Ethics, equity and economics
advertisement

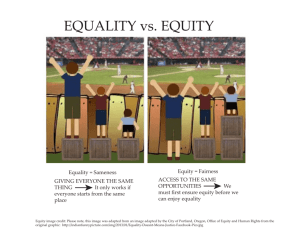
Ethics, equity and economics • Ethics - theories of “justice” - medical versus economic polarisation • Equity - definitions - “health”, “need” and “access vs. use” - micro versus macro • Economics - equity and efficiency Why ethics? • Philosophy determines objectives of health care system e.g. -maximise social well-being based on (consequentialist) utilitarianism • Different philosophical concepts have different implications, esp. for “efficiency” • Main practical manifestation = equity Categorising ethical theories (1) • Distributive justice - “political” or “social” philosophy - concerned with outcome • Procedural justice - “moral” philosophy concerned with process used in achieving the outcome Categorising ethical theories (2) • Political philosophy - societal focus e.g. Rawls • Moral philosophy - individual focus e.g Kantian Imperative • Interaction e.g. utilitarianism - social utility maximised by each individual maximising own utility Categorising ethical theories (3) Individual Process Outcome Society Entitlement Deontological Virtue Utilitarianism Rawlsian Egalitarian Rights Ethical theories • • • • • • • Utilitarianism Rawlsian Entitlement/libertarian Egalitarian Deontological? Virtue “Rights” Utilitarianism • Jeremy Bentham (classic) and John Stuart Mill (adapted) • ‘Maximising greatest ‘utility’ for greatest number’ • Underlies ‘efficiency’ • Issues - domain (whose utility) - malevolence (utility from suffering) Rawlsian ‘maximin’ • John Rawls 1971 • Allocation conducted under ‘veil of ignorance’ - leads to position of less well off in society being maximised • Issues - assumes total risk averseness - ‘bottomless pit’ argument Entitlement/libertarian • Robert Nozick 1974 • Individuals ‘entitled’ to what they have acquired ‘justly’ i.e. within a market situation • Stresses freedom of choice and property rights - minimal state involvement • Similar to utilitarianism Egalitarian • Equal shares in the distribution of a commodity • Issues - of what? health, services? - according to what criteria? ‘need’, age? Deontological (deon (Gk) = duty) • Immanuel Kant • Moral ‘rules’ of how to live which should not be broken (ie absolute moral code) • ‘Do to others as you would have done to you’ • Humans as end, not means Virtue theory • Not ‘what should I do’ but ‘what kind of person should I be’ • Similar to deontological - absolute moral ‘rules’ ‘Rights’ based theories • Unassailable ‘rights’ which cannot be overridden e.g.’right’ to life • Underlies ‘social contract’ theory • Absolute - inflexible ‘Medical’ vs. ‘economic’ ethic (1) • Medical - individual (deontological) ethic - Hippocratic oath, Nightingale Pledge - ‘Agency and professional codes conduct - ‘best interests’ of patient - opportunity cost ignored (?) ‘Medical’ vs. ‘economic’ ethic (2) • Economic - population based ethic - principally ‘utilitarian’ - based on opportunity cost • Overlap of considerations in both professions Medical dilemma (1) “I recall a patient who bled massively from his inoperable cancer of the stomach, I was the houseman and I had a strong sense that I must do my utmost for my patient, I ordered large quantities of blood to be cross matched and set up an infusion to replace the blood the patient had lost. It was not that I believed that the blood would cure him, but it would very probably save his life for a while longer, whereas without the blood transfusion he would have probably died there and then. A few days later the patient had another massive bleed and I again ordered more blood and set up a transfusion, again the patient survived what would almost certainly have been a fatal blood loss. The patient himself, knowing the situation, was keen to fight it as hard as possible.” Medical dilemma (2) After the second massive bleed and equally massive blood transfusion, my chief gently pointed out that there was no point in pouring in the blood as I had been, the patient had widespread cancer secondaries, his stomach was riddled with cancer and likely to bleed whenever the cancer eroded a blood vessel; blood transfusions could do no more than prolong the patient’s life by a very short time. If I went on ordering blood at the predigious rate I had been, I would literally break the bank, the blood bank, causing enormous expense whilst seriously jeopardising the chances of other patients for whom a blood transfusion could really be lifesaving, rather than merely death prolonging. Medical dilemma (3) I wanted to discuss all this with the patient, but he died the same day from a further massive bleed and that time I simply was not called. My superior had decided that there was nothing beneficial that could be done. More precisely, however, his analysis was surely based on a different assessment, notably that the benefit to the patient of repeated blood transfusions each time his stomach cancer bled, even if he himself wanted to fight to the last second, was insufficient to justify the enormous cost (to others) of providing the blood.” Tavistock Group - BMJ, Jan 23, 1999 • Prepare shared ‘code’ based on consistent moral framework - “healthcare is a human right…provide access…regardless of their ability to pay” - “care of individuals is at centre of health care but must be viewed within context of [generating] greatest possible health gains for groups and populations” Why equity? (1) • ‘Health’ = fundamental commodity (Sen) necessary for