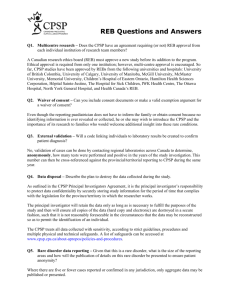
DRAFT Lactation Support in CPSP, FQHCs and Outpatient Clinics
advertisement

Lactation Support in CPSP, FQHCs and Outpatient Clinics Notes from COIN Community Clinic Call with CPSP and Medi-Cal Billing Staff June 12, 2013 CPSP Question/Scenarios: Scenario #1: Confirm that it is acceptable to bill for a CPSP Outreach worker, CPHW, to round in the hospital to make postpartum appointments. Some of these CPHWs may also provide breastfeeding support while making that visit. However the purpose of the visit, and the billable aspect of the visit, is to provide outreach and make the postpartum appointment. So the question for billing is about this as a billable outreach visit. Diana Muth (Xerox): No, because the place of service that would come across on the claim would be inpatient because at the time that they are offering the support services and making that confirmed appointment, the patient is inpatient. So no, not a billable service. Candace Gray(CPSP State Coordinator): It’s my understanding that all services for CPSP are out-patient in the clinics. Karen Farley(CA WIC Assn.): It’s not a billable event in the hospital. Scenario #2: A mother and baby are released from the hospital, but need lactation support because it was not available in the hospital, and/or a pump is needed. They can go to the community health center, on the day of discharge, and receive lactation support and the clinic can bill for the visit as a CPSP visit. Diana: Yes, as long as mom was assessed under the discipline that they plan to bill under. Yes, they do have a billable service. When patients are in-patient they obviously have a due date but day of discharge is not billable. So the patient going over from the hospital to the clinic, that day of service would be payable. Can you define what you mean by assess under the discipline? Diana: Example is: they plan to bill a postpartum service under nutrition. They would need to have done that initial nutrition assessment before they can bill under those nutrition services. That would have had to been done prenatally? 1 Diana: No, those can actually be done postpartum as long as you are using appropriate diagnosis, some of those services when it comes to breastfeeding issues can be done postpartum. So what you’re saying, Diana, is that the initial assessment should be done prior to the service being provided? Diana: That is correct. Can it be done that same day? Diana: Yes it can. If there are no other units to bill under nutrition, can they use that as a health education session? If they have billable hours? Diana: Are we talking about perinatal education, the Z-6410? Where we say it’s nonspecific, that they can do nutrition, psychosocial and health ed? Is that the one you’re talking about? Or are you talking about any of the health education services? Any health education services, so say they ran out of their nutrition hours, and they don’t have any capacity to bill, can they then use that education under health education? Any of those units? Diana: It’s not just a simple yes on that. If we can just go onto the next one? In the meantime I’m going to go online and just see what the diagnosis code range is. Because if there is no diagnosis code range available for postpartum under some of those certain health education codes then the answer would be no. If we do have postpartum diagnosis codes available under health education, the answer would be yes. But I would need to check. Jon Goldfinger(Children’s Hospital Los Angeles/AltaMed): If we have to do the evaluation prior to actually billing for the nutrition service, do we have to do the entire evaluation or can it just be the nutrition section that’s done for a given patient? Nutrition. Diana: It would just need to be under that particular section whether it be under, psychosocial, or health ed if you were not using them. Jon: Does it have to be done by the same person? Let’s say somebody else did the psychosocial on the other evaluation. Does the nutrition evaluation have to be done by the same person, or in the same visit? Or it can be done separately? 2 Diana: It can be done by different staff members, as long as the person that is providing the CPSP service to the Medi-Cal recipient is approved to do CPSP services at that particular site. Jon: When you say approved, do you mean they’ve actually been admitted by the provider or the physician as one of their service providers? Diana: They are on the list to provide CPSP services. The list they give to the PSC for that county. Each provider has proved staff, whether it be the provider, the health educator, there’s certain staff members. Basically we just call it the approved list. Is this person on the list that was submitted to the PSC for your county? Karen Clemmer(Sonoma County CPSP Coordinator): I think the simplest way to explain that is that each county Perinatal Service Coordinator has a practitioner list. That’s the list of all providers that have been approved at a clinic site to provide face-to-face CPSP services. I think that’s what Diana’s talking about, whether a different provider can do assessments in more than