Cardiovascular disease
advertisement

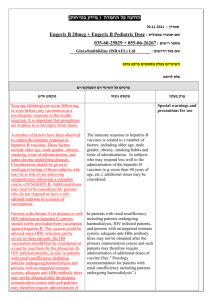
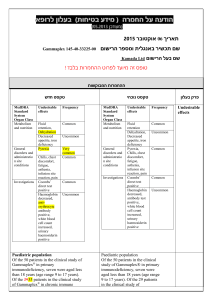
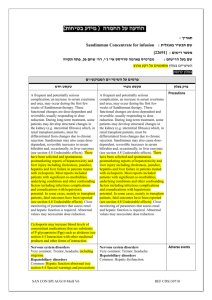
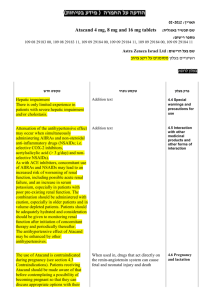
קבלה של חולה בכירורגיה יונתן אברהם דמה סיבת הפניה מחלה נוכחית הבעיה ,זמן תלונות נלוות :מעי ,שד... בדיקות לבירור :אנדוסקופיה ,קולונוסקופיה U/S, CT, ממוגרפיה.MRI , גורמי סיכון :סיפור משפחתי ,שד... רקע סוגי ניתוחים דחוף ( - )urgentמיידי או מוות. :Emergent יש לבצעו תוך 24שעות. אלקטיבי :יש זמן להכנת החולה. מג'ורי (קשים ,נרחבים וממושכים -השתלות כבד ,לבלב ,כריתות וכו'). רגיל (רוב הניתוחים). מינורי (למשל הסרת לזיות עוריות בהרדמה מקומית). רקע Age Nutritional Status Obesity Cardiovascular Cerebro-vascular Pulmonary Renal Hepatobiliary Endocrine Hematologic ASA Classification I—Normal healthy patient II—Patient with mild systemic disease III—Patient with severe systemic disease that limits activity but is not incapacitating IV—Patient who has incapacitating disease that is a constant threat to life V—Moribund patient not expected to survive 24 hours with or without an operation Significant independent predictor of mortality.[ Age Age has been reported as an independent risk factor for postoperative mortality. Predicting and preventing postoperative delirium Patients with three or more of the following have a 50% risk for postoperative delirium: 70 years or older; self-reported alcohol abuse; poor cognitive status; poor functional status; markedly abnormal preoperative serum sodium, potassium, or glucose level; noncardiac thoracic surgery; and aortic aneurysm surgery. Post operative delirium If delirium does occur, metabolic and infectious causes need to be investigated before labeling the event as sundowning. Nutritional Status Evaluation of the patient's nutritional status is part of the preoperative evaluation. A history of weight loss greater than 10% of body weight over a 6-month period or 5% over a month is significant. Degree of malnutrition temporal wasting, cachexia, poor dentition, ascites, peripheral edema Serum markers Albumin (half-life, 14-18 days), Transferrin (half-life, 7 days), Prealbumin (half-life, 3-5 days) TPN Patients with severe malnutrition appear to benefit most from preoperative parenteral nutrition. The majority of studies show a reduction in the rate of postoperative complications from approximately 40% to 30%. Obesity The perioperative mortality rate is significantly increased in patients with clinically severe obesity: body mass index [BMI] >40 kg/m2 or BMI >35 kg/m2 with significant comorbid conditions. Severe obesity Clinically severe obesity is associated with a higher frequency: essential hypertension pulmonary hypertension left ventricular hypertrophy congestive heart failure ischemic heart disease :לפי הספר Patients with no or one of these risk factors receive a β-blocker preoperatively for cardio-protection. Patients with two or more risk factors undergo noninvasive cardiac testing preoperatively. Obesity Obesity is also a risk factor for postoperative wound infection. The rate of wound infections is much lower with laparoscopic surgery in this group, which could have a bearing on selection of the operative approach. Obesity Obesity is an independent risk factor for DVT and PE. appropriate prophylaxis is instituted in these patients. CLEXAN Cardiovascular disease - leading cause of death in the industrialized world, - its contribution to perioperative mortality during noncardiac surgery is significant. Cardiovascular disease Of the 27 million patients undergoing surgery in the United States every year, 8 million, or nearly 30%, have significant coronary artery disease or other cardiac comorbid conditions. One million of these patients will experience perioperative cardiac complications, with substantial morbidity, mortality, and cost. Revised Cardiac Risk Index 1. Ischemic heart disease 1 2. Congestive heart failure 1 3. Cerebral vascular disease 1 4. High-risk surgery 1 5. Preoperative insulin treatment of diabetes 1 6. Preoperative creatinine >2 mg/dL 1 Each increment in points increases the risk for postoperative myocardial morbidity Revised Cardiac Risk Index סיכון לסיבוך קרדיאלי מאג'ורי 0 גורמי סיכון – 0.4% 1 גורמי סיכון 0.9% 2 גורמי סיכון 7% 3 ומעלה ג"ס – 11% Cardiac Tests 1. 