Management of Penetrating Neck Trauma
advertisement

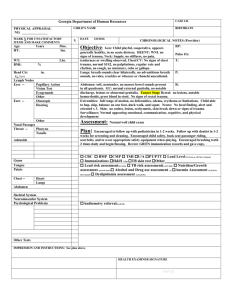
Management of Penetrating Neck Trauma Ottawa Civic MVA, aphasia, R hemiplegia Types of Weapons Low velocity – knives, ice picks, glass High velocity – handguns, shotguns, shrapnel Guns Ballistics Anatomy Anatomy Incidence and Mortality Signs of Injury: Signs of Injury: Initial Management Management of the Stable Patient: The Standard: The Standard: Based on wartime experiences Fogelman et al (1956) : immediate neck exploration-> better outcomes in vascular injuries. negative neck explorations in > 50% Arteriogram? screening tool before exploration zone 1 and 3 injuries hard to detect on physical Safe answer on board exam… Arteriogram Flint et al (1973): negative P.E. in 32% of pts. with major zone 1 vascular injury. Arteriogram can be accompanied by treatment (e.g. embolization). A Newer Algorithm Mansour et al 1991 retrospective study Newer Algorithm (Mansour) 63% of the study population was in the observation group. Overall mortality 1.5% similar to those in more rigorous treatment protocols. Similar results obtained in other large studies with similar protocols (e.g. Biffi et al 1997). NOTE: Arteriogram in asymptomatic patients with zone 1 injury. Points of Controversy: Most trauma surgeons accept observation of select patients similar to the Mansour algorithm. Study by Eddy et al questions the necessity for arteriogram / esophagoscopy in asymptomatic zone 1 injury (use of P.E. and CXR resulted in no false negatives). Other noninvasive modalities than arteriogram exist for screening patients for vascular injury. CT scan Can id weapon trajectory and structures only in stable patients. Gracias et al (2001) CT scan in stable patients: able to save patients from arteriogram indicated by other protocols 50% of the time avoid esophagoscopy in 90% of tested patients who might otherwise have undergone it. Duplex Ultrasonography Requires the presence of reliable technician and radiologist. A double blinded study by Ginsburg et al (1996) showed 100% true negative, 100% sensitivity in detecting arterial injury, using arteriography as the gold standard. Is this really wise?? Incision for Neck Exploration: Incisions for Neck Exploration: Management of Vascular Injuries: Common carotid: Internal carotid: Shunting is usually necessary Vertebral: repair preferred over ligation in almost all cases. Saphenous vein graft may be used. Shunting is rarely necessary. Thrombectomy may be necessary. Angiographic embolization proximal ligation can be used if the contralateral vertebral artery is intact. Internal Jugular: Repair vs. ligation. Esophageal Injury: Diagnosis: Controlled fistula with T-tube esophagoscopy and esophagram in symptomatic patients. Injection of air or methylene blue in the mouth may aid in localizing injuries. exteriorization of low non-repairable wounds Small pharyngeal lesions above arytenoids can be treated with NPO and observation 5-7 days All patients should be NPO for 5-7 days. Laryngeal/Tracheal Injury Thorough Direct Laryngoscopy for suspicious wounds Tracheotomy for suspected laryngeal injury Thoracic Trauma Thoracic Trauma 2nd leading cause of trauma deaths after head injury 10-20% of all trauma deaths Many deaths are preventable Thoracic Trauma Mechanisms of Injury Blunt Injury Deceleration Compression Penetrating Injury Combination Thoracic Trauma Anatomical Injuries Thoracic Cage (Skeletal) Cardiovascular Pleural and Pulmonary Mediastinal Diaphragmatic Esophageal Penetrating Cardiac Thoracic Trauma Hypoxia Hypercarbia in intrathoracic pressure relationships level of consciousness Impairments to cardiac output hypovolemia pulmonary V/P mismatch in intrathoracic pressure relationships blood loss increased intrapleural pressures blood in pericardial sac myocardial valve damage Acidosis – final result hypoperfusion of tissues Thoracic Trauma Initial exam directed toward life threatening: Injuries Open pneumothorax Flail chest Tension pneumothorax Massive hemothorax Cardiac tamponade Thoracic Trauma Assessment Findings Mental Status Pulse narrow PP, hyper- or hypotension, pulsus paradoxus Ventilatory rate & effort absent, tachy or brady BP decreased tachy- or bradypnea, labored, retractions Skin diaphoresis, pallor, cyanosis, open injury, ecchymosis Thoracic Trauma Assessment Findings Neck Chest contusions, tenderness, asymmetry, abN a/e, bowel sounds, abnormal percussion, open injury, impaled object, crepitus, hemoptysis Heart Sounds tracheal position, SQ emph, JVD, open injury muffled, distant, regurgitant murmur Upper abdomen contusion, open injury Thoracic Trauma Assessment Findings ECG (ST segment abnormalities, dysrhythmias) History Dyspnea Pain Past hx of cardiorespiratory disease Restraint devices used Item/Weapon involved in injury Thoracic