one area. What you want to make sure, the bottom line is that your local CPSP site/clinic has a current practitioner list and it lists all the people who would be providing face-to-face services and billing CPSP for those. Diana: Back to the postpartum health ed. The health ed assessment, as far as the codes, the Z-6414, postpartum health education assessment treatment and or intervention. If a patient runs out of nutrition units, can they go ahead and use the units under health ed? Yes we do have postpartum diagnosis codes out there. Just to give a few: postpartum care after delivery; postpartum care lactation; routine postpartum follow-up, etc. So the answer is yes. Jon: For the CPSP site, do the primary site providers have to provide obstetric services and CPSP obstetric services, in order to be credentialed as CPSP providers and bill for these other services? We’ve had a little bit of confusion about this in LA County with AltaMed. Some people seem to feel like it needs to be an obstetrician, although as a pediatrician myself, I’ve read what I understand to be the law. It seems to be that a pediatrician could do it and even though we don’t provide obstetric services we could bill for those postpartum nutrition services. Yes, absolutely. It’s not just the OBs. It’s pediatricians, family practice, GPs. Jon: So I could become CPSP certified and I could bill for those services that I am able to provide or my staff are able to provide, and my clinic regardless of whether or not we could provide the obstetric portion of CPSP? Is that correct? 3 Yes that is correct. If you’re working with an OB provider, or family practice, whoever is doing the prenatal care, you would typically have an agreement. So that doctor would then transfer that patient over to you. Karen Clemmer: You need an MOU between the OB care provider and your site because you’re not dual providers. That just spells out how you’re going to communicate and clarifies how you’ll prevent duplicity of billing. It’s totally doable. Jon: It is doable. Ok, because we’ve had some discrepancies. Do you have something in writing that says or a case study of that you come send me? We’ve had a lot of discussion in LA County, including the local department of public health coordinator, tell me that that is not doable. I think it’s because they never done it before and they don’t want to explore how to do it. But I keep explaining to them that I don’t believe that that’s the case but I don’t have any evidence for that. Can you send me something? It’s in the regulations. It’s actually in the provider hand book that is given to the providers. It has a list of all of those who can be CPSP providers and a pediatrician is one of them. FQHC/CPSP Questions/Scenarios: Scenario #1: A mother returns for a postpartum CPSP appointment and also has lactation questions. The baby has not yet enrolled in a health plan. The CPHW (IBCLC, CLE) or CPSP providers (MD, CNM, NP, PA) can bill for the postpartum visit, providing lactation support, under the mother, at the FQHC rate. Diana: Yes. Remember, there needs to be that paper trail that mom was assessed before we provide the discipline. Assuming that before we start going into treatment and/or intervention, she was assessed prior to the service. All we are now talking about is: Can this be billed under mom at an FQHC rate? The answer is yes. Karen Farley: Can that assessment could have been in her prenatal period? You mentioned before a nutrition assessment-if let’s say she’s a patient there a lot of times, prenatally, and she did her nutrition assessment, is that good postnatally, or do you have to do another nutrition assessment? Or just start in with her lactation questions? Diana: As long as she was assessed at any time during her pregnancy or postpartum. The key is that initial assessment. 4 Lynn Thiebaud(Contra Costa County Public Health): You have listed under the CPSP providers different disciplines but you don’t have RN’s. Would it be ok if it was an RN? Yes, an RN can be a practitioner. Robbie Gozalez-Dow(CA Breastfeeding Coalition): Let’s say the mom had an OB provider that is a CPSP provider, and then she goes to the pediatrician and they’re a CPSP provider and they can provide the postpartum CPSP services and provide her with lactation care. If the assessment was already done at the OB, does that count as the assessment or can you bill for the assessment twice? Diana: It’s my understanding from years ago, I started doing CPSP 16 years ago, and it’s my understanding that as long as the patient was assessed, whether the patient was assessed with the pediatrician, the patient was assessed with her family practice provider, her OB, they can accept the records from the previous provider and just have those in the patient’s charts. So they don’t actually have to assess the patient as long as they have the records that the patient was assessed. If something has changed in my 16 years, if somebody can let me know. Karen Clemmer: What about the Individualized Care Plan? Is that a requirement? Because that’s what I’ve always understood. Diana: So we’re talking about the ICP, there still needs to be, it’s