Accidental Hypothermia - Calgary Emergency Medicine
advertisement
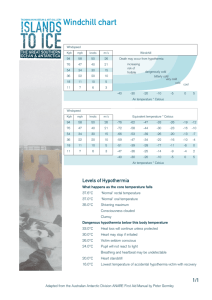
Accidental Hypothermia Grand Rounds Oct 15, 2009 Garth Smith CCFP-EM A case • 68 yo F, hx of dementia • missing for 7 hours • found by EMS in drainage ditch, comatose A case • • • • • • RR 6, pulse not palp, BP, T, Osat unmeasurable Glu 5.2 ECG - junctional bradycardia 30-40 bpm decor posturing, GCS 5, no signs trauma, pupils dilated/NR, foley temp 22.7C How to proceed? • • • airway - is it safe to intubate a profoundly hypothermic patient? what about that irritable mycocardium? breathing - what rate? Osat not registering so now what? how do I interpret ABG? what if I can’t get an ABG? circulation - choose your ACLS algorithm PEA vs unstable bradycardia vs hypothermia. dry or wet? afterdrop? CBP? Objectives • • • • • • • • • educate and entertain a case review definitions and physiology common investigation pitfalls or surprises ACLS / AHA guidelines and algorithm, Calgary protocol treatment modalities including some “new” ones hypothermia zingers what to expect in the near future questions • • • • • • accidental hypothermia approx 100 deaths per year (Stats Can) overall mortality ~15%. In mod/severe ~40%-80% (depends on underlying disease) hospital records “tip of the iceberg” mortality similar between men and women men are hypothermic more often (stupid) extremes of age at greater risk accidental hypothermia • majority of AH patients were drunk, using sedatives, outdoor exposure, and male Danzl D, Pozos R, Auerbach P, et al. Multicenter hypothermia survey. Ann Emerg Med 1987;16:1042-1055 Bizek G. Characteristics and Rates of Rewarming of Emergency Department Patients with Moderate to Severe Accidental Hypothermia. Annals of Emerg Med. 2008; 52:4 Definitions • • • • AH - unintentional decline in core temp <35C therapeutic - intentional, preserve brain & other organs. CPB, TBI, post Vfib arrest primary AH - exposure of healthy person to cold, thermoregulation overwhelmed secondary AH - disease state interferes with thermoregulatory process. includes trauma. Definitions Most Lit ACLS Trauma Mild 32 - 35 34 - 36 34 - 36 Mod 28 - 32 30 - 34 32 - 34 severe 20 - 28 <30 <32 profound < 20 Heat Transfer • test Heat Transfer • victims of AH are exposed to convection (wind) and conduction (water, ground, ice) • conductivity of water is 30 x that of air Thermoregulation • test Production + Retention < Cold = Hypothermia • • • • • • • • • • • • The politically incorrect Bs babies baldies (geriatrics) bums (streetpersons, low socioeconomic) booze and benzos blood (low sugar / trauma) brain - CNS and PNS (chronic and acute) boneheads bananas/bonkers (phenothiazines, TCAs, Lithium, impaired adaptive behaviour) badness (sepsis, pancreatitis, MI) barfers (anorexia or general malnourishment) burns breakdowns (this is Western Canada after all) Physiology • how do you die from hypothermia? • multi organ failure secondary to prolonged cardio respiratory arrest Danzl and Pozos. Accidental hypothermia. NJEM. 1994;26, 331, 1756-1760 Testa. Accidental Hypothermia. From EMRAP Feb 2009 Excitation Adynamic (slowing down) Shut down Danzl and Pozos. Accidental hypothermia. NJEM. 1994;26, 331, 1756-1760 Testa. Accidental Hypothermia. From EMRAP Feb 2009 Coagulopathy Gardner. accidental hypothermia. emergency medicine reports. 2009;30 Jurkovich. Environmental Cold-induced Injury. Surgical Clinics of N.A. 87 (2007) 247-267 Vfib • Ventricular fibrillation is rare above a core temperature of 32 C • increasingly more likely at lower temperatures • literature has numerous hypotheses Danzl DF. Accidental hypothermia. In:Auerbach P, ed.Wilderness Medicine, 5th ed(Mosby) 2007Steinman, Cardiopulmonary resuscitation and hypothermia. Circulation. 