ACU Vascular Clinic - Northeastern Ontario Stroke Network
advertisement

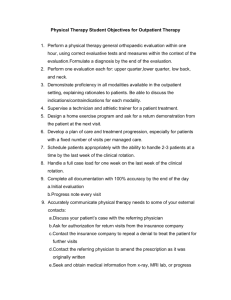
Hôpital régional de Sudbury Regional Hospital Outpatient Vascular Summit Stroke Recheck Clinic Presentation Wendy Archambault M-SLP, Reg. CASLPO, S-LP (C) Speech-Language Pathologist September 16th, 2010 Stroke Recheck Clinic History of clinic: • 1st clinic was in May 2009. • Clinic falls under the Rehabilitation & Transitions Program at HRSRH. • Clinic is a service of the Geriatric and Day Hospital. • Mandate of clinic remains as per initial structure. Stroke Recheck Clinic Goals of clinic: • To follow clients throughout the transition home and in the community upon discharge from the Intensive Rehabilitation Unit to promote and facilitate: – – – – – – Adequate follow-up at home Community re-integration Decrease falls Decrease hospital re-admissions Maximize quality of life Make recommendations re: caregiver burnout... Stroke Recheck Clinic Patient Population • Inclusion and exclusion criteria developed (trial basis) – – – – Confirmed diagnosis of stroke Residents of Northeastern Ontario Consenting and willing Living in home or residential environments (LTC excluded at this time) – Medically stable – Physician’s order as well as inter-disciplinary referral form required Stroke Recheck Clinic Patient Population: • Patients are referred upon discharge from the Intensive Rehabilitation Unit (IRU). • In accordance with Heart and Stroke best practice guidelines, follow-up appointments occur at approximately 6 weeks, 3 months and 1 year post discharge from IRU. • Clinics are on Thursday afternoons in outpatient department at HRSRH to allow for Physiatrist support. Stroke Recheck Clinic Staffing • Limited staff allocation: 0.4 Physiotherapist, 0.2 Occupational Therapist, 0.2 Speech-Language Pathologist (flexing from other caseloads). • Social Work, Recreation Therapy, Registered Dietitian, Registered Nurse and other staffing not allocated but available for consultation as needed. Stroke Recheck Clinic Current Patient Volumes • Up to 4 patients are seen in each weekly clinic. • Initially clinic was biweekly but frequency has increased to accommodate increased referrals. • There is no waitlist but wait times for recheck appointments sometimes exceed best practice recommendations due to patient volumes. • Patient volumes tend to flex based on number of stroke patients discharged from IRU. • To date 60 patient’s have been referred to this clinic. Stroke Recheck Clinic Patient Journey: • Upon arrival at clinic patient and family member register at outpatient rehab reception and are given a Stroke Impact Scale to complete. • Patient then meets with OT, PT and SLP for 45 minute appointment (complete inter-disciplinary follow-up assessment, team discussion, and documentation and initiate referrals as needed). • Questions are asked to determine currently level of function in each discipline (e.g. equipment, mobility, communication, dysphagia, cognition, community reintegration, etc.). • Current supports in place at home are identified. Stroke Recheck Clinic Patient Journey: • Gaps in service are identified and referrals are made as appropriate (e.g. OBIRS, ICAN, VON Day Centre, CCAC, Hand transit, CNIB, Outpatient OT/PT/SLP, YMCA – Support Group, Diabetes Education, Cardiac Rehab, etc.). • As needed, Dr. Graham, Physiatrist, or other allied heath team members are asked to consult in clinic. • Patient is scheduled for next recheck appointment. • Summary report from clinic sent to Dr. Graham and MRP after 1st clinic and thereafter as needed. Stroke Recheck Clinic Relationships Established with other HRSRH Programs/Clinics: • Referrals initiated from IRU. • Patient often referred to other outpatient clinics at HRSRH and in the community. Stroke Recheck Clinic Future Direction of Clinic • Plan to move to 1 full day or 2 half-day weekly clinics as volumes continue to increase. • Possible opening of clinic to referrals from other sources (e.g. Stroke Prevention Clinic). • Approval of Service Description Policy Stroke Recheck Clinic Future Direction of Clinic • Maintenance of patient database to