GI Board review: Part I
advertisement

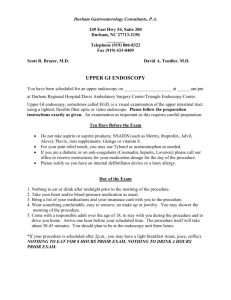
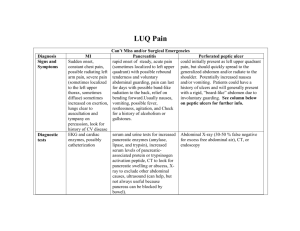
GI BOARD REVIEW: PART I By Molly McVey Esophagus • Symptoms of esophageal disorders: • Dysphagia • Oropharyngeal – diagnostic test is videofluoroscopy • Esophageal – diagnostic test is upper endoscopy • Reflux • Chest pain • Odynophagia • Globus sensation A 35-year-old man is evaluated for a 2-year history of intermittent chest pain. The pain is retrosternal, lasts for seconds to minutes, is unrelated to exertion, and does not radiate. It is occasionally associated with swallowing. He reports intermittent dysphagia to solids and liquids. He denies any reflux symptoms or weight loss. He does not have any risk factors for cardiac disease. Physical examination is unremarkable. Upper endoscopy is normal. A barium swallow is shown. Which of the following is the most likely dignosis? A. Achalasia B. Diffuse esophageal tz ki r Sc ha iti so ph ag hi li ce ge al Eo s in op 0 s sm sp a la Ac ha es op ha 0 in g 0 sia 0 Di ffu se spasm C. Eosinophilic esophagitis D. Schatzki ring Nonmalignant esophageal disorder • Hypertonic Motility Disorder • Achalasia • Failure of lower esophageal sphincter to relax • Symptoms don’t respond to empiric PPIs or H2Bs • Barium swallow: esophageal dilation with “bird’s beak” distally • Manometry: esophageal aperistalsis and incomplete relaxation of LES • Endoscopy performed to exclude mechanical obstruction • Treatment: surgical myotomy vs pneumatic balloon dilatations vs botulinum toxin injections • Pseudoachalasia • Diffuse esophageal Spasm • “corkscrew esophagus” on barium swallow • Tx: CCB • Nutcracker esophagus • distal esophageal pressures of >220mmHg during peristalsis Nonmalignant esophageal disorder • Hypotonic Motility Disorders • “Scleroderma esophagus” • Aperistalsis on manometry and hypotensive LES • Tx is acid reflux control A 25-year-old man is evaluated for a 5-year history of slowly progressive solid-food dysphagia that is accompanied by a sensation of food sticking in his lower retrosternal area. He has compensated by modifying his diet and avoiding fibrous meats. He has not lost weight, and he has not had trouble drinking liquids. He has had episodes of food impaction that he manages by inducing vomiting. He has had no difficulty initiating a swallow and has not had chest pain, odynophagia, reflux symptoms, or aspiration of food while swallowing. He has seasonal allergies that are treated with antihistamines and asthma that is treated with inhaled albuterol. Physical examination is normal. Which of the following is the most likely diagnosis? A. Achalasia B. Eosinophilic esophagitis C. Esophageal candidiasis gia ea ld lm op ha r yn g ge a 0 ys ph a an cy ign al an d id ia iti lc ge a Es op ha Es op ha 0 sis 0 s sia 0 so ph ag la ce Ac ha hi li Eo s in op E. Oropharyngeal dysphagia 0 Or D. Esophageal malignancy Nonmalignant esophageal disorder • Infectious Esophagitis: • Candida – white plaques • Tx: fluconazole • HSV – multiple superficial ulcers • Tx: acyclovir • CMV – isolated esophageal ulcers • Tx: ganciclovir • Pill-induced esophagitis • Common meds assoc: tetracycline (doxycycline), iron sulfate, bisophosphonates, potassium, NSAIDs and quinidine • Eosinophilic esophagitis • Adults, solid food dysphagia and food impaction • High prevalence of asthma and seasonal allergies • Dx by >15 eosinophils/hpf on esophageal biopsy A 50-year-old woman is evaluated for a 1-year history of recurrent left-sided chest pain. The pain is poorly localized, nonexertional, and occurs in 1-minute episodes. There is no dyspnea, nausea, or diaphoresis