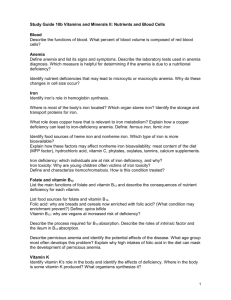
OUTLINE Definition of Terms Blood Cells Hematopoiesis
advertisement

OUTLINE I. II. III. IV. V. VI. VII. VIII. IX. X. HEMATOPOIESIS Definition of Terms Blood Cells Hematopoiesis Hematopoietic Growth Factors a. Erythropoietin b. G-CSF and GS-CSF Iron Cobalamin Folic Acid Anemia a. Iron-deficiency anemia b. Megaloblastic Anemia c. Anemia of Chronic Disease Hemostasis a. Vitamin K b. Fibrinolytic inhibitors c. Serine Protease Inhibitors: Aprotinin Self-test • • • production from undifferentiated stem cells of circulating erythrocytes, and platelets produces over 200 billion new blood cells/d in the normal person and more in conditions that cause loss or destruction of blood cells requires iron, folic acid, cobalamin and growth factors for proliferation and differentiation of blood cells DEFINITION OF TERMS Hematinics • agents that tend to stimulate blood cell formation or to increase the hemoglobin in the blood Hemostasis • finely regulated dynamic process of maintaining fluidity of the blood, repairing vascular injury and limiting blood loss while avoiding vessel occlusion (thrombosis) and inadequate perfusion of vital organs • dysregulated hemostasis include hereditary or acquired defects in the clotting mechanism and secondary effects of Infection or cancer Hemostatics • agents that maintain hemostasis Coagulants • exogenous substances used to promote coagulation. The exogenous blood coagulation factors are considered to be coagulants only when administered as drugs. BLOOD CELLS Blood • • blood volume: 4-4.5L in females ; 4.5-5L in males functions include: transport of various molecules (O2, CO2, nutrients, metabolites, vitamins, electrolytes, etc.), heat (regulation of body temperature) transmission of signals (hormones) buffering immune defense • • • • The young red cell is called a retlculocyte and normally takes about 4 days to mature into an erythrocyte. In health, erythropoiesis is regulated and maintained within a narrow range. <l% of the body's total red blood cells are produced/day It is stimulated by hypoxia. However, oxygen lack does not act directly on the haemopoietic tissues but instead stimulates the production of a hormone, erythropoietin and other hematopoietic factors. HEMATOPOIETIC GROWTH FACTORS • • • • • Red blood cells (RBCs) - transport O2 and pH regulation White blood cells (WBCs) - divided into neutrophilic, eosinophilic and basophilic, granulocytes, monocytes, and lymphocytes. (Neutrophils play a role in nonspecific immune defense; monocytes and lymphocytes participate in specific immune responses) Platelets (thrombocytes) - hemostasis glycoprotein hormones that regulate the proliferation and differentiation of hematopoietic progenitor cells in the bone marrow includes erythropoietin (epoetin alfa), granulocyte colonystimulating factor (G-CSF), granulocyte-macrophage colony-stimulating factor (GM-CSF), and interleukin-11 (IL11) Erythropoietin • This hormone stimulates hemopoietic tissues to produce red cells. • It is inactivated by the liver and excreted in the urine. It is now established that erythropoietin is formed within the Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 1 of 7 kidney by the action of a renal erythropoietic factor erythrogenin on plasma protein, erythropoietinogen. • • other tissues. In the absence of adequate iron, small erythrocytes with insufficient hemoglobin are formed. Absorption: 1mg/day; 2 mg in menstruation, birth and Hypoxia serves as stimulus for the increase in the production of EPO by the kidneys. EPO, in turn stimulates hematopoeitic organs to increase production of RBCs. G-CSF and GM-CSF (Myeloid Growth Factors) • produced by endothelium, macrophages, and a number of other immune cells. The natural human glycoprotein exists in two forms. • is present on precursor cells in the bone marrow, and, in response to stimulation by this factor, initiates proliferation and differentiation into mature granulocytes. • • pregnancy (3-15% in a normal person and ~25% in iron deficient states) iron needed in body: 10-20 mg /day (women>children>men) Only 3 – 15% of Fe intake is absorbed in the duodenum and proximal jejunum. Normal Fe intake for males is 5 – 10 mg/day; for females, 10 – 20 mg/day. 1 3 2 3 • • G-CSF stimulates proliferation and differentiation of progenitors already committed to the neutrophil lineage GM-CSF’s biologic actions: stimulates proliferation and differentiation of early and