Respiratory Power Point (T. Till)

Respiratory
Medications
Theresa Till Ed.D, RN,CCRN
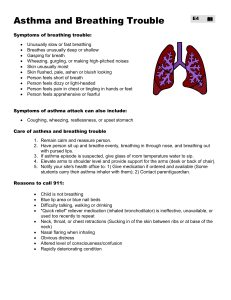
Pathophysiology of Asthma
HYPERRESPONSIVENESS OF AIRWAYS that results in:
Usually, reversible constriction of bronchial smooth muscle (bronchoconstriction).
Hypersecretion of mucus
Mucosal inflammation and edema
(Considered more a disease of inflammation than obstruction: obstruction occurs secondarily)
Triggers to Asthma
Asthma
(narrowed airways)
Asthma
Chronic Bronchitis
Usually caused by smoking or inhaled irritants.
“Mega” mucous
Airway inflammation
Irreversible
Emphysema
Alveolar Destruction
Emphysema
IRREVERSIBLE destruction of alveolar walls which decreases surface area for gas exchange.
Loss of lung elasticity: “springs” that hold open alveolar walls are “sprung” and collapse.
Air becomes trapped and distal airways hyperinflate and rupture.
Quit smoking
Major cause of
COPD.
Nicotine Patch
Medications that Treat
Respiratory Disease
Steroids
–REDUCE INFLAMMATION.
–CONSIDERED A DRUG OF
PREVENTION
–Not used acutely
–Best to use spacer (aerochamber) to decrease systemic effects.
–Rinse & spit after use.
–Commonly ends in “sone,” “olone”
Bronchodilators
Fast acting USED ACUTELY.
Open airways. Most bronchodilators are given via nebulizer, MDI or DPI.
Beta adrenergic agonists (erol, enol)
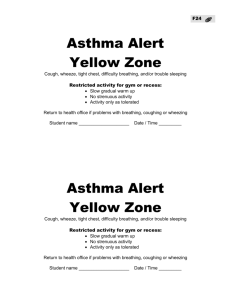
Common side effects are palpitations &, tachycardia. Note: If patients are using more than one canister a month
(200puffs), their disease is in poor control. Don’t use as “fire extinguisher.”
Ask why is fire breaking out?
Bronchodilators
Bronchodilators
(fast or slow acting) work by relaxing muscle walls and thereby making the air passage larger
.
Bronchodilators
– Methylxanthines: theophylline
Aminophylline second line drug given when extra treatment is needed. Given IV or PO.
Most common side effects of aminophylline are tachycardia, shakiness, and palpitations.
– Anticholinergics: relax bronchial smooth muscle but less effective than beta agonists.
– http://www.use-inhalers.com/
Respiratory Preventatives
Mast Cell Stabilizers
Not used acutely. Used to prevent an exacerbation of asthma.
Examples of mast cell stabilizers:
• Cromolyn (Intal)
• Nedocromil (Tilade)
• Inhibit histamine release from mast cells thus decreasing immune response.
Respiratory Preventatives
Leukotriene Modifiers
– Not used acutely. Used to prevent an exacerbation of asthma
– Leukotriene Modifiers: interfere with synthesis or block the action of leukotrienes which cause inflammation. Examples are:
• “lukast
• Montelukast (Singulair)
Valuable Miscellaneous
Interventions
Respiratory and Physical Therapy
Encourage to attend pulmonary rehabilitation classes (exercise supervised by professionals)
Breathing retraining (handout)
– Purse-lip
– Diaphragmatic (abdominal breathing)
Increase exercise tolerance
Effective coughing
– Flutter mucus clearance device
– Acapella- hand-held device that loosens secretions via vibrations & positive pressure
Teach patients to assess sputum
Avoid conversation with exercise
Metered Dose Inhalers
Common treatment.
Note location of
MDI when a spacer or aerochamber is not used.
Peak Flow Meters
Flutter Mucus Device
COPD
Abdominal
Breathing
Pursed Lip Breathing
http://www.bing.com/videos/search?q=t eaching+pursed+lip+breathing+animatio n&qs=n&form=QBVR&pq=teaching+pur sed+lip+breathing+animation&sc=0-
30&sp=-
1&sk=#view=detail&mid=76EC2961EE6
5A64565A976EC2961EE65A64565A9
Nutritional Therapy
Weight loss and malnutrition are common
• Pressure on diaphragm from a full stomach causes dyspnea
• Difficulty breathing while eating leads to inadequate consumption
• Drink fluids in between meals
• Rest at least 30 minutes prior to eating
• Frequent small meals (high calorie and protein)
• Prepare foods in advance
Respiratory Therapy
Aerosol nebulization therapy
–Deliver suspension of fine particles of liquid (medication) in a gas
–Easy to use
–Must be kept clean at home to prevent bacterial growth
Managing Oxygen Liter Flow
Outdated information: Never exceed 2 liters of oxygen per nasal cannula for patients with chronic lung disease because can knock out drive to breath.
This can occur but is rare.
New standard is to use oxygen saturation level as guide to how much oxygen to deliver. Increase oxygen level to maintain therapeutic oximetry. If
Sp02 ↓ with ↑ O2, stop.
Hinkle, MD, SIU Chief of
Pulmonary Medicine