associated with these episodes. She has not had dysphagia, heartburn, weight change, or other gastrointestinal symptoms. She has no other medical problems and does not smoke cigarettes. Family history is noncontributory. On physical examination, vital signs are normal and BMI is 30. The patient's chest pain is not reproducible with palpation. The cardiac examination reveals normal heart sounds without murmurs or extracardiac sounds. The remainder of the physical examination is normal. A lipid panel, fasting plasma glucose test, and chest radiograph are normal. An echocardiogram shows a normal ejection fraction with no wall motion abnormalities. An exercise stress test is normal. Which of the following is the most appropriate management? A. Ambulatory pH study B. Begin an NSAID Am 0 0 Tr ial of a PP I sc op y NS A an n gi Be bu l at or yp H st ud y D. Trial of a PPI 0 ID 0 En do C. Endoscopy Nonmalignant esophageal disorder • GERD • Symptoms: heartburn and regurgitation • Dx: symptoms, endoscopy or ambulatory pH monitoring • Empiric tx first if not effective then endoscopy • Alarm symptoms (dysphagia, anemia, vomiting or weight loss) • Endoscopy is first line • Ambulatory pH monitoring: don’t respond to tx and endoscopy is unremarkable • Tx: • Lifestyle modifications • Medications: PPI superior to H2Bs • PPI may increase susceptibility to GI infections (C.diff) and pneumonia • Unclear data on increase risk of hip fracture • Fundoplication A 55-year-old man is evaluated for a 6-year history of typical gastroesophageal reflux symptoms treated on an as-needed basis with a proton pump inhibitor. However, the frequency of his reflux symptoms has recently increased and his episodes do not respond to treatment as completely as in the past. An upper endoscopy is scheduled to evaluate the cause of this change in his symptoms. Endoscopy reveals a 4-cm segment of salmon-colored mucosa in the distal esophagus. Biopsy from the salmon-colored segment reveals intestinal metaplasia and goblet cells with no dysplasia. In addition to starting a daily PPI, which of the following is the most appropriate management? A. Daily COX-2 inhibitor therapy B. Endoscopic ablation C. Fundoplication ye ar in sc op y en do at pe 1 at io pl ic Fu nd o bl at ca En do sc op i 0 n 0 Re Da i ly CO X -2 in hi bi to rt h. .. D. Repeat endoscopy in 1 year 0 io n 0 A 75-year-old man is evaluated for a 2-month history of progressive solid-food dysphagia. He has transitioned from solid to puréed foods and has been able to maintain his weight. He has a 40-pack-year history of cigarette smoking and a history of alcohol abuse. On physical examination, vital signs are normal. BMI is 35. There is no evidence of supraclavicular lymphadenopathy. Cardiopulmonary examination is normal. On abdominal examination, there is no evidence of mass, tenderness, or hepatomegaly. A complete blood count reveals a hemoglobin level of 10.9 g/dL (109 g/L). Endoscopy reveals an obstructive mass in the distal esophagus, and biopsies show invasive adenocarcinoma. Which of the following is the most appropriate management? 14 A. CT/PET and endoscopic US B. Esophagectomy C. Feeding tube placement D. Radiation therapy 2 y th e t io n Ra di a pl tu be ng Fe ed i ra p en t ac e ge c m to m S cU Es op ha sc op i en do nd Ta PE CT / 0 y 0 Malignant Disorders of the Esophagus • Barrett Esophagus • Complication of GERD • 30-50 fold increased risk of esophageal adenocarcinoma • Screening is not recommended • Dx: biopsy • Tx: • PPI ? Lower risk of developing high grade dysplasia • Ablative therapies for high grade dysplasia • Surveillance: • No dysplasia: repeat endoscopy in 1 year • Low grade: repeat endoscopy in 6 months • High grade: removal of focal lesions Malignant Disorders of the Esophagus • Esophageal Carcinoma • Risk factors for SCC: long term exposure to alcohol and tobacco; nitrosamine; corrosive injury to the esophagus; dietary deficiencies; achalasia; tylosis; HPV • Risk factors for adeno: tobacco, obesity, symptomatic GERD and BE • Dx: endoscopy • Staging: CT, endoscopic US (locoregional staging) and PET A 44-year-old woman is evaluated for a 1-year history of vague upper abdominal discomfort that occurs after eating. She is from a rural area in a developing country. She has not had nausea, vomiting, dysphagia, odynophagia, weight loss, or black or bloody stools. She is otherwise healthy. She has no personal history of peptic ulcer disease and no family history of gastrointestinal malignancy. Her only medication is a multivitamin. On physical examination, temperature is 36.8 °C (98.2 °F), blood pressure is 127/82 mm Hg, pulse rate is 72/min, and respiration rate is 16/min. BMI is 27. There is epigastric tenderness with moderate palpation but no masses or lymphadenopathy. Complete blood count is normal. Which of the following is the most appropriate management? 9 A. H.pylori stool antigen testing B. Initiate an H2 blocker 3 2 C. Initiate empiric treatment for In i tia te py do sc o en m rfo r Pe em tia pi te r ic an tre H2 at bl m oc k en . .. er .. te . en nt ig In i st oo la ri H. py lo H.pylori infection D. Perform endoscopy 0 Dyspepsia • PUD and h.pylori • Alarming symptoms: >50 yo, anemia, dysphagia, odynophagia, vomiting, weight loss, family history of GI malignancy, person history of PUD, gastric surgery or GI malignancy or abdominal mass or LAD on exam • < 50yo and no alarming symptoms: • Test and treat for h.pylori if coming from area with high rates of h.pylori • Empiric PPI in areas where h.pylori rates are low • Alarm symptoms then straight to endoscopy Peptic Ulcer Disease • Gastric or duodenal mucosal break >5mm • >90% caused by NSAIDs and H.pylori • Other causes: gastrinoma (ZE) – multiple ulcers beyond • • • • duodenal bulb associated with esophagitis and diarrhea, Crohn disease, mastocytosis, G-cell hyperplasia, viral infection, infiltrative disease and radiation Gastric: pain shortly after meals, not relieved as much with antacids Duodenal: pain 2-5 hrs after meals and relieved by food or antacids Dx: upper endoscopy with biopsy Complications: bleeding, penetration, perforation and obstruction H. pylori • Infection causes gastritis, PUD, gastric cancer and MALT • Testing: • Serology: suboptimal • Positive IgG shows exposure but not previously treated or eradicated • Urea breath test: good but more costly • Fecal antigen: test of choice for initial dx and eradication proof • >90% sensitivity, specificity and predictive value before and after treatment ***PPIs, H2Bs, antibiotics and bismuth decrease the sensitivity of all H. pylori test except serology**** • Stop PPIs 2 weeks prior to nonserologic testing • Stop antibiotics and bismuth 4 weeks before testing • Stop H2Bs 23-48hr before testing • Endoscopy: histology, rapid urease test and culture • Most cost-effective is gastric biopsies with rapid urease testing • If high suspension and histology negative then send serology test H. pylori • Treatment: • First line: • clarithromycin, amoxicillin and BID PPI x 10-14 days • Tetracycline, metronidazole, bismuth and BID PPI x 10-14 days • Amoxicillin (days 1-5) then clarithromycin and metronidazole or tinidazole (days 6-10) all along with BID PPI • Eradication: • Urea breath test or fecal antigen test 4-6 weeks after treatment A 26-year-old man