late granulocytic progenitor cells as well as erythroid and megakaryocyte progenitors stimulates the function of mature neutrophils together with interleukin-2 stimulates T-cell proliferation IRON € • • It forms the nucleus of the iron-porphyrin heme ring, which together with globin chains forms hemoglobin. Hemoglobin reversibly binds oxygen and provides the critical mechanism for oxygen delivery from the lungs to 4 (1) Intestinal epithelial cells actively absorb inorganic iron and heme iron. (2) Non-heme iron in foods and iron in inorganic iron salts and complexes must be reduced to ferrous iron (Fe2+) before it can be absorbed by intestinal mucosal cells. (3) Iron crosses the luminal membrane by 2 mechanisms: active transport (via DMT1) of ferrous iron and absorption of iron complexed with heme. (4) When total body iron stores are high and iron requirements by the body are low, the excess iron is diverted into ferritin in the mucosal cells. (5) When total body iron stores are low or iron requirements are high, newly absorbed iron is immediately transported by transferrin from the mucosal cells to the bone marrow to support hemoglobin production. Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 2 of 7 5 • Distribution (1) actively transported into the blood or complexed with apoferritin and stored as ferritin, (2) transported by transferrin to erythroid precursors in the bone marrow for synthesis of hemoglobin (as previously described) (3) transported to hepatocytes for storage as ferritin. NOTES: Apoferritin synthesis is regulated by the levels of free iron. When these levels are low, apoferritin synthesis is inhibited and the balance of iron binding shifts toward transferrin. When free iron levels are high, more apoferritin is produced to sequester more iron and protect organs from the toxic effects of excess free iron. Ferritin is detectable in serum. Since the ferritin present in serum is in equilibrium with storage ferritin in reticuloendothelial tissues, the serum ferritin level can be used to estimate total body iron stores. FOLIC ACID • • • • • • • • • provide precursors for the synthesis of amino acids, purines, and DNA deficiency is common and consequences include congenital malformations and vascular diseases average diet contains 500-700 µg of folates daily, 50-200 µg of which is usually absorbed in proximal jejunum (5-20 mg of folates are stored in the liver and other tissues) pregnant women may absorb as much as 300-400 µg of folic acid daily sources are yeast, liver, kidney, and green vegetables. folates are excreted in the urine and stool folic acid deficiency and megaloblastic anemia can develop within 1-6 months after the intake of folic acid stops Metabolism COBALAMIN • • • • • • • • • • • • • serves as a cofactor for several essential biochemical reactions in humans deficiency is secondary to inadequate absorption consists of a porphyrin-like ring with a central cobalt atom attached to a nucleotide deoxyadenosylcobalamin and methylcobalamin are the active forms Cyanocobalamin and hydroxocobalamin and other cobalamins found in food sources are converted to the active forms ultimate source of vitamin B12 is from microbial synthesis average diet contains 5-30 µg of vit B12 daily 1-5 µg of which is usually absorbed requires intrinsic factor; complex is absorb in the ileum average adult storage pool of 3000-5000 µg daily requirement: 2 µg (it would take about 5 years for all of the stored vitamin B12 to be exhausted and for megaloblastic anemia to develop if B12 absorption stopped) bound to a plasma glycoprotein, transcobalamin II excess vitamin B12 is transported to the liver for storage. Enzymatic reactions that use folates. (1) shows the vit B12-dependent reaction that allows most dietary folates to enter the THF cofactor pool and becomes the “folate trap” in vit B12 deficiency. (2) shows the dTMP cycle. (3) shows the pathway by which folic acid enters the THF cofactor pool. ANEMIA • • • • • • Two essential enzymatic reactions in humans that require vit B12. In (A), methylcobalamin serves as an intermediate in the transfer of a methyl group from N5-methylTHF to homocysteine, forming methionine. In (B), vit B12 is required in the isomerization of methylmalonyl-CoA to succinyl-CoA by the enzyme methylmalonyl-CoA mutase. • There is a reduction in blood hemoglobin concentration due to a decrease in the number of circulating erythrocytes and/or in the amount of hemoglobin they