consistently track stats and measure impact on stroke clientele. • Distribution of education about the Stroke Re-check Clinic. • Improve partnerships with community providers. Stroke Recheck Clinic QUESTIONS Hôpital régional de Sudbury Regional Hospital Outpatient Vascular Summit Outpatient Occupational Therapy Brenda Seguin O.T. Reg. (Ont) Occupational Therapist September 16th, 2010 Outpatient Occupational Therapy Patient Population: • Stroke (upper extremity treatment, cognitive, perceptual and visual assessment and treatment) • Spinal Cord injury and disease (upper extremity treatment, splinting) • ABI (splinting and upper extremity treatment) • Cognitive Impairment (dementia) • Congenital disorders such as C.P. , developmental delays,.. • Age varies from 18 and over Outpatient Occupational Therapy Current Patient Volumes • Outpatient services are available in the afternoon only (0.5 FTE) • Usually see 7-9 patients per week + the stroke re-check clinic (1x per week) • Waitlist varies according to type of referrals and current caseload i.e. 1hour sessions vs 1/2hour session Outpatient Occupational Therapy Patient Journey: • Referral from a physician or nurse practitioner • Client is placed on a wait list and then called at home to set up an appointment • Registers at the rehab outpatient reception desk • Assessment by the O.T. • Establish goals of therapy Outpatient Occupational Therapy Examples of goals for the upper extremity: • Increase strength, coordination, fine motor skills and/or • Stimulate and/or Increase active/normal movement • To decrease tone (spasticity) in the shoulder, wrist, hand, fingers • Increase functional use of the UE Outpatient Occupational Therapy Other interventions: • Splinting to provide positioning of the Upper extremity • Splinting to prevent or reduce contractures • Hand and/or wrist positioning aids to protect the palm from infection, odor, injury,… Outpatient Occupational Therapy Relationships Established with other HRSRH Programs/Clinics Outpatient physiotherapy Hand and Upper Limb Rehabilitation Stroke re-check clinic DARS (Driving Assessment and Rehabilitation Service) Referrals often initiated from IRU and from the stroke team on acute care units Outpatient Occupational Therapy Future Direction of Program • Link with the new Geriatric Day Hospital • Possible partnership with the seating clinic re:wheelchair prescription that do not need the specialty of the seating clinic. DARS Driving Assessment Rehabilitation Service Assessment for safety to drive a vehicle Assessment for driving adaptations such as hand controls, left gas pedal, spinner knob Vision Waiver Functional Assessment (specific protocol established by MTO) Vehicle Adaptation and Modification Assessment DARS Most common referrals: • Stroke • ABI • Dementia Less common referrals: • Amputee • Paraplegia • M.S., Parkinsons DARS • Referral from a physician • Fee for service (not covered by OHIP) • Includes a clinical assessment by an OT and followed by an on-road evaluation with a driving instructor and the OT. • Use of the driver instructor’s vehicle with a dual brake (NOT the client’s vehicle) • Report is sent to referring physician, other physician as instructed by the client, MTO and the client. DARS Possible Outcomes: Continue or resume driving if MTO and physician agrees Driving lessons and repeat road test MTO road test Driving with adaptations No driving recommended DARS • For more information and for the referral form, please contact the secretary: Lise Morrissette ext. 7098 Thank you! Hôpital régional de Sudbury Regional Hospital Outpatient Vascular Summit Cardiac Rehab September 16th, 2010 Cardiac Rehabilitation Program History 1970’s - Community-based program at Laurentian University, then moved to community fitness facility “Connie Lou’s Gym”. Cardiac Rehabilitation Program 1985 • Program Moved to Sudbury Arena as part of the Cardiovascular Program. Cardiac Rehabilitation Program 1991 • Recovery program established in the Medical Arts Building. Cardiac Rehabilitation Program 2000 • Programs combined at Centre for Life. Cardiac Rehabilitation sits within the HRSRH Critical Care