enjoyment of all else • Health care important determinant, but often expensive/unpredictable • Insurance = imperfect/expensive • Thus... Why equity? (2) • Healthcare should not be allocated/distributed according to income/wealth • Equity main reason government involvement in health care world-wide • Issues - concern with existing distribution income/wealth then why not change this directly? - trade off with efficiency? Why equity in health care? “ The social conscience is more offended by severe inequality in nutrition and basic shelter, or in access to medical care, than by the inequality in automobiles, books, furniture or boats” Tobin 1970 Equity not necessarily = equality • Equity concerned with ‘fairness' ‘justice’ (i.e.ethical theories) • May not necessarily entail equality. e.g.minimum standards of care, ‘postitive’ discrimination etc. • However, equity usually synonymous with equality of something. Equity: Vertical and/or horizontal? • Vertical - unequals treated unequally - applies especially to finance i.e. inequality in contribution by use (direct payments) or income (taxation) • Horizontal - equals treated equally - applies especially to delivery of health care e.g equal resources, utilisation, access per head. - most discussion refers to this. Ethics and equity • Mostly ‘horizontal’ equity in distribution of health(care) • Based on broad ‘egalitarian’ ethic, but compatible with most others • Basis = equal distribution of x (according to y) • Issues - what are x and y to be? ‘Definitions’ of equity (1) • • • • Equal ‘chance’ of treatment - lottery Equal expenditure per capita - geography. Equal resources per capita - geography. Equal expenditure/resources for equal ‘need’ (i.e. weighted for ‘premature’ mortality/morbidity e.g. RAWP) ‘Definitions’ of equity (2) (opportunity to use) • Equal access (opportunity to use) for equal need e.g equal waiting time per ‘condition’ • Equal utilisation (use) for equal need e.g. equal length of stay per ‘condition’ • Equal treatment for equal need • Equal ‘health’ ‘Access’ or ‘use’? • Access - maintain consumer sovereignty - unlikely to achieve equal ‘health’ • Use - closer to achieving equal ‘health’ - compromises consumer sovereignty Equal ‘health’? • Definition e.g. QALYS, LY’s? • Influence of non-health care factors e.g. housing, diet • Choice versus coercion e.g.smoking, diet • Implies reducing overall ‘health’ not ‘increasing’ - only truly equal state = dead • Maximising versus minimum standards Equity and ‘need’ (1) • ‘Need’ = ambiguous and confusing • Who determines need - producer - individual - ‘elite’ • Supply driven - what is available determines what is needed • Need versus ‘capacity to benefit’ - treat worse off even if health improvement less than treating better off Equity and ‘need’ (2) • ‘need’ versus ‘preference’ • ‘objective’ versus ‘subjective’ need • maximising - quantity of resources required to ensure individual becomes /maintained as healthy as possible = ‘bottomless pit’ • Minimising - standard of care which ensures individual not fall below ‘adequate’ level of health Equity and the NHS (1) “To provide the people of Great Britain, no matter where they may be, with the same level of service” (Bevan 1948) Equity and the NHS (2) “A fundamental purpose of a national service must be equality of provision so far as this can be achieved without an unacceptable sacrifice of standards”. (Merrson 1979) Report of the Royal Commission of the NHS Equity in practice • Historically concerned with geographical distribution of resources e.g. RAWP • In financing usually concerned with finance by taxation - represents ‘positive discrimination’ by income Measuring equity • Finance - Kakwai Index - Suits Index • Health - Gini coeff - see McGuire p.59 • Data - see Folland, Goodman & Stano book p.487 - see Donaldson & Gerard ‘Micro’ versus ‘macro’ equity • Micro - distribution between individuals e.g. GP. Individual ethic • Macro - distribution between groups e.g. regions. Group ethic • Useful to separate - not necessary for one ethic to apply across all levels Economics, equity and ethics • Common root = limited resources • Efficiency based on utilitarian ethic • Equity maybe based on a range of ethics • Does this lead to an inevitable conflict? Social welfare function UB 2 W 1 U W 0 W Umin 45 Umin U UA Utilitarianism encompasses all! (1) • Altruism = ‘caring externality’ - Sen (1977) concept of ‘sympathy’ - own utility enhanced by anothers well-being - fits within utilitarian philosophy • Altruism = ‘duty’ (Kantian imperative) - Titmuss (1970) - ‘duty’ give for benefit of others - constraint on utility maximisation (c.f. resource constraint) Utilitarianism encompasses all (2) • Participation altruism - utility gained from participation in social/collective acts regardless of utility from consumption which results • Outcome altruism - utility gained from utility derived by others in consuming what is ‘charitably’ provided Utilitarianism encompasses all! (3) • Generates possibility of 2, interdependent, utility functions for individual - as citizen and consumer • Diminishing marginal utility, and possibility of ‘free riding’, creates ‘rationale’ for coercion in achieving ‘citizen’ objectives Coming to a consensus? • Efficiency & equity common root scarcity • No universal agreed ethic for objectives of health care sector • But - ‘equality of access’ consistent with most ethical theories and consistent with efficiency (preserves consumer sovereignty)