my understanding, the individualized care plan, if the patient is just walking in, like postpartumly and is needing a service but somebody has had to have done that and they can transfer the records. There needs to be that paper trail that this patient was assessed at some point. Before you can get into the treatment and/or intervention services, the patient needed to be assessed. Somebody needed to develop that care plan before we go into treatment and/ or intervention services. Susan Aldana(Harbor UCLA): Even though her situation: her health challenges, or obviously her lactation challenges, were different for postpartum than they were early in pregnancy, the same assessment is still considered valid? What if you feel like there really needs to be another assessment done because her situation is completely different now? Diana: Whenever the assessment or the care plan is changing, obviously we would need to add to what was already developed, we would add to that. Once we see that we’ve got everything in place then we would do the treatment and/or intervention so assess as necessary: whether that be the first trimester, second trimester, third trimester, I need to assess postpartum. They’re going to need to be assessed before you can provide the discipline 5 and make sure that that patient is basically on track. Anything further on that, I’m going to refer to clinical. Karen Clemmer: There’s a standard postpartum assessment tool that CPSP sites have. It’s a standard form. Scenario #2: A mother returns for a postpartum CPSP appointment and also has lactation questions. The baby is enrolled in Medi-Cal. The CPSP provider (MD, CNM, NP, PA) (Perinatal/OB Clinic/Dept.) will bill for the CPSP visit, providing lactation support, under the mother, at the FQHC rate. Diana: Yes with appropriate diagnosis. AND The IBCLC (otherwise unlicensed), working with a licensed provider (MD, NP, FNP, PA),(Family Practice/Peds Clinic/Dept.) in a 8 minute face-toface including the patient, will bill for the lactation visit, under the baby, at the FQHC rate. Diana: Yes with appropriate diagnosis. Since you were talking about lactation on this one, as long as the diagnosis is appropriate: breastfeeding problems in newborns. The answer to both would be yes. Christine Goltz(Clinica Sierra Vista): What if it’s not an IBCLC but a lactation educator or a CLC? Does that change the answer? Diana: No it does not. Please clarify that the unlicensed IBCLC can be supervised by only an MD, or any licensed staff (NP, FNP, PA) for this 8 minute face-to-face. Diana: This sounds like this is more of a PSC question or maybe a Candace question. As long as the person’s on the list. Basically we go by Title 22 guidelines which you guys know they’ve worked in an OBrelated setting for one year or more and they’ve got a high school diploma. So as far as a billable service for CPSP, as long as the person’s on the list, then I would say yes but I’m going to also defer to programs. Karen Clemmer: One of my concerns with scenario #2: it’s saying that you’re going to bill under the baby. I was thinking this is not CPSP billing because CPSP only covers mom for 60 days postpartum. 6 Diana: It says the baby is enrolled in Medi-Cal, we could also bill for the baby as long as the diagnosis is appropriate. Let’s say that we were going to keep it as simple as feeding problems in newborns that would be a billable diagnosis with a medical visit code of 01. That would not be CPSP services. That is just a newborn visit. We’re keeping it out of CPSP. Mom is under CPSP. The second bullet doesn’t say anything about CPSP. Just that baby’s enrolled in MediCal. Karen Clemmer: I know that CPSP has the units. If we’re talking about a baby-billing Medi-Cal, is there the same criteria that it has to be at least 8 minutes face-to-face or is there some different measure? Diana: It’s different. They go by medical decision making of moderate complexity and it needs to be a face-to-face encounter with a licensed staff member. Carol Swain(Natividad Hospital): If you’re seeing both mom and baby on the same day then you can bill a CPSP visit for the mom AND a Medi-Cal visit for the baby and that’s not double dipping? Diana: As long as we have documentation to support that mom was seen, and we have documentation to support, in a different chart, that baby was seen, it’s not double dipping. It’s two different services: mom is a CPSP service-they’re providing lactation support to mom but then they also had a face-to-face with baby to deal with let’s say feeding problems. Karen Farley: Yes, because you can’t breastfeed without one of the other. So they are two patients, and two billable events. Diana: We don’t have a time frame. Obviously for CPSP there needs to be at least 8 minutes or more. With a baby, we don’t have a time limit. There is no time limit. Diana: These are two different visits whether they were in the same room or not, it was two different visits provided on the same day. One is a CPSP, one is a regular Medi-Cal. Documentation in both charts to support both services were rendered. Karen Clemmer: One’s servicing mom, and one’s servicing baby. Two