Program Initial mandate To assist with the modification of risk factors in patients with established coronary disease in an effort to prevent disease progression and recurrence of cardiac events. Current mandate To provide interventions to enhance and maintain • Physical • Psychological • Vocational Status of individuals with established heart disease or those at high risk for the development of heart disease for both local and regional clients. Multidisciplinary Model • Medical Director • RN EC • RN • Clinical Exercise Specialist • PT • Kin • RD • Psychological Associate Client Inclusion Criteria MI Stable angina CABG PTCA Compensated Heart Failure Cardiomyopathy Transplant Valvular Arrythmias Pacemaker/ICD PAD Programs offered Education Exercise: Aerobic & Resistance Smoking Cessation Heart Failure Stabilization Regional Satellites Hydrotherapy PAD Home Program Vocational Chronic Disease Patient Self Management Client Population 70 60 50 40 Female Male 30 20 10 0 Gender ** Average client age- 62 years Referral Location Covers an area of approximately 185,000 km2 Satellite Programs Espanola Little Current Sturgeon Falls Kirkland Lake New Liskeard Sault Ste. Marie Total Referrals 2003-2010 Hundreds 16 14 12 10 8 6 4 2 0 In town Out of town Client Visits Thousands 18 16 14 12 10 8 6 4 2 0 2005-06 2006-07 2007-08 2008-09 2009-10 Client Journey Referral Risk Stratification Multi-Disciplinary Intervention Intake Diagnostic Testing Case management Exercise Reassessment Education On site Web cast OTN Discharge On site Home Relationships Established with other HRSRH Programs/Clinics Pulmonary Rehab Community Asthma Clinic Diabetes Education Nutrition Counselling Pre-admission Respiratory therapy Cardiology Cardio diagnostics Stroke clinic/Vascular unit ABI Tobacco Cessation Future Direction • Enhanced Heart Function Clinic • Expansion of Pulmonary Rehab Collaboration • New linkages with other clinics and/or patient populations Hôpital régional de Sudbury Regional Hospital Outpatient Vascular Summit Stroke Prevention Clinic September 16th, 2010 Stroke Prevention Clinic 2 minute history of clinic: • Date started: April 2006 • Initial mandate: Provide timely access to diagnostic and medical follow-up for patients presenting with a recent transient ischemic attack (TIA) to prevent progression to a completed stroke • Part of Emergency and Medical Program • Location: Neurology/Stroke Prevention Clinic – 1st Floor South Tower Stroke Prevention Clinic Patient Population: • Diagnoses followed: – TIA (Transient Ischemic Attack) – Non-disabling stroke • Average age = 65 years • Male/female split = 50/50 • Referrals received from (2009/10 data) – HRSRH ED (42%) – HRSRH Inpatients (27%) – Sudbury and Area Physicians (24%) – Community Hospital ED’s (7%) Stroke Prevention Clinic Patient Volumes • # Referrals to Clinic/Year Year # New Pts # Visits 2006/07 122 174 2007/08 227 287 2008/09 272 448 2009/10 247 507 2010/11 280 (proj.) 560 (proj.) Stroke Prevention Clinic Patient Journey: • Referral Made (e.g. from HRSRH Emergency Dept); initial education provided through patient folder in ED • Appointment date is based on triage level (using validated tool) – avg. wait 3-7 days • Prior to 1st visit with physician, each patient is booked for CT Head, Carotid Doppler, Lab Work (fasting blood sugar, lipid profile, AST, ALT and CK) and a nurse visit (includes risk factor education) • Physician visit – complete neurological examination – diagnosis – risk factor management – further testing (e.g. MRI or CTA) if necessary Stroke Prevention Clinic Patient Journey (cont’d) • Follow-up visits in clinic booked for test results and/or medication review • Ongoing medical management provided by family physician • Orphaned patients remain an outstanding issue Stroke Prevention Clinic Relationships Established with other HRSRH Programs/Clinics • Outgoing referrals include – Vascular Surgery – Neurology – Cardiology – Geriatrician (Dr. Clark) – Cardiac Rehab – Smoker’s Helpline – Nutrition Counselling – Diabetes Education – Outpatient Neuro PT and OT Stroke Prevention Clinic Future Direction of Clinic/Program Definite: 1. Develop process