1986; 74 Afterdrop • • • • not the same as rewarming shock AD is physiological response, ↓core T after rewarming or removal from cold stress two theories: circulatory, thermal gradient be aware, reevaluate often, expect ↓T, +/clinical deterioration, rewarm the core first Webb P. Afterdrop of body temperature during rewarming: an alternative explanation. J Appl Physiol 1986;60:385-39 Giesbrecht G. Prehospital treatment of hypothermia. Wilderness Environ Med. 1999;12:24–31.Vanggaard L, Eyolfson D, Xu X, Weseen G, Giesbrecht GG. Immersion of distal arms and legs in warm water (AVA rewarming) effectively rewarms hypothermic humans. Aviat Space Environ Med. 1999;70:1081–108 Danzl DF. Accidental hypothermia. In:Auerbach P, ed.Wilderness Medicine, 5th ed(Mosby) 2007 Cold diuresis • • • • • etiology multifactorial. suggested mechanisms: 1. inhibition of antidiuretic hormone (ADH) release, 2. decreased renal tubular function, 3. relative central hypervolemia caused by systemic vasoconstriction, 4. impaired autoregulation of the kidney Cold water immersion ↑ urinary output x 3.5 ETOH impressively increases the diuresis the rule in AH is that the patient is dry, give volume Danzl DF. Accidental hypothermia. In:Auerbach P, ed.Wilderness Medicine, 5th ed(Mosby) 2007 Coagulopathy • enzymatic nature of the activated clotting factors is depressed by cold • Thrombocytopenia • cannot be confirmed by laboratory studies performed at 37° C • Treatment is rewarming and not simply administration of clotting factors Jurkovich. Environmental Cold-induced Injury. Surgical Clinics of N.A. 87 (2007) 247-267 Danzl DF. Accidental hypothermia. In:Auerbach P, ed.Wilderness Medicine, 5th ed(Mosby) 2007 Investigations and their Pitfalls • appropriate include CBC, Lytes, Ur, Cr, Glu, INR/PTT, ECG, ABG, TSH, Lipase, LFTs, CXR, UA • the general rule is not to make any assumptions. extremely variable results. • Many of the tests can provide falsly reassuring data. CBC • underestimates blood loss because of normal hematocrit • normal WBC count does not rule out infection • normal platelet count does not infer they are functional Danzl DF. Accidental hypothermia. In:Auerbach P, ed.Wilderness Medicine, 5th ed(Mosby) 2007 Hypothermia in the sepsis syndrome and clinical outcome: the Methylprednisolone Severe Sepsis Study Group. Crit Care Med 1992;20:1395-1401 Lytes • must be continuously monitored • K is a tricky little devil • ↓temp can increase hyperkalemic cardiac toxicity • characteristic ECG changes maybe obscured Danzl DF. Accidental hypothermia. In:Auerbach P, ed.Wilderness Medicine, 5th ed(Mosby) 2007 Glu • must have bedside test immediately • can be high or low • all hypoglycemia should be treated • do not treat hyperglycemia unless it does not resolve with rewarming • recheck often during rewarming Gardner. accidental hypothermia. emergency medicine reports. 2009;30 ECG • First ↑PR, then ↑QRS, then ↑QTc • preshivering muscle tone can obscure P waves • Osborn J waves • below 32C, anything is possible Danzl DF. Accidental hypothermia. In:Auerbach P, ed.Wilderness Medicine, 5th ed(Mosby) 2007Aslam et al. Hypotehrmia: Evaluation, Electorcardiographic Manifestations, and Management. Am Jn of Med (2006) 119, 297 -301 ABG • do they need to be corrected to temp? • debate about astat vs ph-stat • uncorrected ABG provides the most useful information Delaney,K. Assessement of Acid Base Disturbances in Hypothermia and their physiologic consequences. Ann Emerg med. Jan 1989; 18: 72-82 Bradycardia? Hemodynamic Status? Circulation. 2005;112:IV-136-IV-138 back to our case • • • • • • patient was intubated and ventilated CPR was not performed external rewarming with forced air blanket warmed IV saline no pressors, no Abx, no defib, no atropine, no pacing pulses palpable 30 min post arrival in ED Circulation. 