2. 3. 4. 5. patient's functional capacity, which is estimated by obtaining a history of the patient's daily activities. 2 flight of stairs. Standard exercise stress test Echography Pharmacologic stress testing with dipyridamole Angiography IHD Patients who have undergone a percutaneous coronary intervention with stenting need to have elective noncardiac procedures delayed for 4 to 6 weeks. General recommendations are to wait 4 to 6 weeks after MI to perform elective surgery. IHD אנגינה יציבה – הקשר לסיבוכים לא ודאי – יש בכל זאת לבצע בירור. אנגינה לא יציבה (במנוחה או פעילות מינמלית) – רצוי לדחות ניתוחים אלקטיביים עד להמשך הבירור הלבבי. אוטם לאחרונה (ב 6חודשים אחרונים) – יש 11-16%סיכון לאוטם חוזר ב 3-6 חודשים אחרי הניתוח ,וגם נשאר גבוה אחרי 6חודשים 4-5%( .לעומת 0.1% באנשים ללא היסטוריה של .)MI B-Blokers Perioperative risk for cardiovascular morbidity and mortality was decreased by 67% and 55%, respectively, in ACC/AHA-defined medium- to highrisk patients receiving β-blockers in the perioperative period versus those receiving placebo. VHD ASמגביר סיכון פי .14 בכל אוושה מסוג –Ejectionנעשה Echoלפני ניתוח. יש לברר תלונות של קוצ"נ במאמץ ,כאב בחזה וסינקופה. בכל מחלה מסתמית (פרט ל MVPללא אוושה) יש צורך באנטיביוטיקה כמניעה לאנדוקרדיטיס בפרוצדורות. מחלה צרברו-וסקולרית שבץ סביב ניתוחי הוא סיבוך נדיר יחסית :פחות מ ,1%וכ 2-5% מחולי לב. מעל 80%מופיעים אחרי הניתוח – ולרוב קורים מירידה בל"ד ואמבוליות קרדיוגניות מפרפור פרוזדורים. המתח הניתוחי החריף עלול לגרום לסימנים פוקאליים של שבץ קודם לחזור ולהופיע ולחקות כך איסכמיה חריפה. מחלה צרברו-וסקולרית גורמי סיכון: גיל, יתר ל"ד, מחלת לב קורונרית, סכרת אישון. אוושה אסימפטומטת בקרוטיד יחסית שכיחה -קורה ב 14%מהמנותחים מעל גיל .55 בפחות מ % 50זה משקף בעיה המודינמית משמעותית. לא הודגמה עלייה בסיכון לשבץ בניתוחים שאינם בלב – אך סביר לעשות דופלר קרוטידים בחולים אלו לפני פרוצדורות ניתוחיות משמעותיות. חולים עם TIAלאחרונה בסיכון מוגבר לשבץ ולכן צריכים לעבור הערכה נוירולוגית לפני ניתוח: CT ראש, אקו, דופלר קרוטידים. אם אצלם ידועה הצרות סימפטומטית בקרוטיד – הם יצטרכו לעבור Endarterectomyלפני ניתוח אלקטיבי כללי. שבץ לאחרונה יש לדחות את ניתוח אלקטיבי לפחות ב 6שבועות. Pulmonary Consider assessment of pulmonary function: all lung resection cases, thoracic procedures requiring single-lung ventilation, major abdominal and thoracic cases in patients who are older than 60 years, have significant underlying medical disease, smoke, pulmonary symptomatology. pulmonary complication pneumonia respiratory failure Need of tracheostomy Adults with an FEV1 of less than 0.8 L/sec, or 30% of predicted, have a high risk for complications and postoperative pulmonary insufficiency. Risk factor of pulmonary complications age, dependent functional status, weight loss, lower albumin level, Obesity, Obstructive sleep apnea previous stroke, congestive heart failure, renal failure, chronic obstructive pulmonary disease, smoking, preoperative sputum production, pneumonia, dyspnea, chronic steroid use, blood transfusion Preoperative interventionS smoking cessation (>2 months before the planned procedure), bronchodilator therapy, antibiotic therapy for preexisting infection, pretreatment of asthmatic patients with steroids. Perioperative strategies epidural anesthesia, vigorous pulmonary toilet and rehabilitation, bronchodilator therapy. Aerovent, Ventolin Renal Approximately 5% of the adult population have some degree of renal dysfunction and cause additional morbidity in the perioperative period. a preoperative creatinine level of 2.0 mg/dL or higher is an independent risk factor for cardiac complications. Renal history and physical examination: particular questioning about previous MI and symptoms consistent with ischemic heart disease. The cardiovascular examination seeks signs of fluid overload. Anemia in CRF Anemia may range from mild and asymptomatic to that associated with fatigue, low exercise tolerance, and exertional angina. Such anemia can be treated with erythropoietin preoperatively or perioperatively. Thrombocytopathy Because the platelet dysfunction associated with