to provide more comprehensive follow-up for discharged acute stroke patients (55-60% of stroke admissions at HRSRH are discharged home from acute care with no formal clinic follow-up) – 1st Step: follow-up of patients discharged from acute care by Hospitalist team – Possible 2nd Step – provide follow-up for patients discharged by family physicians - These 2 scenarios would add approximately 140200 new patients/year to the clinic Stroke Prevention Clinic Future Direction of Clinic/Program (cont’d) Possible: 1. In collaboration with Inpatient Stroke Program – develop a Hypertension Education Program Stroke Prevention Clinic Identified Gaps in Outgoing Referrals • Smoking Cessation Counselling (vs. phone #) • Wait List issues with Outpatient Neuro OT and PT Stroke Prevention Clinic • Questions? Hôpital régional de Sudbury Regional Hospital Outpatient Vascular Summit Outpatient Neuro Physiotherapy September 16th, 2010 Outpatient Neuro. Physio 2 minute history of clinic: • Started approximately 20+ years ago • Physiotherapy assessment and treatment is provided to individuals with neurological conditions with the aim of treatment being to recover function and to help them integrate safely into the community following discharge from the rehabilitation unit. • Individuals from the community who suffer from neurological conditions, vestibular dysfunctions or individuals needing a walker prescription are also seen by this service. Outpatient Neuro. Physio Priorities: • Referrals from Intensive Rehabilitation Unit, Specialists, and “high fall risk” clients. • This service falls under the Rehabilitation and Transitions Program Outpatient Neuro. Physio Staffing: • 0.6 FTE Physiotherapist Patient Population: • C.V.A., A.B.I., Spinal Stenosis, Neuropathy, Amputees, M.S., P.D., Vestibular Dysfunction,Spinal Stenosis, etc. Referrals from: Dr. Graham/I.R.U., Specialists, G.P.’s, Geriatrician-Dr. Clarke Average Age of Patients: 65 Outpatient Neuro. Physio Current Patient Volumes: • 2009- averaged 7 new referrals/mo. • 2006- averaged 6 new referrals/mo. Current Waitlist: • Urgent neuro - 4 weeks • Semi-urgent neuro - 4 months • Chronic neuro - 2 years,10 months Outpatient Neuro. Physio Patient Journey: • Client is deemed to need more physio after d/c, or a new diagnosis. • In the community, physician makes referral to outpatients. Screened by secretary to see if have private coverage. • 1 hour initial assessment: H.P.I., P.M.HX., Discuss: Any issues since d/c, fall hx, pain, functional limitations, education++ s+s of stroke, or of their dx./ sequelae. Outpatient Neuro. Physio Patient Journey: • Physical Ax. : strength, ROM, balance, gait ax., sensation etc. • One hour appointments. –work on goals established at beginning, monitor change and ascertain well-rounded home ex. program • May consult with O.T., ABI team, refer for pool therapy. Outpatient Neuro. Physio Patient Journey: • Refer to: ICAN, VON daycentre, OBIRS. • May re-check ie. Diagnoses that deteriorate every 6 months. P.D., M.S. Outpatient Neuro. Physio Relationships Established with other HRSRH Programs/Clinics: • OBIRS • Oupatient O.T. • Pool Therapy • Stroke Re-check Clinic • Dr. Clarke Outpatient Neuro. Physio Future Direction of Clinic: • Geriatric Day Hospital • Vestibular Rehab. Clinic Outpatient Neuro. Physio • Questions? Hôpital régional de Sudbury Regional Hospital 2010 Outpatient Vascular Summit Medical Imaging Thursday, September 15, 2010 Medical Imaging Medical Imaging supports outpatient clinics in three ways. 1. Outpatient Testing and Diagnosis 2. Therapeutic vascular interventions 3. IHF ownership and physician partnership Service Description Relevant Outpatient Services include • General Radiology and fluoroscopy • All angiographic and interventional special procedures except cardiac angiography • CT scanning (Dual side by Side 64 slice) capable of arterial/venous angiography via venous injections. • MRI scanning (Single 16 channel) capable of arterial/venous angiography via venous injections • Ultrasound arterial and venous assessments Service Description North Tower (Located on the 2nd floor, north of the OR’s and the