2005;112:IV-136-IV-138 • • • • • • ACLS / AHA guidelines do all pulseless patients require CPR? does defibrillation need to be withheld until >30C? do meds need to be withheld until >30C? what meds are most effective? does bradycardia need to be treated? should hemodynamic stability as opposed to temperature determine interventions? do all pulseless patients require CPR? • No, if the patient is in the ED • the presence of an organized cardiac electrical rhythm (anything but vfib or asystole) or U/S evidence of organized movement should be taken as a sign of life • CPR is contraindicated in this situation • concern is conversion to vfib by CPR Jurkovich. Environmental Cold-induced Injury. Surgical Clinics of N.A. 87 (2007) 247-267 does defibrillation need to be withheld until >30C? • • • • Some authors say NO some recommend repeated defibrillation after every 1C rise in core temperature the AHA is vague - recommends repeat defibrillation “as core temperature rises” No evidence was referenced for either set of recommendations Gardner. Accidental hypothermia. Emergency medicine reports. 2009;30 Schweitzer. Cold but Not Dead. Air medical Journal. 2008; 27:2 Hanania. Accidental Hypothermia. Critical Care Clinics. 1999;15:2 do meds need to be withheld until >30C? • • • • AHA indicates meds to be withheld as they may accumulate to “toxic levels” once >30C they can be administered “with increased intervals between doses” systematic review of animal models suggests otherwise case series suggest otherwise Wira. Anti-arrhythmic and vasopressor medications for the treatment of ventricular fibrillation in severe hypothermia: a systematic review of the literature. Resuscitation. 2008; 78, 21-29 Gardner. Accidental hypothermia. Emergency medicine reports. 2009;30 • • • • • What meds are effective? no quality studies in humans, only case reports bertyllium appeared to be effective but was removed from AHA guidelines in 2000 classically taught that vasoconstrictors are ineffective and may precipitate vfib aforementioned animal models and case reports suggest efficacy of epi and amio Procainamide may precipitate vfib Wira. Anti-arrhythmic and vasopressor medications for the treatment of ventricular fibrillation in severe hypothermia: a systematic review of the literature. Resuscitation. 2008; 78, 21-29 Gardner. Accidental hypothermia. Emergency medicine reports. 2009;30 does bradycardia need to be treated? • • • • • • • guidelines say that “profound bradycardia” requires CPR severe hypothermia results in 50% decrease in HR most experts agree - CPR should be withheld in the severely hypothermic patient with a pulse regardless of heart rate or blood pressure. Cardiac pacing is generally not required for bradyarrhythmias unless the bradycardia persists despite rewarming A recent hypothermic dog model study concluded transcutaneous pacing is safe and effective (improved cardiac index, decreased warming time) recent case report of 2 human patients successfully treated with transcutaneous pacing utility of pacing lies in its ability to augment BP and increase rewarming Danzl DF. Accidental hypothermia. In:Auerbach P, ed.Wilderness Medicine, 5th ed(Mosby) 2007 Ahmed F. Hypothermia: Evaluation, Electroradiographic Manifestations, and Management. Am Jn of Med. 2006; 119: 297-301 Ho J. Successful Transcu. Pacing in 2 Severely Hypothermic Patients. Annals of Emerg Med. should hemodynamic stability as opposed to temperature determine rewarming treatment? • absolutely* • stable hemodynamics - noninvasive • cardiac arrest - CPB, thorasic lavage otherwise • unstable hemodynamics - debatable * true evidence-based guidelines do not exist at this time. no controlled randomized trials comparing rewarming techniques Walpoth. Outcome of Survivors of Accidental Deep Hypothermia and circulatory arrest treated with extracorporeal blood warming. NJEM. 1997; 337:1500-5 Kronger. Important aspects in the treatment of severe accidental hypothermia: The Innsbruck Experience. Journal of neurosurgical anesthesiology. 