uremia is often a qualitative one, platelet counts are usually normal. Dialysis Patients with chronic end-stage renal disease undergo dialysis before surgery to optimize their volume status and control the potassium level. Prevention of secondary renal insults avoidance of nephrotoxic agents maintenance of adequate intravascular volume nonsteroidal agents are avoided Hepatobiliary A history of any exposure to blood and blood products or exposure to hepatotoxic agents. Patients need to be questioned about when the diagnosis was made and what activity led to the infection. it is important to obtain this information in case an operative team member is injured during the planned surgical procedure. Symptoms pruritus, fatigability, excessive bleeding, abdominal distention, weight gain. Evidence of hepatic dysfunction on physical examination Jaundice and scleral icterus may be evident with serum bilirubin levels higher than 3 mg/dL. spider angiomas, caput medusae, palmar erythema, clubbing ascites: Abdominal distention, evidence of fluid shift Encephalopathy Asterixis Muscle wasting or cachexia liver function tests hepatocellular enzymes: acute or chronic hepatitis. HAV, HBV, HCV Alcoholic hepatitis (AST/ALT greater than 2). hepatic synthetic function: serum albumin, prothrombin, and fibrinogen. Child-Pugh Scoring System POINTS 1 2 3 Encephalopathy None Stage I or II Stage III or IV Ascites Absent Slight (controlled with diuretics) Moderate despite diuretic treatment Bilirubin (mg/dL) <2 2-3 >3 Albumin (g/L) >3.5 2.8-3.5 <2.8 PT (prolonged seconds) <4 4-6 >6 INR <1.7 1.7-2.3 >2.3 Class A = 5-6 points; Class B = 7-9 points; Class C = 1015 points. initially applied to predict mortality in cirrhotic patients undergoing portacaval shunt procedures, it has been shown to correlate with mortality in cirrhotic patients undergoing a wider spectrum of procedures. Mortality rate Child A-10%, B-31%, and C-76% during abdominal operations. Endocrine diabetes mellitus, hyperthyroidism or hypothyroidism, adrenal insufficiency Diabetes Mellitus Presence of diabetic complications: cardiac disease, circulatory abnormalities, retinopathy, neuropathy, nephropathy. Preoperative testing fasting and postprandial glucose hemoglobin A1c levels Serum electrolyte blood urea nitrogen, and creatinine levels Urinalysis: proteinuria. Neuropathy The existence of neuropathy in diabetics may be accompanied by cardiac autonomic neuropathy, which increases the risk for cardiorespiratory instability in the perioperative period. DM Treatment The adequacy of perioperative glycemic control has an impact on wound healing and the risk for surgical site infection. Discontinue: long-acting sulfonylureas such as chlorpropamide and glyburide because of the risk for hypoglycemia; metformin because of its association with lacticacidosis in the setting of renal insufficiency. Treatment a shorter-acting agent or sliding-scale insulin coverage Frequent assessments of glucose levels are continued through the postoperative period maintain the perioperative glucose level between 80 and 150 mg/dL. Postoperative cardiac events can occur with unusual manifestations in these patients. Although chest pain needs to be evaluated with ECG and serum troponin levels, this same evaluation may need to be done for new-onset dyspnea, blood pressure alterations, or a decrease in urine output. Thyroid disease Hyperthroidism Evidence of hyperthyroidism is addressed preoperatively and surgery deferred until a euthyroid state is achieved. antithyroid medication such as propylthiouracil or methimazole is gived β-blockers or digoxin are also continued Hypothyroidism Hypothyroidism generally do not require preoperative treatment. Severe hypothyroidism Severe hypothyroidism can be associated with: myocardial dysfunction, coagulation abnormality, electrolyte imbalance, hypoglycemia. Severe hypothyroidism needs to be corrected before elective operations. Steroid use A patient with a history of steroid use may require supplementation for a presumed abnormal adrenal response to perioperative stress. Steroid use Patients who have taken more than 5 mg of prednisone (or