Employers Primary Care Providers • • • • • • • • • Improved health Better experience, more coordination More sustainable costs More sustainable costs Higher productivity Less need for vendors to fill in the gaps • More focus on the patient Better practice of medicine Resources for practice transformation and ongoing support More aligned measures and reporting Health Plans • • Greater impact from primary care initiatives • Improved health • More sustainable costs Resources for practice transformation 24 Topics of Interest to the Commission Convincing Providers to Share Data • What’s in it for them? • If data is just based on claims it will be inaccurate. • No one wants inaccurate data to be used for public reporting or payment • Better ability to manage health of the patient if data is collectively shared and used Quality Measures • How important is for payers to use consistent measures? Critical, but very difficult • Does NEBGH have an interest in quality measures in Medicaid? Up until now we really haven’t. SIM project changes a lot • Readmissions…did we agree on a methodology among payers? We focused on resources, not rates initially Challenges Measuring Quality • Hospitals easier to measure than physicians • Groups of physicians easier to measure than individual physicians • Individual physicians is what consumers care most about • If individual physician data is publicly reported, data accuracy is critical • Not many public sites report individual physician performance • Funding APCD and Public Reporting Reasons why All-Payer Databases are Critical • Benefit to State – Complete picture of what care costs, how much providers receive from payers for same and similar services, the resources used to treat patients and variations across the state and among providers in the total cost to treat an illness or medical event • Benefit to Providers – Providers get a complete picture of their population – If insurers provide their own reporting, providers may look different across insurers. Particularly problematic when tiering • Benefit to Consumers and Businesses – Performance and cost data available regardless of insurer – Can use information to make better-informed decisions about costeffective care • Benefit to Insurers – Comprehensive data to make better-informed decisions about cost – effective care Healthcare as a Business Challenge • Cadillac tax has made healthcare a major business challenge. • Employers at a crossroads: actively manage healthcare to get reductions in costs (wellness, care management, value-based benefit design, incentives, onsite clinics, work directly with providers, reference-based pricing, etc.) or go to a defined contribution approach and private exchange • Almost all employers are offering high deductible health plans • Purchaser-driven nonprofit publicly reporting on hospital quality and safety • Founded by purchasers in 2000 in response to 1999 IOM Report To Err is Human • The right care at the right price, while empowering consumer decisionmaking 31 32 The Leapfrog Hospital Survey • One-of-a-kind • A free, voluntary survey on measures of hospital performance important to purchasers • Completed annually by over 1,500 hospitals from across the country • Measures unavailable elsewhere on the national level • Gold standard in transparency • Used by plans, vendors, and purchasers 34 What’s in the Leapfrog Hospital Survey 1. How patients fare – – – 2. Survival Predictors Infection rates Maternity measures Resources used in caring for those patients – – 3. Readmission rates Length of stay Management practices that promote safety – NQF-endorsed safe practices Breakthrough Legislation in Michigan to Require Hospitals Report to Leapfrog On June 3rd , the Michigan Legislature passed a law effectively requiring hospitals to fully complete the Leapfrog Hospital Survey in order to be eligible to receive graduate medical education funding. 57 Michigan Hospitals receive this funding, and a good number of them currently decline to report. This is the first time any state has required Leapfrog. 36 Laurel Pickering President & CEO Northeast Business Group on Health laurel@nebgh.org 212-252-7440 x224