1996; 8: 1, 83-87 Sultan N. Treatment of severe accidental hypothermia with intermittent hemodialysis. CJEM. 2009; 11(2) Roggla M.Wiener Klinische Wochenschrift. 114(8-9):315-20, 2002 May 15 Treatment Active External Passive External Active Internal (invasive, noninvasive) Extracorporeal Passive Active endovascular rewarming catheter Ahmed F. Hypothermia: Evaluation, Electroradiographic Manifestations, and Management. Am Jn of Med. 2006; 119: 297-301 Scary Not Scary Open Mediastinal Lavage Peritoneal Lavage IV infusions Intubations and warm air endovascular catheter Bair Hugger CRRT CAVR CPB Closed Thorasic Lavage Plaisier B. Thoracic lavage in accidental hypothermia with cardiac arrest - report of a case and review of the literature. Resuscitation. 2005; 66: 99-104 Moss JF. A model for the treatment of accidental severe hypothermia. J Trauma 1986;26:68-74 Otto RJ, Metzler MH. Rewarming from experimental hypothermia: comparison of heated aerosol inhalation, peritoneal lavage, and pleural lavage. Crit Care Med 1988;16:869-875 Hall KN, Syverud SA. Closed thoracic cavity lavage in the treatment of severe hypothermia in human beings. Ann Emerg Med 1990;19:204-206Iversen RJ, Atkin SH, Jaker MA, Quadrel MA, Tortella BJ, Odom JW. Successful CPR in a severely hypothermic patient using continuous thoracostomy lavage. Ann Emerg Med 1990;19:1335-1337 Handrigan M. Factors and methodology in achieving ideal delivery Temperatures for intravenous and lavage fluid in hypothermia. Am Jrn of Emerg Med. 1997; 15:4 Sheaff C. Safety of 65C intravenous fluid for the treatment of hypothermia. Am Jrn of Surg. 1996; 172 Danzl DF. Accidental Hypothermia. NEJM. 1994; 331: 1756-60 Gentilello LM. Practical approaches to hypothermia. Adv Trauma Crit Care. 1994; 9:39-79 Steele MT. Forced Air Speeds Rewarming in Accidental Hypothermia. Ann Emerg Med. 1996; 27:479-484 Kornberger E. Forced Air surface rewarming in patients with severe accidental hypothermia. Resuscitation. 1999; 41(2):105-11 Komatsu S. Severe Accidental Hypothermia successfully treated by rewarming strategy using CVVHD system. Journal of Trauma. 2007; 62: 775-776 Gentilello LM, Jurkovich GJ, Stark MS, et al. Is hypothermia in the victim of major trauma protective or harmful? A randomized, prospective study. Ann Surg 1997;226(4):439–47 Walpoth. Outcome of Survivors of Accidental Deep Hypothermia and circulatory arrest treated with extracorporeal blood warming. NJEM. 1997; 337:1500-5 Endovascular rewarming catheters • • • 2 recent case reports 1 small case series Temperature-adjusted sterile saline flows within the balloons and exchanges heat with the blood as it passes by. Endovascular rewarming catheters • • 5-lumen intravascular catheter balloons form a closed loop system in 2 of the catheter's lumen • remaining 3 lumens are available for infusion • inserted as per normal CVC • complications are similar to CVC • may be helpful in trauma patient Taylor E. Active intravascular rewarming for hypothermia associated with traumatic injury: early experience with a new technique. Bayl Univ Med Cent. 2008; 21 (2): 120-126 Ban LH. A novel intravascular rewarming method to treat severe hypothermia. Eur Jr of Emer Med. 2008; 15: 56-58 Laniewicz M. Rapid endovascular warming for profound hypothermia. Annals of Emer Med. 2008; 51:2 Hypothermia Zingers • • • • • • • • CPR in the field: yes or no? initiate rewarming in the field or transport cold? intubation: safe or not? NG/OG: safe or not? when should resuscitation be withheld in the ED / prognostic factors? when can resuscitation be stopped in the ED? what is the optimal rewarming rate? are adjunctive therapies