is evaluated for a 16-month history of intermittent episodes of abdominal discomfort, nausea, and vomiting. He is relatively asymptomatic between episodes, which occur every 4 to 6 weeks. Episodes consist of vomiting once every 2 to 4 hours for about 48 hours. The only relieving factor is hot baths. He currently feels well, but it has been 5 weeks since his last episode. His medical history is notable for daily marijuana use for the past 2 years. On physical examination, vital signs are normal. BMI is 25. Abdominal examination is normal. Laboratory studies reveal a normal complete blood count and normal plasma glucose and thyroidstimulating hormone levels. An abdominal radiograph is normal. Which of the following is the most likely diagnosis? 10 A. Cannabinoid hyperemesis 2 0 e lic Cy c op a Ga st r yn dr o d. .. vo m it i ng s ps eu al tin nt es ci on i Ch r m . es i.. m re hy pe d in oi na b re sis 0 Ca n syndrome B. Chronic intestinal pseudoobstruction C. Cyclic vomiting syndrome D. Gastroparesis Stomach potpourri • Cannabinoid hyperemesis syndrome: abdominal pain, nausea and vomiting in patient using marijuana; associated with compulsive washing • Gastroparesis: nausea/vomiting/early satiety; dx with gastric emptying study; tx dietary adjustment and prokinetic medications • Gastric polyps: if <40 with numerous gastric fundic polyps refer for colorectal evaluation for workup of familial adenomatous polyposis syndrome • Gastric carcinoid tumor: <2cm then survey every 6-12 months x 3 years A 34-year-old man is evaluated in the emergency department for confusion. Three weeks ago he underwent a Roux-en-Y gastric bypass for morbid obesity. He has had poor oral intake since the surgery because of nausea. Vitamin B12 injections were prescribed, but he has not started them yet. He recently took hydrocodone for pain, but he has not needed it for several days. His only current medication is a multivitamin with iron. On physical examination, he is afebrile. Blood pressure is 115/80 mm Hg (no orthostatic changes), and pulse rate is 85/min. The mucous membranes are moist, and there is no skin tenting. He has an ataxic gait, nystagmus, and a disconjugate gaze. The remainder of the neurologic examination is normal. Laboratory studies, including a complete blood count, glucose, and electrolytes, are normal. Which of the following is the most appropriate next step in management? 9 A. CT of the head B. Glucose infusion C. IV naloxone 2 1 B1 2 e in it m ou sV th ia an e IV Su bc ut IV in na fu s io n ad he co se Gl u th e of CT E. Subcutaneous Vit B12 0 lo xo ne 0 D. IV thiamine Bariatric Surgery Complications • Postoperative mortality caused by VTE, anastomotic leak and exacerbation of preexisting comorbidities • Nutritional deficiencies: • Iron - anemia • Vitamin B12 - anemia • Folic acid - anemia • Calcium • Vitamin D • Thiamine – Wernicke-Korsakoff syndrome • Vitamin A • Vitamin E A 42-year-old woman is evaluated following hospitalization for acute pancreatitis due to gallstone disease that occurred 8 weeks ago. An admission CT scan demonstrated no evidence of fluid collection or necrosis, and she had an uncomplicated cholecystectomy prior to discharge. She has no pain, nausea, or anorexia. However, 2 weeks ago she was evaluated for nephrolithiasis following an episode of renal colic and underwent a CT scan. The CT scan demonstrated a 4-mm stone in the right ureter and a 6-cm fluid collection adjacent to the pancreatic tail. There was no evidence of solid debris, and it did not communicate with the main pancreatic duct. There were no mass lesions in the liver and no pancreatic necrosis. She has since passed the kidney stone and is asymptomatic. On physical examination, temperature is 37.2 °C (99.0 °F), blood pressure is 112/72 mm Hg, pulse rate is 66/min, and respiration rate is 18/min. BMI is 25. Abdominal examination discloses a nondistended abdomen and active bowel sounds. There is no tenderness to palpation, hepatosplenomegaly, or masses. Laboratory studies, including complete blood count, liver chemistry tests, CA 19-9, and alkaline phosphatase, are normal. Which of the following is the most appropriate next step in management? 