contain. It occurs when the erythropoietic tissues cannot supply enough normal erythrocytes to the circulation. In anemias due to abnormal red cell production, increased destruction and when demand exceeds capacity, plasma erythropoietin levels are increased. However, anemia can also be caused by defective production of erythropoietin as, for example, in renal disease. It is a deficiency in oxygen-carrying erythrocytes, is the most common and can easily be treated includes iron deficiency anemia, megaloblastic anemia, hemolytic anemia, hemoglobinopathies etc treatment: supplementation of iron, folic acid, cobalamin, growth factors and transfusion Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 3 of 7 A. Iron deficiency anemia • most common cause of chronic anemia and one of the most prevalent forms of malnutrition • Stages: negative iron balance - in which the demands for (or losses of) iron exceed the body's ability to absorb iron from the diet. This stage can result from a number of physiologic mechanisms including blood loss, pregnancy (in which the demands for red cell production by the fetus outstrip the mother's ability to provide iron), rapid growth spurts in the adolescent, or inadequate dietary iron intake iron-deficient erythropoiesis – once transferrin saturation falls to 15 – 20% and so hemoglobin synthesis becomes impaired iron-deficiency anemia – once hemoglobin and hematocrit begin to fall Clinical Manifestations: pallor, fatigue, dizziness, exertional dyspnea, other generalized sx of tissue hypoxia, tachycardia, increased cardiac output, vasodilation • Treatment: oral Fe++ salts o A/E: nausea, epigastric discomfort, abdominal cramps, constipation, diarrhea, black stools anaphylaxis and death (48-72H) Iron-sucrose complex and iron sodium gluconate complex o Less likely to cause anaphylactic reactions • Toxicity acute iron toxicity o seen in children o include necrotizing gastroenteritis, with vomiting, abdominal pain, and bloody diarrhea followed by shock, lethargy, and dyspnea; complications include severe metabolic acidosis, coma, and death o treated with Deferoxamine, a potent ironchelating compound, can be given systemically to bind iron that has already been absorbed and to promote its excretion in urine and feces chronic iron toxicity o secondary to iron overload (hemochromatosis) o results when excess iron is deposited in the heart, liver, pancreas, and other organs o leads to organ failure and death o can be treated by intermittent phlebotomy and Deferasirox by reducing liver iron concentrations B. Megaloblastic anemia • group of disorders characterized by the presence of distinctive morphologic appearances of the developing red cells in the bone marrow • cause is deficiency of either cobalamin (vitamin B12) or folate or genetic or acquired abnormalities affecting the metabolism of these vitamins or defects in DNA synthesis not related to cobalamin or folate • causes cobalamin deficiency or abnormalities of cobalamin metabolism* folate deficiency or abnormalities of folate metabolism** therapy with anti-folate drugs (e.g. Methotrexate) independent of either cobalamin or folate deficiency and refractory to cobalamin and folate therapy: o some cases of AML, myelodysplasia o therapy with drugs interfering synthesis of DNA [e.g. Cytosine arabinoside, hydroxyurea, 6mercaptopurine, azidothymidine (AZT)] o orotic aciduria (responds to uridine) o thiamine-responsive • - parenteral iron o reserved for patients with documented iron deficiency who are unable to tolerate or absorb oral iron and for patients with extensive chronic blood loss who cannot be maintained with oral iron alone Iron dextran o IV infusion or IM injection o give total dose of iron required to correct the hemoglobin deficit and provide the patient with 500 mg of iron stores; second is to give repeated small doses of parenteral iron over a protracted period o formula: kg x 2.3x 15 – hgb in g/dl + 500mg o dilute in D5 0.9 NaCl; given 60-90mins o include headache, light-headedness, fever, arthralgias, nausea and vomiting, back pain, flushing, urticaria, bronchospasm, and, rarely, *Causes of Cobalamin Deficiency Sufficiently Severe to cause Megaloblastic Anemia • nutritional (vegans) • malabsorption (pernicious anemia) • gastric causes (congenital absence of instrinsic factor or functional abnormality, total or partial gastrectomy) • intestinal causes intestinal stagnant loop syndrome: jejunal diverticulosis, ileocolic