required? CPR in the field: yes or no? • • • • • • human experimental evidence is absent regarding the frequency of converting bradycardia to ventricular fibrillation But even if CPR induces ventricular fibrillation, the fibrillation is being treated If spontaneous ventricular fibrillation occurs in the absence of CPR, the resultant anoxia is not being treated at all long pulse check: 60 - 180 seconds if pulse not present, give O2 by BVM pulse still not present, Do CPR in the field (infers no access to cardiac monitor or U/S) Steinman A. Cardiopulmonary resuscitation and hypothermia. Circulation. 1986; 74 Hypothermia Guidelines. Circulation. 2005;112:IV-136-IV-138 CPR in the field: yes or no? contraindications for CPR •non compressible chest •ice formation in airway •decapitation or other injury incompatible with life •unsafe conditions for rescuers •signs of life Gardner. accidental hypothermia. emergency medicine reports. 2009;30 initiate rewarming in the field or transport cold? • if in cardiac arrest, perform CPR and transport cold but perform passive rewarming (remove wet garments, horizontal position, etc) • if pulse present, start rewarming Giesbrecht G. Emergency treatment of hypothermia. Emergency Medicine. 2001; 13: 9-16 Walpoth. Outcome of Survivors of Accidental Deep Hypothermia and circulatory arrest treated with extracorporeal blood warming. NJEM. 1997; 337:1500-5 intubation: safe or not? • • same indications to intubate as in non hypothermic patient • • endotracheal intubation is appropriate in victims of cardiac arrest. • failure to oxygenate, failure to ventilate, decreased level of consciousness, expected clinical deterioration Tracheal intubation was performed without incident in 117 cases, of which 97 were less than or equal to 32.2 C ventilate at have normal rates Danzl D, Pozos R, Auerbach P, et al. Multicenter hypothermia survey. Ann Emerg Med 1987;16:1042-1055 Hypothermia Guidelines. Circulation. 2005;112:IV-136-IV-138 NG/OG: safe or not? • no consensus • “nasogastric tube placement should be avoided because these have been shown to precipitate ventricular fibrillation” • “a nasogastric tube may be placed to relieve gastric distention” Schweitzer. Cold but Not Dead. Air medical Journal. 2008; 27:2 Gardner. accidental hypothermia. emergency medicine reports. 2009;30 • • • • when should resuscitation be withheld in the ED / prognostic factors? unreliable: time submerged, age of patient, etoh/tox ingestion, number of hours CPR, initial temperature, physical exam asphyxia (sudden drowning, avalanche with no air pocket) hypothermic cardiac arrest, K> 9 mmol/L or a pH < 6.50 are not expected to survive K> 10 mmol/L during acute hypothermia appears to be a reliable marker of death be wary of anyone intubated with depolarizing neuromuscular blocker Schaller MD. HyperK, a prognostic factor during acute severe hypothermia. J Am Med Assoc 1990;264:1842-1845 Hauty MG. Prognostic factors in severe accidental hypothermia: experience from the Mt. Hood tragedy. J Trauma 1987;27:107-112 Kornberger M. Prognostic markers in patients with severe accidental hypothermia and cardiocirculatory arrest. Resuscitation1994; 27:47–54 when should resuscitation not be attempted in the ED / prognostic factors? • • • Regardless of the presentation, there are no validated prognostic indicators of the potential for recovery from acute severe hypothermia A decision to continue or terminate resuscitation cannot be based on laboratory parameters alone Survival often appears unpredictable and unrelated to treatment. Schaller MD. HyperK, a prognostic factor during acute severe hypothermia. J Am Med Assoc 1990;264:1842-1845 Hauty MG. Prognostic factors in severe accidental hypothermia: experience from the Mt. Hood tragedy. J Trauma 1987;27:107-112 Kornberger M. Prognostic