11 A. Endoscopic US B. MRCP te ... e in ag ra di a ld fu rt Su rg ic a dr a eo us ta n rc u 0 e in ag M sc op i Pe testing or therapy En do E. No further diagnostic cU S RC P D. Surgical drainage 0 gn os t ic 0 he r 1 No C. Percutaneous drainage Acute Pancreatitis • Classified as mild (interstitial) or severe (organ failure or necrosis/fluid collections) • Dx: symptoms, elevated amylase and/or lipase and CT • Prognostic criteria: BUN most accurate predictor of severity • Management: IVFs, pain control, bowel rest • NG not needed unless ileus or bowel obstruction 2/2 pancreatitis • Antibiotics NOT indicated unless necrosis seen on CT • ERCP only indicated if cholangitis present or worsening clinical symptoms with rising liver enzymes • Complications: • Fluid collections, pseudocysts, pancreatic duct leak, splenic vein thrombosis Chronic Pancreatitis • Symptoms: abdominal pain, weight loss, diarrhea • Signs: exocrine and endocrine insufficiencies – fat-soluble vitamin deficiency, insulin dependence • Dx: no gold standard; clinical symptoms and imaging demonstrating pancreatic calcifications, ductal dilatation, parenchymal atrophy and/or focal inflammatory masses • Tx: pancreatic enzymes, fat-soluble vitamin replacement and pain control….surgical therapies saved for failure of medical management A 72-year-old man is evaluated for a 2-week history of painless jaundice. He also has pruritus, anorexia, and weight loss of 4.5 kg (10.0 lb) during the same time period. He takes no medications. On physical examination, vital signs are normal. BMI is 22, and he appears thin. Scleral icterus and jaundice are present. There is no hepatosplenomegaly and no cutaneous signs of cirrhosis. The gallbladder is palpable. Laboratory studies: Complete blood count Normal Alkaline phosphatase 522 units/L Alanine aminotransferase 354 units/L Aspartate aminotransferase 215 units/L Total bilirubin 12.1 mg/dL (206.9 µmol/L) Direct bilirubin 10.7 mg/dL (183.0 µmol/L) Contrast-enhanced CT scan demonstrates a dilated common bile duct with focal cutoff in the pancreas head. No focal mass is noted in the head. The pancreas duct 9 is dilated. There is no evidence of mass lesions in the liver. Which of the following is the most appropriate initial management? m d. .. cr e fo rp an Re fe r en do sc o pi c at ic o M do m in al rfo r Pe rfo r m in US .. RI 0 ab se r um CA 19 -9 0 Pe Obtain serum CA19-9 Perform abdominal MRI Perform endoscopic US of pancreas Refer for pancreaticoduodenectomy Ob ta A. B. C. D. 3 Pancreatic Adenocarcinoma • 5 year survival rate of 5% • Presentation: painless jaundice, anorexia, weight loss • >50yo presenting with acute pancreatitis – scan • Dx/staging: CT, EUS, biopsy Autoimmune Pancreatitis • Lymphoplasmacytic infiltrate of IgG4 • Affects the pancreas, biliary tree, salivary glands, retroperitoneum and lymph nodes • Present with painless obstructive jaundice • Imaging: CT shows “sausage-shaped” gland • Dx: biopsy showing >10 IgG4 positive cells/hpf • If mass present, want to exclude malignancy • Tx: steroids 23-year-old woman is evaluated in the hospital for recurrent episodes