ER) • • • • • • • • • • • • This Primary Inpatient or Outpatient therapeutic interventions department includes 3 Digital radiology rooms 1 Inpatient fluoroscopy room 3 Ultrasound suites 2 64slice CT scanners 1 MRI 2 Digital Angiography suites 24/7 Technical Area 6 Bed recovery area Outpatient Interventional Preadmission Suite Reception and Registration Stretcher holding capacity separate from patient waiting. North Tower Hours of Operation • • • • • • • NT General Radiology will be staffed 24 hours a day; 7 days a week with booked examinations and procedures 8 hours a day, 5 days a week (M-F). NT General Radiology ER Suite is staffed 24 hours a day; 7 days a week with backup support and trauma pager coverage. NT Angiography Services will be offered 8 hours per day (0800-1600), 5 days per week. Call services are available 24/7. NT Ultrasound will book examinations 14 hours a day, 5 days per week (M-F)(0700-2100). Saturdays and Sundays 9 hours (0800-1700). CT and MRI services will be offered as per today’s standards provided that MOH Wait time funding is maintained. Call will be offered 24/7 for ER and specialist emergencies. CT North Tower operational 17 hours per day (M-F) (0700-2400) plus call 24/7. Saturday-Sunday 8 hours (0730-1530). MRI North Tower operational 16 hours per day, 7 days a week. (07002300) plus call. Service Description South Tower (Located on the 2nd floor, adjacent to ACU) • • • • • • • • • • • This Primary Outpatient department will include; 2 Digital radiology rooms 2 Conventional radiology rooms with CR 1 Digital outpatient fluoroscopy room 4 ultrasound Suites 2 Digital mammography rooms 1 Digital Prone Stereotactic Biopsy table Central Bookings Reception and Registration File Room Administration South Tower Hours of Operation • Important Note: The South tower designed as an outpatient center, was never planned to accommodate Inpatients and does not have the capacity to accommodate Inpatients. As a result, upon consolidation, all inpatient services with the exception of Nuclear medicine will be performed in the North Tower. The only planned exceptions will be ERCP patients who will be serviced in the South Tower Fluoroscopy room. • ST General Radiology will be staffed 10 hours per day, Monday to Friday (700-1700). • ST Ultrasound will book examinations 10 hours a day, 5 days per week (M-F). (0700-1700) • ST Mammography will be offered 10 hours per day, Monday to Friday (0700-1700). • ST Nuclear Medicine will be offered 10 hours per day, Monday to Friday. (0700-1700). Sudbury Vascular Lab • Outpatient Vascular Ultrasound clinic run in conjunction with VINO (Vascular Institute of Northern Ontario). Questions? Hôpital régional de Sudbury Regional Hospital Outpatient Vascular Summit Tobacco Dependence Treatment Initiative September 16th, 2010 Tobacco Dependence Treatment Initiative • Expansion site for Ottawa Model-UOHI • Advisory Committee formed, Coordinator hired-policies, tools created, best practices examined, limited implementation of Ottawa Model begins in 2007 • Additional funding-2009-2011 through Federal Tobacco Strategy-Regional Expansion; partnership with three other hospitals • Currently housed under Preventive Oncology & Screening Division-RCP Tobacco Dependence Treatment Initiative Patient Population: • Initial pilot began on vascular, thoracic and urology surgical unit-baseline tobacco use prevalence rate is 37% (used tobacco in last 6 months) • Expansion to Cardiology unit-baseline tobacco use prevalence rate is 22% • 68% prevalence rate-inpatient psychiatric unit Nurse hired to develop in-patient policy and procedures for this specialized population • Some outpatient clinics-CCS Fax Referral Program Tobacco Dependence Treatment Initiative Current Patient Volumes • Under FTS Grant Baseline patient enrolment 144-November2009-February 2010 (patients given usual care) • Intervention group February 2010September 10- (196 patients counselled and given option of IVR follow-up) • NRT available hospital wide through preprinted order Tobacco Dependence Treatment Initiative Patient Journey: • Upon identification of patient as having used tobacco within last six