Trauma Specific Injuries Rib Fracture MC chest wall injury from direct trauma More common in adults than children Especially common in elderly Most commonly 5th - 9th ribs Poor protection Rib Fracture Fractures of 1st and 2nd second require high force Frequently have injury to aorta or bronchi Occur in 90% of patients with tracheo-bronchial rupture May injure subclavian artery/vein 30% will die Rib Fracture Fractures of 10 to 12th ribs can cause damage to underlying abdominal solid organs: Liver Spleen Kidneys Rib Fracture Management PPV Analgesics for isolated trauma Non-circumferential splinting Monitor elderly and COPD patients closely Broken ribs can cause decompensation Patients will fail to breathe deeply and cough, resulting in poor clearance of secretions Sternal Fracture Uncommon, 5-8% in blunt chest trauma Large traumatic force Direct blow to front of chest by Deceleration steering wheel dashboard Other object Sternal Fracture 25 - 45% mortality due to associated trauma: Disruption of thoracic aorta Tracheal or bronchial tear Diaphragm rupture Flail chest Myocardial trauma High incidence of myocardial contusion, cardiac tamponade or pulmonary contusion Sternal Fracture Management Establish airway High concentration oxygen Assist ventilations as needed IV NS/LR Restrict fluids Rule out associated injuries Flail Chest Usually secondary to blunt trauma Most commonly in MVA Also results from falls from heights industrial accidents assault birth trauma More common in older patients Flail Chest Mortality rates 20-40% due to associated injuries Mortality increased with advanced age seven or more rib fractures three or more associated injuries shock head injuries Flail Chest Consequences of flail chest Respiratory failure due to pulmonary contusion inadequate diaphragm movement Paradoxical movement of the chest must be large to compromise ventilation Increased work of breathing decreased chest expansion pain Flail Chest Suspect spinal injuries Establish airway Assist ventilation Treat hypoxia from underlying contusion Promote full lung expansion Consider need for intubation and PEEP Mechanically stabilize chest wall questionable value Flail Chest Management IV of LR/NS Avoid rapid replacement in hemodynamically stable patient Contused lung cannot handle fluid load Monitor EKG Chest trauma can cause dysrhythmias Simple Pneumothorax Incidence 10-30% in blunt chest trauma almost 100% with penetrating chest trauma Morbidity & Mortality dependent on extent of atelectasis associated injuries Simple Pneumothorax a # rib lacerates lung Usually well-tolerated in the young & healthy Severe compromise can occur in the elderly or patients with pulmonary disease Degree of distress depends on amount and speed of collapse Simple Pneumothorax HDI and respiratory distress High index of suspicion Chest tube when in doubt before CXR Open Pneumothorax If the trauma patient does not ventilate well with an open airway, look for a hole May be subtle Abrasion with deep punctures Opening in the chest wall Sucking sound on inhalation HDI/resp distress SQ Emphysema Open Pneumothorax Profound hypoventilation may occur communication between pleural space and atmosphere Prevents development of negative intrapleural pressure Results in ipsilateral lung collapse inability to ventilate affected lung Open Pneumothorax V/Q Mismatch shunting hypoventilation hypoxia large functional dead space Pressure may build within pleural space Return from Vena cava may be impaired Open Pneumothorax Cover chest opening with occlusive dressing Assist with positive pressure ventilations prn Monitor for progression to tension pneumothorax Tension Pneumothorax Incidence Penetrating Trauma Blunt Trauma Morbidity/Mortality Severe hypoventilation Immediate life-threat if not managed early Tension Pneumothorax Pathophysiology One-way valve forms in lung or chest wall Air enters pleural space, but cannot leave Pressure collapses lung on affected side Mediastinal shift to contralateral side Reduction in cardiac output Increased intrathoracic pressure deformed vena cava reducing preload Tension Pneumothorax Severe dyspnea extreme resp distress Restlessness, anxiety, agitation Decreased/absent breath sounds Worsening or Severe Shock Cardiovascular collapse Tachycardia Weak pulse Hypotension Narrow pulse pressure Tension Pneumothorax Jugular Vein Distension absent if also hypovolemic Hyperresonance to percussion Subcutaneous emphysema Late Tracheal shift away from injured side Cyanosis Tension Pneumothorax Recognize & Manage early Establish airway Needle thoracostomy then chest tube Tension Pneumothorax Decompress with 14g (lg bore), 2-inch needle Midclavicular line: 2nd intercostal space Midaxillary line: 4-5th intercostal space Go over superior margin of rib to avoid blood vessels Be careful not to kink or bend