equivalent) per day for more than 3 weeks within the past year are considered at risk when undergoing major surgery. Lower doses of steroid or minor procedures are not generally associated with adrenal suppression. Steroid use Minor operations such as hernia repair under local anesthesia may not require any additional steroid The adequacy of the hypothalamic-pituitary response to adrenocorticotropic hormone (ACTH) can be tested in any patient who may have some degree of suppression secondary to chronic or intermittent steroid use: low-dose ACTH stimulation test Steroid use Moderate operations such as open cholecystectomy or lower extremity revascularization: 50 to 75 mg/day of hydrocortisone equivalent for 1 or 2 days. Major operations such as colectomy or cardiac surgery are covered with 100 to 150 mg/day of hydrocortisone equivalent for 2 to 3 days. Hematologic anemia, inherited or acquired coagulopathy, hypercoagulable state. Anemia evaluation CBC, reticulocyte count, serum iron, total iron-binding capacity, ferritin, vitamin B12, folate Blood transfusion patients with normovolemic anemia without significant cardiac risk or anticipated blood loss can be managed safely without transfusion. most healthy patients tolerating hemoglobin levels of 6 or 7 g/dL. Coagulopathy Coagulopathy may result from inherited or acquired platelet or factor disorders or may be associated with organ dysfunction or medications personal or family history of abnormal bleeding. history of liver or kidney dysfunction or recent common bile duct obstruction use of anticoagulants, salicylates, nonsteroidal antiinflammatory drugs (NSAIDs), and antiplatelet drugs are noted. Physical examination may reveal bruising, petechiae, or signs of liver dysfunction. Platelets qualitative or quantitative defects as a result of immune-related disease, infection, drugs, or liver or kidney dysfunction. Qualitative defects may respond to medical management of the underlying disease process, quantitative defects may require platelet transfusion when counts are less than 50,000 in a patient at risk for bleeding. anticoagulation therapy anticoagulation therapy usually require preoperative reversal of the anticoagulant effect. FFP, VIT K In patients taking warfarin, the drug is withheld for four scheduled doses preoperatively to allow the international normalized ratio (INR) to fall to the range of 1.5 or less (assuming that the patient is maintained at an INR of 2.0-3.0). Patients with a recent history of venous thromboembolism or acute arterial embolism frequently require perioperative IV heparinization because of an increased risk for recurrent events in the perioperative period. Patients taking anticoagulants for less than 2 weeks for pulmonary embolism (PE) or proximal DVT are considered for inferior vena cava filter placement before surgery. risk for venous thromboembolism Patients are questioned to elicit any personal or family history suggestive of a hypercoagulable state. Ex: aborption Levels of protein C, protein S, antithrombin III, and antiphospholipid antibody can be obtained. Risk factor stratification age, type of surgical procedure (hip or knee arthroplasty, hip fracture surgery; major trauma; spinal cord injury), previous thromboembolism, cancer, obesity, varicose veins, cardiac dysfunction, indwelling central venous catheters, inflammatory bowel disease, nephrotic syndrome, pregnancy, estrogen or tamoxifen use. בדיקות ספירה – אובדן דם משמעותי ,מחלה כרונית אלקטרוליטים BUN ,ו קראטינין – בגיל מעל ,60שימוש בדיורטיקה ,שלשול כרוני ,מחלת כליה ,מחלת כבד ,סכרת. שתן – בסימפטומים אורולוגיים ,אם יש קטטר ,באפשרות של פרוטזות בניתוח - PTT ,INRאם יש הסטוריה של דימומים במשפחה או בחולה ,שימוש בא"ק, מחלת כבד. ביוכימיה ותפקודי כבד – במחלת כבד/דרכי מרה. בדיקת הריון – כל אישה בגיל הפוריות (אלא אם אחרי כריתת רחם) גזים בדם :אם בסכנה לכשל נשימתי צילום חזה PA :וצדדי – כשיש סיכון מוגבר לסיבוכים ריאתיים ,פרוצדורות בלב/חזה -אלא אם צעיר מגיל 35או ידוע על אבנורמליות ב 6חודשים האחרונים. אקג –בגברים מעל ,40נשים מעל 50או אם יש בעיה קרדיו-וסקולרית ,אריתמיה או סכרת. רכיבי דם: סוג והצלבה – בסיכון גבוה לדימום הזמנת מנות דם לגבי בדיקות להפעיל שיקול דעת לגבי רקע