Rehabilitation and Functional History
advertisement

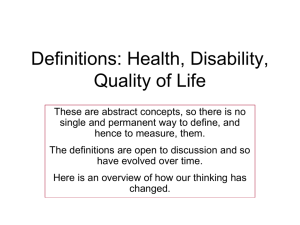
Thomas McNalley, MD Chronic Care: Introduction to Rehabilitation Medicine, Functional Assessment & Disability 2014-15 Objectives • Take a functional history • Appreciate the scope and foci of rehabilitation medicine (PM&R) • Review functional scales • Reflect on the definitions of disability and impairment, and the impact of medicalization on social roles. Function What have you done today? • Mobility • Activities of Daily Living (Basic/Instrumental) • Cognition/communication • Vocational/avocational • Transportation and community mobility Rehabilitation Physician • PM&R • physiATrist or phySIatrist? • 4 yr residency • Diagnosis and mgmt of neurologic and • • • • musculoskeletal impairment Emphasis on function and QOL Electrodiagnosis Pain mgmt – both interventional and noninterventional TEAM based intervention Inpatient Rehabilitation Team • • • • • • • Rehab Nursing Rehab psychology Social Work Nutrition Rehab/vocational counseling Education/school Therapists • Physical • Occupational • Speech pathologists • Recreation therapy Conditions we Treat • Spinal cord injury • Traumatic Brain Injury • Stroke • Multiple sclerosis • Low back pain • Neuromuscular disease including: • Muscular dystrophies • ALS • Neuropathies – hereditary and acquired • Sports Medicine • Musculoskeletal medicine Functional scales • Functional Independence Measure (“FIM”) or pediatric version – “WEE FIM”) • Karnofsky • East Coast Oncologic Group (ECOG) • Folstein Mini Mental Status • Roland-Morris Pain Scale • Pain Intensity and Interference Scale Functional Independence Measure (FIM) • • • • • Contains 18 items composed of 13 motor tasks and 5 cognitive tasks (BADLS) 7 point ordinal scale: total assistance (or complete dependence) to complete independence Scores 18 (lowest) to 126 (highest) indicating level of function Scores are generally rated at admission and discharge Dimensions assessed include: • • • • • • • Eating Grooming Upper body dressing Lower body dressing Toileting Bladder management Bed to chair transfer Toilet transfer Locomotion (ambulatory or wheelchair level) Cognitive comprehension Expression Problem solving Memory Bathing Bowel management Shower transfer Stairs Social interaction Palliative Care: Karnofsky Performance Scale • • • • • • • • • • • * 100% - normal, no complaints, no signs of disease * 90% - capable of normal activity, few symptoms or signs of disease * 80% - normal activity with some difficulty, some symptoms or signs * 70% - caring for self, not capable of normal activity or work * 60% - requiring some help, can take care of most personal requirements * 50% - requires help often, requires frequent medical care * 40% - disabled, requires special care and help * 30% - severely disabled, hospital admission indicated but no risk of death * 20% - very ill, urgently requiring admission, requires supportive measures or treatment * 10% - moribund, rapidly progressive fatal disease processes * 0% - death. Palliative care: ECOG/WHO/Zubrod Scale • • • 0 - Asymptomatic 1 - Symptomatic but completely ambulant 2 - Symptomatic, <50% in bed during the day • 3 - Symptomatic, >50% in bed, but not bedbound • 4 - Bedbound • 5 - Death Geriatrics: Katz Independence Measure (ADLS) ACTIVITIES Points (1 or 0) DEPENDENCE: (1 POINT) (0 POINTS) NO supervision, direction or personal WITH supervision, direction, personal assistance assistance or total care Points: ________ (1 POINT) Bathes self completely or needs help in bathing only a single part of the body such as the back, genital area or disabled extremity. (0 POINTS) Needs help with bathing more than one part of the body, getting in or out of the tub or shower. Requires total bathing. Points: ________ (1 POINT) Gets clothes from closets and drawers and puts on clothes and outer garments complete with fasteners. May have help tying shoes. (0 POINTS) Needs help with dressing self or needs to be completely dressed. Points: ________ (1 POINT) Goes to toilet, gets on and off, arranges clothes, cleans genital area without help. (0 POINTS) Needs help transferring to the toilet, cleaning self or uses bedpan or commode. Points: ________ (1 POINT) Moves in and out of bed or chair unassisted. Mechanical transferring aides are acceptable. (0 POINTS) Needs help in moving from bed to chair or requires a complete transfer. (1 POINT) Exercises complete self control over urination and defecation. 