months, hospital-wide pre-printed order is used to initiate provision of NRT. Training re NRT guidelines for front line staff is currently being held. • On units where Nurse Counsellor provides service, patient is visited, consultation form filled out, counselling provided, NRT prescribed, post discharge support offered in form of Interactive Voice Response and referral to available community resources. Tobacco Dependence Treatment Initiative Internal and external partnerships • Psychiatric Inpatient unit • Fax Referral program (Stroke Program, DECP, RCP, Cardiac Pulmonary Rehab) • FTS Regional Partnership- 3 hospitals • OHSS Tobacco Cessation Program • Aboriginal & Francophone groups • TCAN and Cessation sub committee • UOHI • TEACH-CAMH • June 2009 Regional Conference Tobacco Dependence Treatment Initiative Future Directions • Introduction of smoke free grounds-July 2010-Staff, volunteers, students, contractors • Patient ban to follow with additional smoking cessation support (possibly early 2011) • Expansion of Fax Referral Program to additional outpatient units • Exploring sustainable funding Tobacco Dependence Treatment Initiative Future Directions cont’d… • HRSRH Board is establishing a quality indicator related to smoking cessation. Need to establish a consistent systematic, mandatory mechanism for recording the smoking status of all patients admitted to HRSRH Hôpital régional de Sudbury Regional Hospital Outpatient Vascular Summit OBIRS September 16th, 2010 OBIRS (Outpatient Brain Injury Rehab Service) • Established in 1990, part of the Rehabilitation & Transitions Program • An adult (16+) out-patient program specializing in post-acute rehab services for individuals with a confirmed diagnosis of brain injury. • An Interdisciplinary team which provides assessment and rehabilitation therapy to assist the client in returning to their identified roles at home and in the community. OBIRS-Interdisciplinary Team • • • • • • • Social Worker Speech and Language Pathologist Occupational Therapist Psychological Associate Recreation Therapist Case Manager Program Secretary OBIRS: Admission Criteria Individuals must have a documented, established diagnosis of an Acquired Brain Injury defined as: • Occurs at least 7 days after birth and is not related to a congenital disorder or developmental disability, (e.g., cerebral palsy, muscular dystrophy, autism, spina bifida) or a process which progressively damages the brain, (e.g., dementing processes, MS, Alzheimer’s Disease, Parkinson’s Disease) OBIRS: Admission Criteria • Damage to the brain caused traumatically e.g., from an external force such as collision, fall, or assault • Damage to the brain caused through a medical problem or disease process which causes damage to the brain e.g. anoxia, nonprogressive tumour, aneurysm, infection, stroke with diffuse cognitive deficits OBIRS: Participate to Learn • A Rehab approach which aims to reduce the client’s need to generalize the strategies being learned to their ‘real life’ situations. • Therapy is conducted within the home, workplace, on-site or in the most relevant community setting. This requires more active involvement of the client and their support system and increases the likelihood carryover and longer-term success. • “Roles as Goals”---Goals should be developed jointly and be meaningful to the client and their families. OBIRS: Referral Source 36% 64% IRU Inpatient Transfers (N= 29) Outpatient Referrals (N=52) OBIRS: Referral Distribution Region 26% Sudbury/Manitoulin 74% Sudbury/Manitoulin 74% North East Region 26% OBIRS 2009/10 Referral Pattern 60 50 40 30 20 10 0 Sudbury Manitoulin North Bay Parry Sound Elliott Lake/Blind River Espanola/Birch Island Kirkland Lake Temiskaming Sault Ste Marie Wawa Timmins OBIRS Wait list Management A Priority system based on the following: I. II. III. IV. Individuals preparing for discharge from an inpatient program with a primary diagnosis of ABI Individuals identified through ABI Case Management Individuals less than 3 years post-injury at the time of the referral All other referrals are prioritized according to date received. OBIRS Referral/Rehab Pathway ABI