visits, two people, two bills. Scenario #3: 7 A mother comes to an eligible CPSP appointment for breastfeeding help/support. The baby is at the office for the 3 day post discharge check. An IBCLC (otherwise unlicensed) sees the mother for sore nipples and concerns about her milk supply. She bills for a CPSP appointment. Yes. AND A licensed provider (MD, NP, FNP, or PA) sees the baby for its 3 day post discharge appointment and bills under the baby at the FQHC rate. Yes. Scenario #4: A mother comes in to an eligible CPSP appointment for breastfeeding questions. The Medi-Cal enrolled baby is scheduled for a weight check. An IBCLC (otherwise unlicensed) sees the mother for concerns regarding her milk supply and feeding frequency. She bills for CPSP appointment. Yes AND A licensed provider (MD, NP, FNP, or PA) sees the baby for the weight check and assessment and bills under the baby at the FQHC rate. Yes Scenario #5: A mother seeks lactation assistance after her CPSP coverage period has ended. She has no medical coverage. The baby is enrolled in Medi-Cal. A licensed provider (MD, NP, FPN, PA)(Family Practice/Peds. Clinic/Dept.) will bill for the lactation visit under the baby, at the FQHC rate. Yes. This would be considered a visit under Medi-Cal not CPSP. OR The IBCLC (otherwise unlicensed), working with a licensed provider (MD, NP, FNP, PA),(Family Practice/Peds Clinic/Dept.) in a 8 minute face-toface, including the patient, will bill for the lactation visit, under the baby, at the FQHC rate. Diana: Yes, but it’s one visit. In this situation it’s one visit under the baby because mom has no coverage. Karen Clemmer: Can an IBCLC bill for the services provided to the baby through Medi-Cal or only a licensed provider? Diana: Since we’re billing under Medi-Cal then it has to be a licensed provider. 8 Karen Clemmer: If I’m an IBCLC and an RN, and I’m helping this baby and mom, and billing under the baby, mom does not have Medi-Cal, and I’m supervised by a physician who is not in the room, can I bill Medi-Cal for that visit? Diana: I’m going to defer to programs. I know that an RN can be a practitioner, but working under a licensed provider. I know because we’re in the FQHC part of it, an MD does need to pop in and see that everything’s ok. It says “working with” so I’m assuming that they’re together, and that is a billable moment. Diana: Not just being supervised. The person popping their head in and checking on the patient. Diana: It says “working with” a licensed provider, so I’m assuming that both of them provided this service. As long as both of them were a part of the visit, I would say yes. Both scenarios say “working with” not supervised by. Karen Clemmer: The 8 minutes is not related to Medi-Cal, that is CPSP? Diana: Correct. Meg Beard(Santa Barbara County WIC): There is a document dated January 7, 2009-it is not real clear but may not require the presence of a physician practitioner. Titled: “Medi-Cal Breastfeeding-Related and Evaluation and Management Billing Services Update” from Department of Healthcare Services, Medi-Cal. http://files.medi-cal.ca.gov/pubsdoco/newsroom/newsroom_10133.asp So we assume according to this one does not need a doctor. Karen Farley: We can share it with everybody to get a better answer to that. Scenario #6: A mother seeks lactation assistance after her CPSP coverage period has ended, but she now has Medi-Cal. And the baby is enrolled in Medi-Cal. An IBCLC(otherwise unlicensed) working with a licensed provider (MD, NP, FNP, PA) (Family Practice Clinic/Dept.) in a 8 minute face-to-face, including the patient, will bill for the mother’s lactation visit. Diana: Depending on the mom’s Medi-Cal eligibility. It says that mom’s CPSP coverage period has ended but she now has Medi-Cal. As long as we have full scope Medi-Cal and not some sort of restricted MediCal, we do have a billable service for mom. And then baby would be yes, billable service. 9 Karen Clemmer: Is there still an 8 minute face-to-face criteria? I think that’s somewhat confusing if we’re talking about Medi-Cal. Diana: If we’re talking about Medi-Cal, we don’t have that CPSP, 8 minute criteria. AND A licensed provider (MD, NP, FNP, PA) (Family Practice/Peds Clinic/Dept.) could bill for the baby for services related to the baby and lactation. This could include a weight check, developmental check, suck check, etc. Karen Clemmer: After mom delivers her baby, and when she’s pregnant she had Medi-Cal, there’s a strong assumption that baby would qualify for Medi-Cal. If I’m an FQHC site and I’m seeing mom and baby, baby has not been established with Medi-Cal, I can still provide the service and then bill retroactively when that Medi-Cal becomes active, is that correct? Diana: That is correct, but you can also use mom’s ID to bill for baby because baby is eligible under mom’s ID for the month of birth and month following. The billing staff would just need to make sure that they are using the appropriate information on the claim form letting us know that baby’s using mom’s ID for it to go through the system, so we know when we see the two ID’s coming in for the same date of service, it’s not looking like