Title of Presentation: Precepting Nurse Practitioner Students: Joys
advertisement

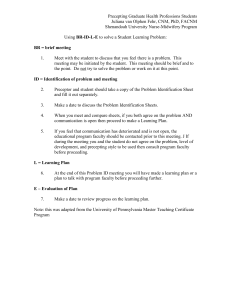
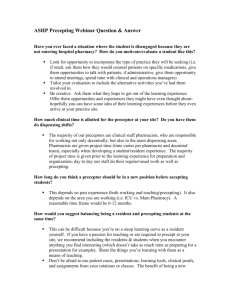
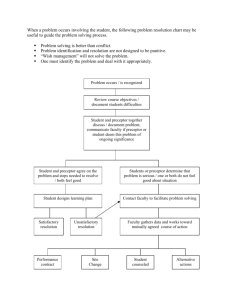
PRECEPTING NURSE PRACTITIONER STUDENTS: JOYS AND PITFALLS Eileen R. Giardino, RN, PhD, ANP-BC, FNP-BC Associate Professor UT Health - Houston – School of Nursing Houston, TX Program Objectives: The participant will: • Learn ways to improve the precepting experience • Improve evaluation of NP student performance • Understand legal aspects of the preceptor role • Relate NP study findings of expectations of NP preceptors to clinical practice The value of preceptors Preceptors: • Are valuable resource to every NP program • Are essential to strength & viability of NP programs • Teach students essential clinical skills • Evaluate student competence & performance • Serve as professional role models & socialization experts • Help students learn how to function in “real world” • Have both positive and negative qualities! (Ulrich, 2011) Why Be A Preceptor • Part of the professional role • Teaching/evaluating is part of what we do as NPs (Ulrich, 2011) • Satisfaction of “giving back” (Lyon and Peach, 2001) • Essential part of process for NP students to learn their profession (Burns, et al, 2006, Barker and Pittman 2010) • Students keep us “on our toes” (Suzewits, 2002) • Enhance quality of clinical practice • Contribute to professional development of SNPs. (Giardino & Giardino, 2013) • Preceptors enjoy teaching, want to develop the profession, support NPs in primary care (Giardino & Giardino, 2013) Preceptor Expectations Preceptor should expect: • To communicate with or have program faculty visit clinical site during semester • Support when needed from program faculty • Orientation to student/program curriculum • Know what students able/expected to do at practice site • Schools send students to site with little to no information about what student should do or is able to do at their site • CEU credit for precepting Precepting Rewards • Some programs pay stipends, most don’t (GNE Grant) • Some programs offer adjunct faculty appointment • Precepting keeps you sharp and current • Enhances professional reputation • Satisfaction in doing the “right thing” • Assures continuing excellence in NP profession NP program responsibilities • Understand what preceptors expect from students • Cultivate preceptors • Address preceptor needs & concerns that stem from • • • • student supervision. Have faculty available to address preceptor concerns Communicate with preceptor & site for any needed issues Respect that preceptor/site are graciously working with your students Students are ‘guests’ at the site Patient Expectations The patient should/must: • Agree that student may participate in visit • • Can inform patients at initial visit that practice educates clinicians Having a student is part of the practice philosophy • Know that visit might take additional time d/t student • Be seen by the provider as well Often patient impressed that provider is a teacher Study findings regarding precepting • Liability concerns • Conflicts between student’s educational needs and practice expectations to increase provider productivity [Lyon & Peach, 2001] • May face issues they are unaware of or unprepared for when precepting nurse practitioner students (Hayes, 1994) • Preceptors report greater self-confidence in rating students when they have had training in the precepting process (Aagaard, Teherani & Irby, 2004) Study Findings - Giardino & Giardino, 2013 • Preceptors felt students weak in generating & prioritizing diff diagnoses • Increase the focus on student generated differential diagnoses throughout the clinical experience • Many preceptors do not directly observe the SNPs conducting a physical examination. • Watch SNPs perform physical examination on patients at various times throughout the clinical experience • Opportunity to offer specific feedback around physical examination skills • Support SNP verbally presenting the patient case using a SOAP format • Preceptors work with students because • They enjoy teaching • Want to develop the profession • Support NPs in primary care • Important for NP program to support preceptors through • recognition of willingness to precept • Recognition of commitment to foster next generation of 10 care providers Logistics of Having Students in Practice • Space in practice for • extra exam room for student to see patient • talking with student privately • student to be when not seeing patients • Time factors – Precepting takes additional energy even when it doesn’t take much more time • Melding time it takes to precept into the productive schedule • Study in rural practice indicated that • parallel precepting strategy was 12 mins 24 sec per visit • & “regular” consultation (without precepting) was 13 mins, 27 sec • Walters, Worley, Prideaux & Lange, 2008 • Experienced preceptors take less time per visit with comparable outcomes (Baritt, 1997), (Vinson, 1997) • The more you precept, the better it gets from a time perspective Principles for Precepting Success • Different learners, different levels of experience, different techniques • Often we precept the way we were precepted • Not necessarily the best way to proceed • Remember what helped you the most to learn • The larger our repertoire of clinical teaching techniques, the more likely we are to help students be successful Techniques To Help Precepting • Determine student’s clinical goals. • Allow student opportunity to interact with patients • Choose appropriate patients for student • Request student to give a case presentation • Question student about case details • Allow student to give differentials and state a plan Feedback Techniques • Get a commitment • What do you think is going on? • Probe for supporting evidence • What led you to that conclusion? • Teach general rules • Many times when . . . • Reinforce what was right • ”You did an excellent job of . . . • Correct mistakes • Next time this happens, try this . . . • (Neher, Gordon, Meyer, Stevens, 1992) Principles of Evaluation • Difficult part of the process • Difficult to tell student that s/he not performing well • Be honest • Give specific examples of positive and negative situations • Should be constructive and based on skill development • Should be consistent for student’s level of practice • Should be respectful-focus on actions and preparation not personality • Can be day to day feedback or interval evaluation • Include assignments for further study or improvement • Should include communication to the faculty Dealing With Challenging Students • Patient safety is a primary concern • Trust your judgment - Go with your ‘gut’ • A failing student will often have limited insight or lack of personal awareness • Early communication of problems to student & faculty • Expect professional behaviors and professional dress • Articulate your expectations at outset of experience • Identify poor professional behavior or boundary breeches • Communicate expectations for change Dealing With Challenging Student • DOCUMENT, DOCMENT, DOCUMENT • Focus on behaviors rather than personality • Tell Faculty – Expect a site visit • Faculty should be supportive of your evaluation • Suggest strategies for reassignment if necessary Some Precepting Don’t’s Don’t: • precept a student when overcommitted & stressed • fail to review your students’ work • assume that student’s documentation is adequate or appropriate • put student down in front of the patient • hesitate to mention issues that are a source of annoyance or concern • From: Paulman, P.M. (2001) Family Medicine 33:10, 730-731 Legal or Liability Considerations • Site needs an affiliation agreement in place • Know what agreement states • See patients and review notes • Consider what skills student able to perform • Who is responsible if student gets needle stick or contracts HBV? Questions? Comments?