of hypoglycemia. During hospitalization, she developed neuroglycopenic symptoms after 8 hours of fasting associated with a plasma glucose level of 30 mg/dL (1.7 mmol/L) and a corresponding insulin level of 8 µU/mL (58 pmol/L). She does not have diabetes mellitus and does not take oral hypoglycemic agents or insulin. On physical examination, temperature is 37.0 °C (98.6 °F), blood pressure is 90/56 mm Hg, pulse rate is 110/min, and respiration rate is 22/min. BMI is 22. No tenderness, masses, or hepatosplenomegaly is found on abdominal examination. A contrast-enhanced CT scan demonstrates no evidence of a pancreatic mass. Which of the following is the most appropriate diagnostic test to perform next? A. Endoscopic US B. MRI C. Operative pancreatic 10 M ex p. .. S cU tre nt e Op er at ive ot id pa n es cr e En do at cin ic sc op i ph y 0 RI 0 t ig ra 1 Pe exploration D. Pentetreotide scintigraphy Pancreatic Neuroendocrine Tumors Tumor Type Gastrinoma Insulinoma VIPoma Glucagonoma Hormone Symptoms Criteria for Diagnosis Gastrin Peptic ulcers, diarrhea, esophagitis (ZollingerEllison syndrome) Elevated serum gastrin >1000 pg/mL (1000 ng/L), secretin stimulation test Insulin Hypoglycemia; associated with MEN-1 Inappropriately high insulin level during hypoglycemia Vasoactive intestinal peptide Watery diarrhea, hypokalemia, hypochlorhydria (VernerMorrison syndrome) Elevated serum VIP level >75 pg/mL (75 ng/L) Glucagon Dermatitis (necrolytic migratory erythema), diabetes mellitus Elevated serum glucagon >1000 pg/mL (1000 ng/L) MEN-1 = multiple endocrine neoplasia type 1; VIP = vasoactive intestinal peptide. A 34-year-old woman is evaluated in an urgent care clinic for a 1-day history of watery diarrhea and mild abdominal cramps. She is having four watery stools per day. She has not had fever or blood in her stool. Although she has felt mildly nauseated, she has been able to stay hydrated with oral intake. She works as a banker, and colleagues at work have had similar gastrointestinal symptoms over recent weeks. She has no history of recent hospitalization, antibiotic use, or medication changes. She has no risk factors for HIV infection. On physical examination, temperature is 36.1 °C (97.0 °F), blood pressure is 110/75 mm Hg, pulse rate is 86/min, and respiration rate is normal. BMI is 24. The mucous membranes are moist, and there is no skin tenting. Abdominal examination reveals mild abdominal tenderness but normal bowel sounds. There is no guarding or rebound. A urine pregnancy test is negative. Which of the following is the most appropriate diagnostic test? 9 A. C.diff PCR B. Fecal leukocyte testing er na l st ud i lc u. .. i.. ad di No al st o ol ba c os c op y w te sti n te oi d m sig Ge n bl e xi 0 es 0 tio 0 g PC R C. di ff le uk oc y Fe c al Fle biopsies D. General stool bacterial cultures E. No additional studies 0 te ria C. Flexible sigmoidoscopy with Diarrhea • Definition: Increased frequency or liquidity of stool or stool weight >200g/d • Classifications: • Duration: • Acute <14 days (think infectious) • Subacute 14 days-4 weeks • Chronic >4 weeks (good history, stool studies, endoscopic eval, imaging • Feature: • Osmotic: volume <1L/d, stool improves when fasting; stool osmotic gap <50mOsm/kg • Secretory: large volume, electrolyte disturbances, no improvement with fasting; stool osmotic gap >100mOsm/kg • Inflammatory: blood or mucus in stool • Malabsorptive: loss of nutrients, fat, carbohydrate or protein A 26-year-old man is evaluated for fatigue and has been newly diagnosed with iron-deficiency anemia. The patient has Down syndrome, and details of his clinical history are provided by