markers in patients with severe accidental hypothermia and cardiocirculatory arrest. Resuscitation1994; 27:47–54 when can resuscitation be stopped in the ED? • • • the only definite criterion of death is failure to respond to resuscitation and rewarming most experts agree that refractory cardiac arrest above 32C is indicative of death the decision to terminate resuscitation must be individualized by the physician in charge and should be based on the unique circumstances of each incident Danzl DF. Accidental hypothermia. In:Auerbach P, ed.Wilderness Medicine, 5th ed(Mosby) 2007 Weinberg A. Hypothermia. Annals of Emerg Med. 1993; 22 • • • • • what is the optimal rewarming rate? rapid rewarming does not necessarily improve the chance of survival, except when cardiac arrest is present A rewarming rate of 1.85°C/hour can ↑ O2 extraction up to 60% →mismatch supply/demand a safe strategy would be to promote steady but moderate warming If perfusing cardiac output target of 1-2ºC per hour If cardiac arrest, then a faster rate of >2ºC per hour Komatsu S. Severe Accidental Hypothermia successfully treated by rewarming strategy using CVVHD system. Journal of Trauma. 2007; 62: 775-776 Giesbrecht G. Prehospital treatment of hypothermia. Wilderness and Environ Med. 2001; 12: 24-31 Davis PR, Byers M. Accidental Hypothermia. J R Army Med Corps 2006;152:223-33 are adjunctive therapies required? • empiric steroids, barbiturates, and antibiotics do not increase survival rates from hypothermia • recommendations for the use of empiric steriods, Abx, insulin, sodium bicarb are out of date and should not be routinely used Ahmed F. Hypothermia: Evaluation, Electroradiographic Manifestations, and Management. Am Jn of Med. 2006; 119: 297-301 Gardner. accidental hypothermia. emergency medicine reports. 2009;30 what to expect in the near future • lots on therapeutic hypothermia • hypothermia for space flight / hibernation • potential therapeutic hypothermia in trauma, “suspended animation” • more studies on endovascular rewarming catheters • more miraculous case reports back to our case • • • • • • • invasive core warming was thought to be indicated IV fluids, heated ventilation and forced air were not effective warm pleural lavage considered, CV surgery consulted for CPB endovascular catheter was used instead normothermia was achieved 5 hours later in ICU good hemodynamic recovery but minimal neurologic recovery family requested comfort care, patient died day 8 Laniewicz M. Rapid endovascular warming for profound hypothermia. Annals of Emer Med. 2008; 51:2 Conclusion In severe and profound hypothermia, details regarding CPR, defibrillation, medications, and other interventions may be less important than the provision of appropriate, effective rewarming • • • • • • • • Pearls important numbers: <36C dynamic phase of hypothermia, 32C critical temp for trauma patients, 32C can establish warm and dead, <30C patient is in trouble, >30C where ACLS algorithm changes afterdrop: be aware of it, reevaluate patients often, expect ↓T, +/clinical deterioration, rewarm the core first cold diuresis: AH patient is dry, give volume coagulopathy: normal INR/PPT does not reflect coagulopathic state. treatment is rewarming - not clotting factors. elevated INR/PTT in trauma deserves treatment with FFP and cryo beware the K: ↓T can ↑hyperkalemic cardiac toxicity. ECG may not show ↑K changes. Glucose: treat low glu. do not treat high glu. ECG: anything is possible. don’t confuse J waves for ↑ST ABG: don’t correct for temperature. just run it. target ph 7.4 pCO2 40 • • • • • • • • • Pearls no pulse: if in the field - long pulse check (up to 3min), give O2, if still no pulse - do CPR. In the ED - use ECG or U/S to establish presence of organized rhythm. If organized, No CPR despite no pulse contraindications