fistula, anatomic blind loop, intestinal stricture, etc ileal resection and Crohn's disease selective malabsorption with proteinuria tropical sprue transcobalamin II deficiency fish tapeworm Malabsorption of Cobalamin May Occur in the Following Conditins but is not usually sufficiently severe and prolonged to cause megaloblastic anemia • • Gastric causes simple atrophic gastritis (food cobalamin malabsorption) Zollinger-Ellison syndrome Gastric bypass surgery Use of proton pump inhibitors Intestinal causes Gluten-induced enteropathy Severe pancreatitis Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 4 of 7 HIV infection Radiotherapy GVH disease Deficiencies of cobalamin, folate, protein, ? Riboflavin, ? Nicotinic acid Therapy with colchicine, para-aminosalicylate, neomycin, slow-release Kcl, anticonvulsant drugs, metformin, phenformin, cytotoxic drugs Alcohol Treatment: 1. Erythropoietin originally purified from the urine of patients with severe anemia recombinant human erythropoietin (rHuEPO, epoetin alfa) is produced in a mammalian cell expression system CHF: usual dose is 50–150 U/kg 3x/week IV hemoglobin levels of 10–12 g/dL are usually reached within 4–6 weeks if iron levels are adequate; 90% of these patients respond 4-13H half life; Darbepoetin alfa with a longer half life • • • • Treatment: Cobalamin a) Oral preparations: 500-1000 µg b) parenteral injection is available as cyanocobalamin or hydroxocobalamin 100-1000 µg of vitamin B12 IM daily or every other day for 1-2 weeks then maintenance therapy consists of 100-1000 µg IM once a month for life Toxicity: rapid increase in hematocrit and hemoglobin and include hypertension and thrombotic complications 2. Myeloid Growth Factors originally purified from cultured human cell lines recombinant human G-CSF (rHuG-CSF; filgrastim) is produced through bacterial expression and recombinant human GM-CSF (rHuGM-CSF; sargramostim) is produced in a yeast expression serum half-lives of 2-7 hours after IV or SQ; longer for pegfilgrastim NOTE: - if neurologic abnormalities are present, maintenance should be given every 1-2 weeks for 6 months before switching to monthly injections - oral cobalamins are not used to treat Vit B12 deficiency with neurologic manifestations but can be used for pernicious anemia (500µg BID) Uses: myelosuppressive chemotherapy producing neutropenia in autologous stem cell transplantation **Folate Deficiency Causes : (please refer to Table on the last page) Treatment : Folic Acid oral preparations: - 400 µg folic acid daily for adults are satisfactory - 600 µg for pregnant women - 500 µg for nursing mothers A/E: C. Anemia of Chronic Disease • encompasses inflammation, infection, tissue injury, and conditions (such as cancer) associated with the release of proinflammatory cytokines—is one of the most common forms of anemia seen clinically and probably the most important in the differential diagnosis of iron deficiency • low serum iron, increased red cell protoporphyrin, a hypoproliferative marrow, transferrin saturation in the range of 15–20%, and a normal or increased serum ferritin • Decrease EPO response – interleukin, TNF • Hepcidin – found in liver in chronic inflammation decreases iron uptake and metabolism G-CSF causes bone pain GM-CSF can cause fever, malaise, arthralgias, myalgias, and a capillary leak syndrome characterized by peripheral edema and pleural or pericardial effusions; allergic reactions HEMOSTASIS Intrinsic and extrinsic pathways of blood coagulation. Both results to the activation of factor X. Blood coagulation. With tissue factor (TF), factor VII forms an activated complex (VIIa-TF) that catalyzes the activation of factor IX to factor IXa. The cascade proceeds as shown, resulting ultimately in the conversion of fibrinogen to fibrin. Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 5 of 7 Clotting Factors: inhibits fibrinolysis by free plasmin inhibits the plasmin-streptokinase complex in patients who have received that thrombolytic agent reduce bleeding by as much as 50% from many types of surgery increased risk of myocardial infarction, stroke, and renal damage in aprotinin-treated patients association with anaphylaxis has been reported in <0.5% of cases SELF-TEST 1. Vitamin K found primarily in leafy green vegetables dietary requirement is low, synthesized by bacteria that colonize the human intestine 2 natural forms exist: vitamins K1 and K2. Vitamin K1 (phytonadione) is found in food and Vitamin K2 (menaquinone) is found in human tissues and is synthesized by intestinal bacteria vitamins K1 and K2 require bile salts for absorption from the intestinal tract vitamin K1 is available in oral and parenteral forms effect delayed for 6 hours but the effect is complete by 24 hours when treating depression of prothrombin activity by excess warfarin or vitamin K deficiency IV administration should be slow( rapid infusion can produce dyspnea, chest and back pain, and even death.) vitamin K repletion is best achieved with intravenous or oral administration, administered to all newborns to prevent the hemorrhagic disease of vitamin K deficiency, which is especially common in premature infants. 2. Fibrinolytic Inhibitors adjunctive therapy in hemophilia therapy for bleeding from fibrinolytic therapy prophylaxis for rebleeding from intracranial aneurysms postsurgical bleeding and bladder hemorrhage secondary to radiation- and drug-induced cystitis. a) Aminocaproic acid similar to lysine; synthetic inhibitor of fibrinolysis competitively inhibits plasminogen activation rapidly absorbed orally and cleared by the kidney oral dosage is 6 g QID; IV at a 5 g loading dose should be infused over 30 minutes to avoid hypotension AE: intravascular thrombosis from inhibition of plasminogen activator, hypotension, myopathy, abdominal discomfort, diarrhea, and nasal stuffiness. CI: in patients with DIC or GU bleeding of the upper tract, eg, kidney and ureters because of the potential for excessive clotting b) Tranexamic acid analog of aminocaproic acid orally with a 15 mg/kg loading dose followed by 30 mg/kg/day QID 3. Serine Protease Inhibitor : Aprotinin Case for questions 1-4 A 23y/o pregnant woman is referred by her obstetrician for evaluation of anemia. She is in her fourth month of pregnancy and has no history of anemia; her grandfather had pernicious anemia. Her hemoglobin is 10g/dL (normal, 12-16 g/dL) 1. If this woman has macrocytic anemia, an increased serum concentration of transferring, and a normal serum concentration of vitamin B12, the mostly likely cause of her anemia is deficiency of a. Cobalamin b. Erythropoietin c. Folic acid d. Intrinsic factor e. Iron 2. If the patient had deficiency on folic acid, her infant would have a higher than normal risk of a. Cardiac abnormality b. Congenital neutropenia c. Kidney damage d. Limb deformity e. Neural tube defect 3. The laboratory data for your pregnant patient indicate that she does not have macrocytic anemia but instead has microcytic anemia. Optimal treatment of normocytic or mild microcytic anemia associated with pregnancy uses a. A high-fiber diet b. Erythropoietin injections c. Ferrous sulfate tablets d. Folic acid supplementation e. Hydroxocobalamin injections 4. If this patient has a young child at home and is taking ironcontaining prenatal supplements, she should be warned that they are a common source of accidental poisoning in young children and advised to make a special effort to keep these pills out of her child’s reach. Toxicity associated with acute iron poisoning usually includes a. Dizziness, hypertension and cerebral hemorrhage b. Hyperthermia, delirium and coma c. Hypotension, cardiac arrhythmia and seizures d. Necrotizing gastroenteritis, shock and metabolic acidosis e. Severe hepatic injury, encephalitis and coma 5. The iron stored in intestinal mucosal cells in complexed to a. Apoferritin b. Intrinsic factor c. Oprelvekin d. Transcobalamin II e. Transferrin 6. Which of the following is the MOST likely to ne requires by a 5 y/o boy with chronic renal insufficiency? a. Cyanocobalamin b. Deferoxamine c. Erythropoietin d. Filgrastim (G-CSF) e. Oprelvekin (IL-11) 7. In a patient who require filgrastim(G-CSF) after being treated with anticancer drugs, the therapeutic objective is to prevent a. Allergic reactions b. Cancer recurrence c. Excessive bleeding d. Hypoxia e. Systemic infections Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 6 of 7 8. The megaloblastic anemia that results from vitamin B12 deficiency is due to inadequate supplies of a. Cobalamin b. dTMP c. folic acid d. homocysteine e. N5-methlytetrahydrofolate Case for question 9-10 After undergoing surgery for breast cancer, a 53 y/o woman is scheduled to receive 4 cycles if cancer chemotherapy. The cycles are to be administered every 3-5 weeks. Her first cycle was complicated by severe chemotherapy-induced thrombocytopenia. 