his mother. There is no history of melena, hematochezia, or hematuria. His hemoglobin level was checked 2 years ago and was normal. His bowel movements are regular, and his weight is unchanged. He has no abdominal problems. On physical examination, temperature is 36.3 °C (97.3 °F) and pulse rate is 88/min. Other vital signs are normal. BMI is 29. Mild skin pallor is noted. Abdominal and rectal examinations are normal. Serum tissue transglutaminase IgA antibody testing is negative. Colonoscopy and upper endoscopy are unremarkable. Which of the following is the most appropriate diagnostic test to perform next? A. Meckel scan B. Push enteroscopy C. Repeat upper endoscopy with am in at io en d. .. e ex ac ua i St oo lg el c en do 0 n 0 ap su l sc op y. .. 0 bo w all - tu pp er Sm n sc a en te ea Re p ec ke l Pu sh 0 ro sc op y 0 M small-bowel biopsies D. Small-bowel capsule endoscopy E. Stool guaiac examination Malabsorption • Fat malabsorption: diarrhea and weight loss • Fecal fat collection for 48-72 hours • Pancreatic insufficiency • Celiac disease • Autoimmune enteropathy • Small intestinal bacterial overgrowth • Carbohydrate malabsorption: diarrhea, bloating, excess flatus but NO weight loss • Lactose • Protein malabsorption: diarrhea, edema, ascites, anasarca • Stool alpha 1 antitrypsin clearance test • Ex: C.diff infection, IBD, celiac dz, Whipple dz, constrictive pericarditis, lymphangiectasia and lymphatic obstruction Celiac disease • Symptoms: diarrhea, bloating and weight loss • Extraintestinal: anemia, osteopenia/porosis, dematitis herpetiformis… • Associated with Down syndrome, type 1 DM, juvenile RA, thyroid dz and AI liver conditions • Dx: tTG IgA antibody (false negative in IgA deficiency) • Tx: gluten-free diet A 51-year-old woman is evaluated for a 6-month history of diarrhea and bloating. She reports four to six loose stools per day, with occasional nocturnal stools. She has had a few episodes of incontinence secondary to urgency. She has not had melena or hematocheziabut notes an occasional oily appearance to the stool. She has lost 6.8 kg (15.0 lb) during this time period. Results of a colonoscopy 1 year ago were normal. She has not had recent travel, antibiotic use, or medication changes. She does not think consumption of dairy products alters hersymptoms. She has a history of systemic sclerosis for which she takes omeprazole for symptoms of gastroesophagealreflux disease. On physical examination, vital signs are normal. BMI is 22. Facial telangiectasiasare present, and there is bilateral skin thickening of the hands. The abdomen is mildly distended, and bowel sounds are normal. Rectal examination is normal, with normal resting and squeeze tone.There are no palpable mass lesions. Laboratory studies: Hemoglobin 10.8 g/dL (108 g/L) Mean corpuscular volume 104 fL Serum electrolytes Normal Folate 63 ng/mL (143 nmol/L) Glucose Normal Thyroid-stimulating hormone Normal Vitamin B12 118 pg/mL (87 pmol/L) Tissue transglutaminase antibody Normal Stool cultures, including an ova and parasite examination, are normal. Which of the following is the most likely diagnosis? 0 Sm all 0 . l.. er ia ac t al b st in in te M ic r os co pi c co pt io n bs or ala m se ct o La 0 lit is 0 IB S as e 0 cd ise Celiac disease IBS Lactose malabsorption Microscopic colitis Small intestinal bacterial overgrowth Ce lia A. B. C. D. E. Bacterial Overgrowth • Symptoms: diarrhea, bloating and weight loss • Signs: macrocytosis 2/2 B12 def, elevated serum folate • Common risk factors: altered gastric acid, structural abnormalities and intestinal dysmotility • Dx: hydrogen breath test or upper endoscopy with culture