to CPR: non compressible chest, ice in airway, decapitation or other injury incompatible with life, unsafe conditions for rescuers, signs of life pre hospital rewarming: passive rewarming for everyone. if in cardiac arrest - don’t rewarm until CPB. everyone else - safe to rewarm, target core, watch for afterdrop intubation: indications identical to normothermic patient. its safe...proceed if needed. ventilate at half normal rates repeat defib: consider giving repeat defib x 1 for every 1C rise of core temp despite being <30C resus meds: evidence is lacking: a few case reports and animal models. consider giving epi or amiodarone despite core temp being <30C. reduce frequency. bertyllium or procainimide not recommended adjunctinve therapy: empiric antibiotics, bicarb, steroids do not improve outcomes OG/NG - no evidence. conflicting opinion if safe or not. concern is irritating myocardium bradycardia: No CPR if pulse/heart movement, regardless of HR or BP. Pacing not recommended but transcutaneous may be safe and could improve CO. Intravenous pacing contraindicated • • • Pearls withhold resus: must be in cardiac arrest. Decapitation, evisceration or other injuries not in keeping with life. Consider if multi trauma patient with temp <32C or asphyxiated patient (definitive history) with K>10 prognostication: there are no validated prognostic indicators of the potential for recovery from acute severe hypothermia. Time submerged, age of patient, number of hours CPR, initial temperature, physical exam are all unreliable. K>10 has been suggested to indicated death prior to cooling. (warning: it could be elevated due to depolarizing NMB) stop resus: the only definite criterion of death is failure to respond to resuscitation and rewarming. If initiated resus, should strive to warm to 32C to establish death • • • • • • • Pearls hemodynamics: primary determinant of treatment modality, urgency of rewarming, and rewarming rate hemodynamic stable and mild ↓temp: passive external rewarming +/- bair hugger and IV cardiac arrest: level 1 trauma. transport to FMC. preferred treatment is CPB. consult CV surgery. back up method is thorasic lavage (open or closed). consider underlying disease, comorbidities, and likelihood of meaningful recover before initiating invasive/heroic measures hemodynamic stable and severe↓temp: treatment is debatable. No urgency. Go with least invasive, most familiar, and available unstable and mod/severe↓temp: treatment is debatable. Some urgency. Consult ICU/Trauma for possible extracorporeal rewarming. Go with least invasive, most familiar, and available. likely CRRT for most endovascular rewarming catheter: effective, easy to use, minimal complications, portable, rewarms throughout entire resus and work up (CT, angio, OR). minimal literature. expect more in the future optimal rewarming rate: no evidence. experts recommend if perfusing 1-2ºC per hour. If cardiac arrest, fast as possible, >2ºC per hour Pearls • look for hypothermia: can occur without cold exposure (ie • • • • DKA, MI, Sepsis) and is even found in warm situations (marathon runners) remember the physiology: bradycardia or coma when core >30C is abnormal. Tachycardia when core <32C is abnormal. seek other diseases entities to explain findings find the other problem: elderly patient usually becomes hypothermic because of another condition. find and treat this precipitating condition (often sepsis) in parallel with hypothermia landmark studies: Walpoth. Outcome of Survivors of Accidental Deep Hypothermia and circulatory arrest treated with extracorporeal blood warming. NJEM. 1997; 337:15005 good review:Gardner. Accidental hypothermia. Emergency medicine reports. 2009;30 Questions? Big THANKS to Dr. Gavin Greenfield Dr. Andy Kirkpatrick Dr. Bronwyn Kotyk Dr. Jason Lord Dr. Kyle McLaughlin