needle or catheter If available, attach a one-way valve Hemothorax Most common result of major trauma to the chest wall Present in 70 - 80% of penetrating and major nonpenetrating trauma cases Associated with pneumothorax Rib fractures are frequent cause Hemothorax Each can hold up to 3000 cc of blood Life-threatening often requiring chest tube and/or surgery If assoc. with great vessel or cardiac injury 50% die immediately 25% live five to ten minutes 25% may live 30 minutes or longer Blood loss results in Hypovolemia Decreased ventilation of affected lung Hemothorax Accumulation of blood in pleural space penetrating or blunt lung injury chest wall vessels intercostal vessels myocardium Massive hemothorax indicates great vessel or cardiac injury Intercostal artery can bleed 50 cc/min Hemothorax Chest tube, go to OR if 1000 cc out on insertion 200 cc/h for 4 hours Pulmonary Contusion Pathophysiology Blunt trauma to the chest Rapid deceleration forces cause lung to strike chest wall high energy shock wave from explosion high velocity missile wound low velocity as with ice pick Most common injury from blunt thoracic trauma 30-75% of blunt trauma mortality 14-20% Pulmonary Contusion Pathophysiology Rib Fx in many but not all cases Alveolar rupture with hemorrhage and edema increased capillary membrane permeability Large vascular shunts develop Gas exchange disturbances Hypoxemia Hypercarbia Pulmonary Contusion Assessment Findings Evidence of blunt chest trauma Cough and/or Hemoptysis Apprehension Cyanosis CXR changes late Pulmonary Contusion Management Supportive therapy Early use of positive pressure ventilation reduces ventilator therapy duration Avoid aggressive crystalloid infusion Severe cases may require ventilator therapy Myocardial Contusion Most common blunt injury to heart Usually due to steering wheel Significant cause of morbidity and mortality in the blunt trauma patient Myocardial Contusion Pathophysiology Behaves like acute MI Hemorrhage with edema Hemopericardium may occur from lacerated epicardium Cellular injury vascular damage may occur May produce arrhythmias hypotension unresponsive to fluid or drug therapy Myocardial Contusion Cardiac arrhythmias following blunt chest trauma Angina-like pain unresponsive to nitroglycerin Precordial discomfort independent of respiratory movement Pericardial friction rub (late) Myocardial Contusion ECG Changes Persistent tachycardia ST elevation, T wave inversion RBBB Atrial flutter, Atrial fibrillation PVCs PACs Myocardial Contusion IV LR/NS ECG Cautious fluid administration due to injured myocardium Standard drug therapy for arrhythmias 12 Lead ECG if time permits Admit to monitored evironment Pericardial Tamponade Incidence Usually associated with penetrating trauma Rare in blunt trauma Occurs in < 2% of chest trauma GSW wounds have higher mortality than stab wounds Lower mortality rate if isolated tamponade Tamponade is hard to diagnose Hypotension is common in chest trauma Heart sounds are difficult to hear Bulging neck veins may be absent if hypovolemia is present High index of suspicion is required Pericardial Tamponade Pathophysiology Space normally filled with 30-50 ml of strawcolored fluid lubrication lymphatic discharge immunologic protection for the heart Rapid accumulation of blood in the inelastic pericardium Pericardial Tamponade Pathophysiology Heart is compressed decreasing blood entering heart Myocardial perfusion decreased due to Decreased diastolic expansion and filling Hindered venous return (preload) pressure effects on walls of heart decreased diastolic pressures Removal of as little as 20 ml of blood may drastically improve cardiac output Pericardial Tamponade Beck’s Triad Resistant hypotension Increased central venous pressure distended neck/arm veins in presence of decreased arterial BP Small quiet heart decreased heart sounds Pericardial Tamponade Signs and Symptoms Narrowing pulse pressure Pulsus paradoxicus Radial pulse becomes weak or disappears when patient inhales Increased intrathoracic pressure on inhalation causes blood to be trapped in lungs temporarily Pericardial Tamponade Management ECHO if stable to diagnose In ER – consider pericardiocentesis Pericardial window followed by sternotomy in OR Traumatic Aortic Dissection/Rupture Caused By: Motor Vehicle Collisions Falls from heights Crushing chest trauma Animal Kicks Blunt chest trauma 15% of all blunt trauma deaths Traumatic Aortic Dissection/Rupture 1 of 6 persons dying in MVC’s has aortic rupture 85% die instantaneously 10-15% survive to hospital 1/3 die within six hours 1/3 die within 24 hours 1/3 survive 3 days or longer Must have high index of suspicion Traumatic Aortic Dissection/Rupture Separation of the aortic intima and media Blood enters media through a small intima tear Tear 2° high speed deceleration at