Chapter 3
Chronic Obstructive
Pulmonary Disease
© 2007 McGraw-Hill Higher Education. All rights reserved.
Topics
•
•
•
•
•
Emphysema
Chronic Bronchitis
Pressure-volume curve
Dynamic airway compression
Ventilation-perfusion inequality
© 2007 McGraw-Hill Higher Education. All rights reserved.
Case Study #3: Chuck
• Used car salesman
• SOB over the last 3 years
– Chronic cough for 15 yrs
• Yellow, purulent
sputum
• 45 yr smoking history
• 2 packs a day
• Intermittent swelling of
the ankles
• Respiratory infection
history
• No family history of
lung disease
© 2007 McGraw-Hill Higher Education. All rights reserved.
Case Study #3: Chuck
•
•
•
•
•
Dyspneic
Florid appearance
Cyanotic
BP: 150/80
Barrel shaped
chest
• Ankle edema
• Whistling lung
sounds
© 2007 McGraw-Hill Higher Education. All rights reserved.
Chuck
• Hb: 17 g/dl
• X-ray
– Showed over inflation
• Ppa: 30 mmHg
• Vo2 max: 1.2 L/min
• Treatment
– Bed rest, oxygen
therapy, bronchodilators,
diuretics
– Advised to stop smoking
– COPD rehab program
© 2007 McGraw-Hill Higher Education. All rights reserved.
Chuck
• 6 mo later
– Admitted with acute
chest infection
– Marked dyspnea
– Purulent sputum
– Cyanosis
– Rales
– Obvious ankle
edema
– PaO2: 42 mmHg
– PaCO2: 55 mmHg
– pH 7.30
– died
© 2007 McGraw-Hill Higher Education. All rights reserved.
Chronic Bronchitis
• Autopsy
– Lungs voluminous and lacked elastic recoil, some bronchi
filled with mucus secretions, much destruction, with alveolar
destruction prominent
– Definite Chronic Bronchitis (blue bloaters) and emphysema
(pink puffers), which caused respiratory failure
© 2007 McGraw-Hill Higher Education. All rights reserved.
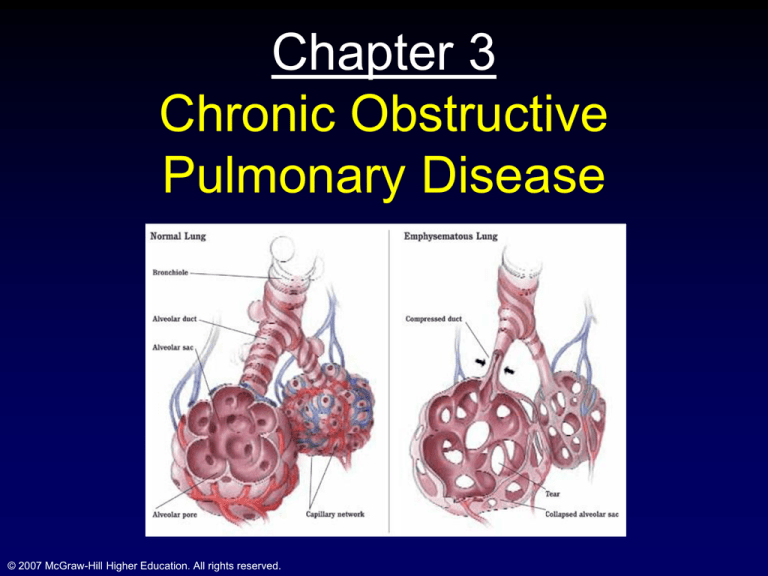
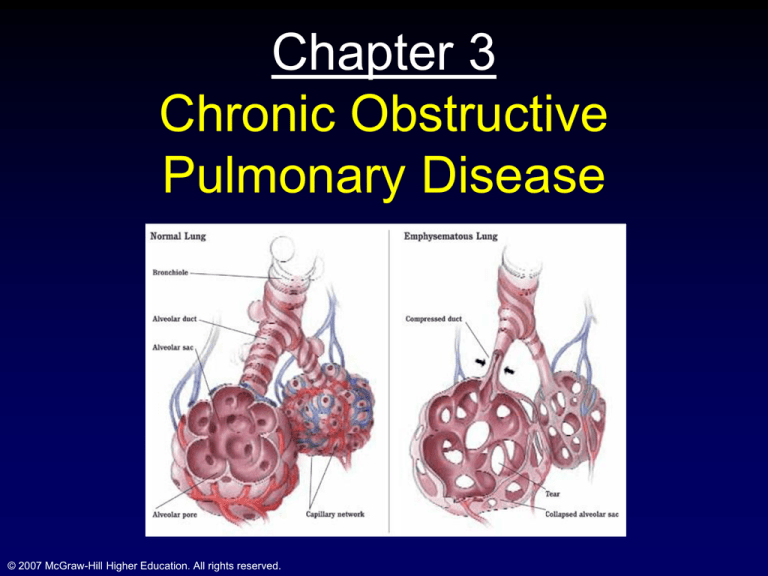
Pathology
• Structure
– Alveolar
destruction
– Enlarged
airspaces
– Emphysema:
– From the latin to
inflate
– Characterized by
enlargement of
the air spaces
distal to the
terminal
bronchioles w/
destruction of the
alveolar walls
© 2007 McGraw-Hill Higher Education. All rights reserved.