somebody double dipping. We can clearly see that this is baby’s claim, this mom’s is claim. Scenario #7: For home visits, for CPSP patients, can it only be a RN, or any licensed provider? Diana: Any home visits for CPSP patients needs to be done by a licensed staff member. Karen Clemmer: Yes, if a licensed provider, practicing within their scope of practice and providing service in an area that has already been assessed. So for example a RN could, an MA could not, a LVN could, and they would get their FQHC encounter rate. Outpatient Clinic: NON FQHC or CPSP Scenario #1: A mother seeks postpartum lactation assistance. Both she and the baby have Medi-Cal. An IBCLC (otherwise unlicensed) works with the mother and baby to assist with lactation support, then meets with a licensed provider (MD, NP, 10 FNP, PA) (Outpatient Hospital Clinic or Family Practice or Pediatric Clinic/Dept.) in a minimally 8 minute face-to-face visit, including the patient, to approve the plan for lactation support, and the licensed provider will bill for the lactation visit, billing under the mother or baby. Diana: Yes, because they would just be billing for traditional 99-200 series code: evaluation and management. It’s saying here that the patient is with a lactation consultant, the IBCLC, THEN meets with a licensed provider. This would fall under a 99-200 series code with the appropriate diagnosis. Yes it would be billable. OR A licensed provider (MD, NP, FNP, PA) (Outpatient Hospital Clinic or Family Practice/Peds Clinic/Dept.) could bill under the mother or baby for services related to lactation support. Carol: It says an IBCLC works WITH the mother THEN meets with the licensed provider, so does that mean the licensed provider is WITH the IBCLC? Or can this be a supervised by, but not seen by the provider? Defer to programs. Carol: There’s no 8 minute guideline for that? If provider came in during the visit and took a look at mom’s breasts, took a look at baby, to see what IBCLC had done but only spent like 3 minutes, but doesn’t do a full work up or anything. I’m wondering about with Medi-Cal, if there are no time limits for that provider to put hands on. Diana: We said before this scenario, no CPSP, no FQHC, so we don’t have a time limit. It’s just that face-to-face medical decision making of moderate complexity no matter what the timeframe was as long as we have documentation to support the level of Evaluation and Management service that they are providing. Scenario #2: A mother seeks postpartum lactation assistance. Both she and the baby have Medi-Cal. A licensed RN IBCLC, sees both mom and baby and provides lactation support services, usually referred by MD in hospital, but could be a self or RN referral. Services include: Weight check of infant, 24 hour infant diet recall, evaluation of average weight gain/loss of infant since discharge from hospital, evaluation of milk transfer, evaluation of breasts for adequacy of breastfeeding or of nipple trauma and 11 treatment, jaundice evaluation of infant if symptoms present with TcBili of infant skin, etc. Charting includes the reason for the mom’s visit, objective data collection, an assessment and plan, including the time spent on the consult which is usually about 60 minutes, but can be as great as 120 minutes or as few as 30 minutes. We currently have an MD who oversees the RN IBCLC, signing off on charting and billing, but without seeing the patient. Question #1: Can the mom and baby be registered separately for billing separately for each person? Diana: Can program answer? It seems to be clinical in nature. Looks like to me it would be a 99-200 series code. Looks like as long as we have the appropriate diagnosis, mom’s eligible, baby’s eligible, we have documentation again to support, it shouldn’t be a problem. Dr. Tarby would be able to answer this. Question #2: Is it better to register the mom or the baby, if only one could be registered, and which would have improved payment? Diana: In a situation where we are looking and no CPSP, no FQHC-the payment would be the same depending on what was being billed. We’re just going to be going off Medi-Cal rates so as long as we have an eligible baby or an eligible mom and the diagnosis is appropriate, there wouldn’t be any payment difference on one or the other. Question #3: Can a RN, bill, as a licensed provider, and not need the oversight of a MD or NP? Diana: We’ll need to get back to everybody. Question #4: Does Medi-Cal prefer ICD-9 codes of 676.84 for mom or 779.31 for baby or V24.1 for either? Diana: The diagnosis needs to be appropriate for the services that they’re billing. So we don’t prefer one over the other. We just look for an eligible diagnosis for the service that you are providing, a diagnosis that is appropriate and a diagnosis that is in effect at the time. Question #5: Does Medi-Cal reimburse for TcBili (This is like a point of care blood glucose, but is monitoring for jaundice)? 12 Diana: That is a reimbursable code. It falls under Automated Chemistry Test, 82247. That is a billable code and that is in the Medi-Cal manual, part 2 under Pathologies, Organs or Disease- Oriented Services, page 3. 13