Lab lecture 2 – prescription writing
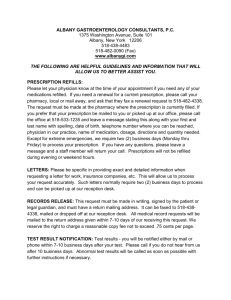
advertisement

Prescription Writing Lab Lecture Prescription • The prescriber’s written order to prepare or dispense a specific treatment (usually a medication) for a specific patient • Who can write a prescription? • Physician • Dentist • Veterinarian • Nurses are authorized to administer medications • Pharmacists are authorized to prepare and dispense drugs Definition of terms • Generic name or International Non-proprietory Name (INN) – the scientifically and internationally recognized name for their active ingredient/s • Drug product – finished product containing the active ingredient, may also contain inactive ingredients • Fixed Dose Combination (FDC) – containing 2 or more active ingredients Rational Prescription Writing 1. Make a specific diagnosis 2. Consider the pathophysiologic implications of the diagnosis 3. Select a specific therapeutic objective or goal. 4. Select a drug of choice 5. Determine the appropriate dosing regimen 6. Devise a plan for monitoring the drug’s action and side efects and determine end point for therapy 7. Plan a program of patient education. Rational Prescription Writing • Rule of Right • Right drug, for the right patient, with the right diagnosis, at the right dose, right route, right intervals, right duration of therapy under prevailing constraints • SANE Criteria: • • • • Safety Affordability Need Efficacy • Choose drugs that are clearly needed and scientifically proven to be effective • Do not be influenced by patient pressure or med rep pressure Elements of a prescription 1. Identity of the prescriber a. b. c. Full name, address and contact number on top License number, PTR, S2 number Signature 2. Identity of the patient a. b. Full name, age, address, sex (weight – optional) Date 3. Body of the prescription a. b. c. d. Superscription Inscription Subscription and Refill information Transcription Elements of a prescription 3. Body of the prescription a. Superscription = Rx = “take thou” b. Inscription • • Name of medication (generic and brand) Strength and and dosage to be dispensed c. Subscription and refill information • • Instruction to pharmacist for quantity of medication Refill or not d. Transcription = sig. = “label” • • Directions for use: route, interval, duration, purpose Other instructions Why Generic? • Every generic drug product should be as satisfactory as the trade-named product • Generic drugs have the same bioavailability • Bioequivalent to a reference standard formulation • These drugs must have the same rate and extent of absorption • Should not differ between manufacturers • Generic names allow substitution of medicines by the pharmacist • Due to unavailability, cost, etc. Why Generic? • Generic names • Of distinct sound and spelling • Grouped or related drugs may have similar prefixes of suffixes to easily identify their class • • • • • • • -ac = anti-inflammatory agents/NSAIDS Cef- = cephalosporins -cillin = penicillin group -dipine = calcium channel blockers -olol = beta blockers -tidine = H2 antagonists (antacids) -pril = ACE inhibitors Prescribing errors • Must be legible, unambiguous, dated and signed • Should contain sufficient information to permit the pharmacist or nurse to discover possible errors before the drug is dispensed or administered Prescribing errors • Omission of information • Continue pre-operative medicines • Continue eye drops • Poor prescription writing • Poor handwriting • Misplaced decimal point • Abbreviations that may be misread • Ex. 10U or 10μg may be read as 100 • Does the abbreviation OD mean once a day or right eye? Prescribing errors • Inappropriate drug prescriptions • Failure to recognize contraindications imposed by other diseases the patient may have • Failure to obtain information about other drugs the patient is taking (ex. drug-drug interactions) • Failure to recognize possible psychochemical incompatibilities between drugs (ex. disulfiram and alcohol) Compliance • The extent to which patients follow treatment instructions (adherence) • • • • Fail to buy/obtain the medication Fail to take the medication as prescribed Prematurely discontinues the medication Patient or another person takes medication inappropriately (ex. sharing of meds) Off labeled use of drugs • Not the actual intention of the drug, but may seem to be beneficial in some cases • Ex. Finasteride = initially a medicine for BPH, now a medicine for hair loss Pediatric Dosing • Suspensions or syrups or drops • Calculated based on weight • Dose recommendations based on weight • Ex. paracetamol: 10-15mg/kg/dose, given every 4 hours • Ex. amoxicillin: 30-40mg/kg/day divided into 3 doses • Dose recommendations based on age and average weight • Decongestants: phenylpropanolamine or phenylephrine • 2-6 years = 2.5mL QID • 7-12 years = 5mL QID • Cetirizne • 6months-2 years: 2.5mg/day • 2 years -5 years: 5mg/day or 2.5mg BID Case 1 • S> An 18 year old student came to the clinic due to nasal congestion, slightly productive cough x 2 days. No fever. No vomiting. No pain. Able to eat well. Slight discomfort during sleeping • O> Pertinent PE: Temp: 36.8C, not in distress. boggy turbinates, slightly hyperemic pharynx, clear breath sounds. • A> • P> Case 1 • Available drugs • • • • • • • • Decolgen Sinutab Neozep Bioflu Solmux Mucosolvan Ventolin nebulizer Benadryl expectorant Case 2 • S> 6 year old male, came to you for fever and sore throat for 3 days duration. Decreased appetite, no vomiting or diarrhea. No cough or colds. No other complaints. Mother says her son has G6PD deficiency • O> Weight = 20kg, Temp = 38.5C, not in distress. Normal nose and ears. Hyperemic tonsils with exudates. Clear breath sounds and heart sounds. • A> • P> Case 2 • Available antibiotics • • • • • Amoxicillin Co-amoxiclav Chloramphenicol Co-trimoxazole Metronidazole