COPD and lung function
• Chronic bronchitis
– Marked by hypertrophied
mucus glands
– Inflammatory response due to
irritants in smoke
– Airways are swollen and
blocked by mucus
– Increased sputum production
© 2007 McGraw-Hill Higher Education. All rights reserved.
Physiology & pathophysiology
• Increasing SOB
– Thickened bronchial walls
– Obstruction
– Poorly supported airways
– Airway collapse
– Florid with central
cyanosis
• Elevated Hb
• Low SaO2
• Low Po2
–Release of EPO
© 2007 McGraw-Hill Higher Education. All rights reserved.
Physiology & pathophysiology
• Overinflation: inc. lung volume
• Whistling sounds caused by
increased turbulence
• Neck vein engorgement, ankle
edema and enlarged liver
consistent with pulm
hypertension
– Right axis deviation is
consistent with hypertrophy
of the RV
© 2007 McGraw-Hill Higher Education. All rights reserved.
Pulmonary function tests
© 2007 McGraw-Hill Higher Education. All rights reserved.
•
Pressure volume curve
Gives you the compliance curve
– Gives information about the elasticity of the lung
– Pleural pressure is the negative pressure created by
the outward pull of the ribcage and the inward pull of
the lung
– The lung will inflate as this pressure becomes more
negative
– Hysteresis
– Transpulmonary pressure: pressure differential
across the lung
• Diff betw intrapulmonary and intrapleural
pressures
© 2007 McGraw-Hill Higher Education. All rights reserved.
Compliance
• Volume change per unit pressure change (ΔV/ΔP)
• Lung very compliant in the middle of the curve; very
stiff on the ends
• Emphysema Increases the compliance and reduces
the elasticity of the lung
© 2007 McGraw-Hill Higher Education. All rights reserved.
Regional differences in Ventilation
• Uneven
– Higher in lower lung units, lowest in upper
• Posture dependent
• Laying supine
–Highest in posterior lung
© 2007 McGraw-Hill Higher Education. All rights reserved.
Regional differences in Ventilation
• Why?
• Intrapleural pressure
less negative at
base
– Due to the weight
of the lung
– Upper lobes are
already
somewhat
distended
– Lower lobes thus
fill more (larger
unit change in
volume)
© 2007 McGraw-Hill Higher Education. All rights reserved.
•At low lung volumes
Now intrapleural pressures are uniformly less
negative (lung is smaller); base is now being
compressed and ventilation is impossible; so apex
is now better ventilated; typically apex is better
ventilated
Airway closure
• Compressred regions do not have all the air
squeezed out
– Small airways close first
– Traps gas
– Usu. Occurs only at low lung volumes
– In aging the volume this occurs at rises; why?
• Dependent regions of the lung are poorly
ventilated
© 2007 McGraw-Hill Higher Education. All rights reserved.
Forced expiration
• Measured with spirometer
– FEV1.0
– FVC
– Measured after breath to TLC
– FEF25-75% Measure of elasticity of lung
© 2007 McGraw-Hill Higher Education. All rights reserved.