points of relative fixation Thinned layer may rupture Descending aorta at the isthmus distal to left subclavian artery most common site of rupture ligamentum arteriosom Traumatic Aortic Dissection/Rupture Assessment Findings Retrosternal or interscapular pain Pain in lower back or one leg Respiratory distress Asymmetrical arm BPs Upper extremity hypertension with Decreased femoral pulses, OR Absent femoral pulses Dysphagia CXR Work up CTA Angio is rarely used Address other injuries first Ideally, repaire when stable Stent vs open Diaphragmatic Penetration Suspect intra-abdominal trauma with any injury below 4th ICS Suspect intrathoracic trauma with any abdominal injury above umbilicus Diaphragmatic Rupture Usually due to blunt trauma but may occur with penetrating trauma Usually life-threatening Likely to be associated with other severe injuries Diaphragmatic Rupture Pathophysiology Compression to abdomen resulting in increased intra-abdominal pressure abdominal contents rupture through diaphragm into chest bowel obstruction and strangulation restriction of lung expansion mediastinal shift 90% occur on left side due to protection of right side by liver Diaphragmatic Rupture Assessment Findings Decreased breath sounds Usually unilateral Dullness to percussion Dyspnea or Respiratory Distress Scaphoid Abdomen Usually impossible to hear bowel sounds Management suspect NG tube CT Laparoscopy Sensitive and specific Esophageal Injury Penetrating Injury most frequent cause Rare in blunt trauma Can perforate spontaneously violent emesis carcinoma Esophageal Injury Assessment Findings Pain, local tenderness Hoarseness, Dysphagia, Respiratory distress Mediastinal esophageal perforation mediastinal emphysema / mediastinal crunch SQ Emphysema Shock Abx resuscitation Early diagnosis Gastrographin -> dilute Ba Repair vs exclude Tracheobronchial Rupture Uncommon injury less than 3% of chest trauma Occurs with penetrating or blunt chest trauma High mortality rate (>30%) Respiratory Distress Obvious SQ emphysema Hemoptysis Especially of bright red blood Signs of tension pneumothorax unresponsive to needle decompression Tracheobronchial Rupture Majority (80%) occur at or near carina rapid movement of air into pleural space Tension pneumothorax refractory to needle decompression Consider early intubation intubating right or left mainstem may be life saving If arrest and suspect air embolysm, may have to do ERT… Damage control Damage control principle… ED Thoractomy Thoracotomy performed in ER for resuscitation of patients arriving in extremis Plan to take to OR afterwards AIM: Expeditious control of hemorrhage Maximization of coronary and cerebral perfusion Release of pericardial tamponade Tx of massive air-embolysm Procedure – Left Anterolateral Thoracotomy Clamshell Thoracotomy Release Pericardial Tamponade Control Intrathoracic Hemorrhage Eliminate massive air embolism or bronchopleural fistula Post intubation & positive pressure ventilation Get air transfer across traumatic alveolovenous channels Pulmonary hilar cross clamping Air aspirated from L ventricular apex and aortic root Cardiac massage Perform Open Cardiac Massage Bimanual internal massage with hands in a hinged clapping motion Ventricular compression proceeding from apex to base of heart Occlude Descending Thoracic Aorta Futile? Overall survival ~4-5% Little to Lose risk to Health care workers Risk blood contact 26% trauma pts HIV+ or Hepatitis+ Health care costs J Trauma. 1998 Jul;45(1):87-94 Selective Application of ED Thoracotomy Mechanism of Injury Presence of Vital Signs Location of Injury Other Signs of Life Survival based on mechanism J Trauma. 1998 Jul;45(1):87-94 Presence of vital signs J Trauma. 1998 Jul;45(1):87-94 Survival based on organ injured JACS 2000 Mar;190(3):288-98. Other Signs of Life (SOL) JACS 2000 Mar;190(3):288-98. What about PEA? 26/62 (42%) ED Thoracotomy survivors had PEA requiring CPR JACS 199:211-215, 2004 Conclusions ER thoracotomy considered in pts w/: Presence of vital signs in field or hospital Better results in penetrating cardiac injury Results w/ Blunt trauma poor, but survivors exist PEA after penetrating trauma from stabs Up to 70% good outcomes Contraindicated in pts with: No vital signs, prolonged asystole and unwitnessed arrest/loss of SOL JACS 199:211-215, 2004 Finally… PEA after blunt trauma? Typically poor outcome, but occasionally will have a survivor If CPR > 5 min, contraindicated References and thanks Thank God for internet and Google several websites specifically: http://www.adhb.govt.nz/trauma/presentations/Forums/major%20chest%20inj uries/sld001.htm http://www.templejc.edu/dept/ems/Pages/PowerPoint.html http://www.mssurg.net www.nordictraumarad.com/Syllabus06/mo%2015/NORDTERpenetrating.pdf www.iformix.com/spu/chest_trauma.ppt Greenfield textbook of surgery