referral received Reviewed and Placed on wait list Intake Assessment Interdisciplinary Team Assessment & Review (as needed) Referrals to other Services as appropriate Feedback to client & referral sources and Individualized Goal development Pre-testing Active Rehabilitation (group, individual Community based) (Length of stay varies) Case Conference review 6-8 weeks Discharge & Post-testing Case Management Follow-up up to 1 year Family Involvement OBIRS: Alternate Pathway • If a client already has clearly defined deficits and treatment needs (i.e. already assessed elsewhere) they may move directly into active treatment • Clients being transferred from an inpatient acquired brain injury program move directly into active treatment OBIRS: Outreach Consultation • Regional clients may be assessed in-person with the assistance of Health Travel Grants, by the Ontario Telehealth Network or in their home communities by 1-2 members of the Interdisciplinary team • Assessment results and recommendations are provided to local services for implementation and follow-up • Some clients may obtain ongoing treatment using OTN or direct travel to Sudbury if preferred. OBIRS: Current Relationships • • • • • • • • • • ABI FLIC team/ABI Service Continuum Out-patient Neuro Physiotherapy Stroke Re-check clinic Cardiac Rehab Service (Rec Therapist) Mental Health & Addictions (SUBI, Bridging) Neurology Forward to Function (Chronic Pain, WSIB) Trauma Services Driving Assessment Service Cancer Program OBIRS: Future Relationships? • Trauma Team (Concussion Clinic) • Geriatric/Adult Day Hospital • Children’s treatment Center (adolescent transition) • Strengthened relationship with Psychiatry/Mental Health & Addictions • Strengthened relationships with Cancer Program • Professional Practice/NOSM/Laurentian • Education and Awareness of ABI across organization OBIRS: External Relationships • • • • • • Ontario March of Dimes Ontario Brain Injury Association Toronto Rehab & ABI Network Neurotrauma Foundation CHIRS/CAMH Case Management companies/WSIB/Insurance Companies • North-eastern Ontario ABI Network • Academic Affiliations Hôpital régional de Sudbury Regional Hospital Outpatient Vascular Summit A.C.U. Vascular Clinic September 16th, 2010 A.C.U. Vascular Clinic History of clinic: • Introduced in 2007 • Initially to see 6-8 vascular patients • Currently 18-25 vascular/complex wounds per week • Falls within A.C.S. / D.S.A.C.P. A.C.U. Vascular Clinic Patient Population: • Quantitative data not collected • Complex wound patients related to diabetic ulcer venous ulcer post-op amputations other (some skin cancers discovered) A.C.U. Vascular Clinic Annual Visits 2008-09………………… 753 2009-10………………….779 A.C.U. Vascular Clinic Current Patient Volumes Weekly clinics 18– 25 patients Year to Date: April - August 2006 2007 2008 2009 2010 121 219 279 319 345 A.C.U. Vascular Clinic Patient Journey: • • • • Patient referred to a vascular surgeon Initial booking by surgeon’s office Regular visits as required Patients seen by: - Vascular surgeon - Enterostomal Therapy Nurse - A.C.U. Nursing Staff - Medical Photographer A.C.U. Vascular Clinic Future Direction of Clinic Potential – O.D.S./ MOHLTC call for proposal: Centre for Complex Diabetes Care • Possible linkages between A.C.U., CCDC, Bayshore outpatient clinic A.C.U. Vascular Clinic • Growing need clearly demonstrated • NECCAC also looking at processes re: Diabetic Foot & venous leg ulcers • Experiencing difficulty containing vascular clinic within allocated resources. A.C.U. Vascular Clinic Thank You Hôpital régional de Sudbury Regional Hospital Outpatient Vascular Summit Outpatient Rehabilitation Presentation September 16th, 2010 Outpatient Rehabilitation Services: • • • • • • • • Chiropody Augmentative Communication Clinic Prosthetics and Orthotics Seating Clinic Outpatient Physiotherapy Outpatient Occupational Therapy Driver Assessment and Rehabilitation Service Helpline Personal Emergency Response Service Outpatient Rehabilitation Patient Population: • Adult (over 18 years) • Varies by service; includes Stroke, acquired brain injury, diabetes, dementia, multi-trauma etc. • Physician