0 POINTS) Is partially or totally incontinent of bowel or bladder. (1 POINT) Gets food from plate into mouth without help. Preparation of food may be done by another person. (0 POINTS) Needs partial or total help with feeding or requires parenteral feeding. BATHING DRESSING TOILETING TRANSFERRING CONTINENCE Points: ________ FEEDING Points: ________ TOTAL POINTS = ______ 6 = High (patient independent) dependent) INDEPENDENCE: 0 = Low (patient very Pain: The Roland-Morris Low Back Pain and Disability Questionnaire Please read instructions: When your back hurts, you may find it difficult to do some of the things you normally do. Mark only the sentences that describe you today. I stay at home most of the time because of my back. I change position frequently to try to get my back comfortable. I walk more slowly than usual because of my back. Because of my back, I am not doing any jobs that I usually do around the house. Because of my back, I use a handrail to get upstairs. Because of my back, I lie down to rest more often. Because of my back, I have to hold on to something to get out of an easy chair. Because of my back, I try to get other people to do things for me. I get dressed more slowly than usual because of my back. I only stand up for short periods of time because of my back. Because of my back, I try not to bend or kneel down. I find it difficult to get out of a chair because of my back. My back is painful almost all of the time. I find it difficult to turn over in bed because of my back. My appetite is not very good because of my back. I have trouble putting on my sock (or stockings) because of the pain in my back. I can only walk short distances because of my back pain. I sleep less well because of my back. Because of my back pain, I get dressed with the help of someone else. I sit down for most of the day because of my back. I avoid heavy jobs around the house because of my back. Because of back pain, I am more irritable and bad tempered with people than usual. Because of my back, I go upstairs more slowly than usual. I stay in bed most of the time because of my back. Pain intensity and interference: 2-item scale • “Over the last month, on average, how would you rate your pain?” 1-10 scale • “Over the last month, on average, how much has pain interfered with your daily activities?” 1-10 scale, with 1 “no interference,” and 10 “unable to carry on daily activities.” Impairment, disability and society: International Classification of Function (ICF) ICF: Back pain as example Impairment and disability • Impairment: an injury, illness, or congenital condition that causes or is likely to cause a loss or difference of physiological or psychological function. • Disability: a social construct -- the loss or limitation of opportunities to take part in society on an equal level with others due to social and environmental barriers. Examples of impairment and disability Impairment (cause) • Abnormal gait (spastic diplegia) • Executive dysfunction (TBI) • Fecal incontinence (neurogenic bowel) • Wheelchair use (paraplegia) Disability • Can’t join soccer team • Reduced educational performance • Limited social interaction • Reduced access to buildings fewer employment opportunities Models of disability • Medical • Identify impairments and classify them • Reductionist? • Brings resources to bear • “problem to be fixed” Models of disability (cont) • Moral/Charity model • Punishment/God’s will • Inspiration porn • Social Model • Cultural construction of disability • Social change can mitigate (eliminate?) disability • Bio-psycho-social model • See ICF Implications of disability for healthcare • 28% of insured persons with disabilities report not getting needed tx, equipment, medications (vs. 7% of non-disabled) • 19% of those with disabilities did not get medical care when they needed it (vs. 6% of nondisabled) • Why? • Lack of insurance coverage • High costs • Difficulties/disagreements w/ doctors • Access to clinics • Communication disorders Resources • UW Disability Studies (Upper campus) • Disability Non-clinical selective • Implicit Associations Test https://implicit.harvard.edu/implicit/ • Dept of Rehabilitation Medicine • Center for Human Development and Disability 6 Whispers of the (palliative) care team • • • • • • Be a healing presence Be a humble servant Trust your team Words are important; silence is profound. Do your dance and retreat in peace. Don’t be afraid to reach out and ask for help. Thanks!