9. During the second cycle of chemotherapy, it would be appropriate to consider treating this patient with a. Darpoetin alpha b. Filgrastim c. Iron dextran d. Oprelvekin e. Vitamin B12 10. 20 months after finishing her chemotherapy, the woman had relapse of breast cancer. Te cancer was now unresponsive to standard doses of chemotherapy. The decision was made to treat the patient with higher-dose chemotherapy followed by autologous stem cell transplantation. Which of the following drugs is most likely to be used to mobilize the peripheral blood stem cells needed for the patient’s autologous stem cell transplantation? a. Erythropoietin b. Filgrastim c. Folic acid d. Intrinsic factor e. Oprelvekin Greetings! :D Merry Christmas and Happy New Year Everyone! (sabi ng friend ko, bkit dw super sikat si Everyone? At in fairness, halos lhat nga ng greetings sa fb ay naka-address kay Everyone. Hehehe) Again, congratulations to SINAG-TALA and SARANGGOLA NI BRO! At salamat sa lahat ng tumulong mula sa costumes ng chorvA (FARIE!!!, Pia, Tin, Elaine, Ethel, Cocai, Unica, Fao, Yvette, Grethel) to the stars (Gretch, Nice, Fiona, and those she asked to help :P), tansan (Go Fao, Armin—the official spray painter hehe), cd flower (Go Lexie, Nadinne), paper crane (Bau, Ria, Unica) , clouds, phoenix (Go Ivan, Kuya Manny, Pia, Joy), paper mache (Go Bjorn, Robin, Ewi, Jei, Yoj, Tin, Giselle), paper twine, hair blower (Go Cocai!), xray (Paul, Judith), drawings (Berry), frame (Go Mike and Rocky!!!), stand (Go Carlo!), etc ng lantern natin. Salamat din sa tulong at suporta ni Pau2x (perfection!), Gelo, Andrew, Chad, Jen, Anna, Lance, Madaam, Rika, Andrea, Mau, Faye (oops, may nakalimutan ba ko? Sana wala. Pero kung meron man, maraming salamat pa rin sayo. :D and of course, sa lahat ng hindi nahiya at nag-share ng kanilang KALANDIAN at KAARTEHAN para gumanda ang ating parol (Casey, Ate Rena, Vincent). GUJAB!!!! Start na naman ng ating buhay-estudyante. Wala namang nagsabing magiging madali ang lahat. Ang importante, alam natin kung sino ang ating kakapitan (think Saranggola ni Bro) :D Tandaan, anuman ang mangyari, anuman ang sabihin nila, si Bro, ndi bumitiw sa krus...kaya, KAPIT LANG. :) /dwtl-ssc 59 Lea E. Answers 1. Deficiencies of folic acid or vitamin B12 are the most common causes of megaloblastic anemia. If a patient with this type of anemia has a normal serum vitamin B12 concentration, folate deficiency is the most likely cause of the anemia. Answer is C. 2. Deficiency of folic acid during early pregnancy is associated with increased risk of a neural tube defect in the newborn. Answer is E. 3. The anemia most commonly associated with pregnancy is iron deficiency microcytic anemia. In this condition, oral iron supplementation is indicated. Answer is C. 4. Acute iron poisoning often causes severe gastrointestinal damage resulting from direct corrosive effects, shock from fluid loss in the gastrointestinal tract, and metabolic acidosis from cellular dysfunction. Answer is D. 5. The iron stored in intestinal mucosal cells, macrophages and hepatocytes is in ferritin, a complex of iron and the protein apoferritn. Answer is A. 6. The kidney produces erythropoietin; patients with chronic renal insufficiency often require exogenous erythropoietin to avoid chronic anemia. Answer is C. 7. Filgrastim stimulates the production and function of neutrophils, which are important cellular mediators of the innate immune system, the first line of defense against infections. Answer is E. 8. Deficiency of vitamin B12 leads to a deficiency in tetrahydrofolate and subsequently a deficiency of the dTMP required for DNA synthesis. Homocysteine and N5methyltetrahydrofolate accumulate. Answer is B. 9. Oprelvekin stimulates platelet production and decreases the number of platelet transfusions required by patient undergoing bone marrow suppression therapy for cancer. Answer is D. 10. The success of transplantation with peripheral blood stem cells depends on infusion of adequate numbers of hematopoietic stem cells. Administration of G-CSF to the donor (in the case of autologous transplantation, the patient who also will be the recipient of the transplantation) greatly increases the number of hematopoietic stem cells harvested from the donor’s blood. Answer is B. Faye Bautista | Ralph Bautista | Paul Bejosa | Berry Beriña | Alex Bondoc | Mafe Bonifacio | Mau Borja Jei Chan | Ivan de Guzman | Lance Domingo | Ram Enerio | Joy Esguerra | Lea Esquivel | Nice Gelvosa Page 7 of 7