referral required (internal, external) • Self referral (Helpline) Outpatient Rehabilitation Current Patient Volumes • High referral volumes for some, not all services • Prioritization of referrals by service team • Wait times variable by service and priority of need Outpatient Rehabilitation Patient Journey: • Upon receipt of physician referral, service lead reviews and assigns priority • pt contacted with appointment by rehab reception staff • Initial visit – assessment by involved staff (dependent on service – OT, PT, Chiropodist, Orthotist, etc.) • Treatment provided (can include hands-on tx, fabrication of necessary device, education) • Discharge (follow-up available dependent on service) Outpatient Rehabilitation Relationships Established with other HRSRH Programs/Clinics • • • • Inpatient units / IRU Medical / Surgical units (ex. outpt physio) Transitional Care Unit (ex. Chiropody) Children’s Treatment Centre (P&O) Outpatient Rehabilitation Future Direction of Clinic/Program (Definite and Possible) • Geriatric and Adult Day Hospital – Linkage of existing outpt PT / OT • DARS – Driveable centre • Use of new technology to realize improved efficiencies (ex. P&O) Hôpital régional de Sudbury Regional Hospital Outpatient Vascular Summit Geriatric and Adult Rehab Day Hospital (GARD) September 16th, 2010 Geriatric and Adult Rehab Day Hospital History: • • • • ALC Task Force Specialized Geriatric Services Committee Location – first floor north tower Program Development Geriatric and Adult Rehab Day Hospital Mandate: • To provide comprehensive multidisciplinary assessment and rehabilitation in order to help individuals maintain or improve their level of function. • The goal is to facilitate optimal independence and quality of health so that they can remain at home as long as possible • Short-term treatment, counseling, and education are available to patients and their caregivers to facilitate community support and long-term care planning. • The service is designed as an alternative to admission to hospital or to facilitate discharge and decrease current length of stay required by current in-patients. Geriatric and Adult Rehab Day Hospital The multidisciplinary team includes: • • • • • • • • • Occupational Therapist Social Worker Speech-Language Pathologist Physiotherapist Nurse Clinical Nurse Specialist Dietitian Pharmacist The individual’s family physician will manage the individual’s medical needs. • Consultation with a Geriatrician or Physiatrist may be arranged as needed Geriatric and Adult Rehab Day Hospital Services Provided: • Coordination of healthcare services and community resources • Health education • Links with social and leisure activities • Maximization of mobility and improved physical wellness • Assessment of cognitive abilities • Assistance with depression and anxiety issues • Home safety • Hydrotherapy • Caregiver stress • Communication difficulties and swallowing issues • Nutrition and weight loss • Medication review, monitoring and counseling Geriatric and Adult Rehab Day Hospital Patient Population: • Must require a comprehensive multidisciplinary approach to rehabilitation to attain maximum functional independence. • Must be 65 years of age or older for the Geriatric stream and 18 of age or older for the Adult stream. • Must be a resident of the Sudbury Region. • Must be medically and psychiatrically stable and be able to tolerate travel to and from the program in addition to the therapy provided. • Must be willing and able to engage at a purposeful level and be sufficiently oriented to their surroundings. • Must have the potential to achieve realistic and self-directed goals. • A tolerance level to attend on average two-and-a –half hour session twice a week for 6 to 8 weeks is required. Geriatric and Adult Rehab Day Hospital Current Activity • Referral Process • Intake process • Metrics • First patient activity – SLP – Dietitian Geriatric and Adult Rehab Day Hospital Relationships: • GEM • In-patient units • NE RGP • NECCAC • Community Supports Geriatric and Adult Rehab Day Hospital Future Direction: • Out patient OT • Outpatient PT • Stroke Re-Check • Value added services