Dynamic compression
of Airways
• Descending limb is invariant because it is
“effort independent”
• What limits flow?
• Only at high volumes does increased
effort result in increased flow
© 2007 McGraw-Hill Higher Education. All rights reserved.
Dynamic airway compression
• Airways are compressed as
intrathoracic pressure increases
• A: opening pressure of 5 cmH2O
• B: Opening pressure of 6 cmH2O
• C: Opening pressure of 8
• D: Closing pressure of 11 cmH2O
• Thus, maximal flow decreases
with lung volume
• Lung volume changes here are
entirely due to elastic recoil
• Worse in emphysematous lungs
as elastic recoil is reduced
© 2007 McGraw-Hill Higher Education. All rights reserved.
Blood gases
• PaO2 declines somewhat
with age
• Cause:
– VA/Q mismatch
– Po2 is determined by the
ratio of ventilation to blood
flow
© 2007 McGraw-Hill Higher Education. All rights reserved.
Ventilation-perfusion
inequality
–
–
–
–
A: normal VA/Q
B: No ventilation; so VA/Q of 0
C: No blood flow: VA/Q of ∞
Note how VA/Q is different betw apex
and base of lung
© 2007 McGraw-Hill Higher Education. All rights reserved.
Ventilation-perfusion
• Areas with very
high VA/Q add very
little to oxygen to
blood; thus PaO2 is
dominated by areas
of low VA/Q
• Also shape of O2Hb dissociation
curve dictates that
areas of very high
VA/Q cannot
increase the
oxygenation of the
blood very much,
while areas of low
VA/Q can lower Po2
considerably
© 2007 McGraw-Hill Higher Education. All rights reserved.
•
Ventilationperfusion
Normal lung, A-aDO is
2
about 4 mmHg due to
VA/Q mismatching
• Disease can increase
this by quite a bit
• MIGET
– Inert gases with
range of solubilities
infused
intravenously
– Measure
concentrations in
arterial blood and
expired air
– No blood flow to
unventilated areas
(no shunt)
© 2007 McGraw-Hill Higher Education. All rights reserved.
Measurement of ventilationperfusion inequality
• Alveolar-arterial Po2 difference
– PAO2 = PIO2 – [PACO2/R]
– Chuck:
– 149-[49/0.8] = 88 mmHg
– PaO2 = 58
– AaDO2= 30
• PaCO2
– Chuck: 49 mmHg
• VA/Q mismatch
• Hypoventilation: Pco2 = [Vco2/VA]*K
• pH: falls due to elevated Pco2 (respiratory acidosis)
© 2007 McGraw-Hill Higher Education. All rights reserved.
Acclimatization and High-altitude
diseases
• Hyperventilation
– Hypoxemia stimulates peripheral chemoreceptors; blows off
Co2, raises PAO2
– PB 250 mmHg do calculation
– Renal compensation reduces HCO3• Polycythemia
– Increased Hct and [Hb]
– Increases O2 carrying capacity: draw eq.
– EPO form kidney
• Other features
– Rightward shift in O2-Hb dissociation curve (Leftward at
extreme altitude)
• Improves off-loading of O2 at the tissues
• Caused by ↑2,3 DPG at altitude
• Increased capillary-to-fiber volume ratio
– Muscle mass drops at altitude
© 2007 McGraw-Hill Higher Education. All rights reserved.
Acclimatization and High-altitude
diseases
• Acute mountain sickness
– Headache, dizziness, palpitations, insomnia, loss of appetite
and nausea
• Hypoxemia and resp. alkalosis
• Chronic mountain sickness
– Cyanosis, fatigue, severe hypoxemia, marked polycythemia
• High altitude pulmonary edema
– Severe dyspnea, orthopnea, cough, cyanosis, crackles and
pink, frothy sputum
– Life threatening
– Associated with elevated Ppa (hypoxic pulm
vasoconstriction)
• High altitude cerebral edema
– Confusion, ataxia, irrationality, hallucinations, loss of
consciousness and death
– Fluid leakage into brain
© 2007 McGraw-Hill Higher Education. All rights reserved.